Qinghao Zhao
Aortic Valve Disease Detection from PPG via Physiology-Informed Self-Supervised Learning
Feb 04, 2026Abstract:Traditional diagnosis of aortic valve disease relies on echocardiography, but its cost and required expertise limit its use in large-scale early screening. Photoplethysmography (PPG) has emerged as a promising screening modality due to its widespread availability in wearable devices and its ability to reflect underlying hemodynamic dynamics. However, the extreme scarcity of gold-standard labeled PPG data severely constrains the effectiveness of data-driven approaches. To address this challenge, we propose and validate a new paradigm, Physiology-Guided Self-Supervised Learning (PG-SSL), aimed at unlocking the value of large-scale unlabeled PPG data for efficient screening of Aortic Stenosis (AS) and Aortic Regurgitation (AR). Using over 170,000 unlabeled PPG samples from the UK Biobank, we formalize clinical knowledge into a set of PPG morphological phenotypes and construct a pulse pattern recognition proxy task for self-supervised pre-training. A dual-branch, gated-fusion architecture is then employed for efficient fine-tuning on a small labeled subset. The proposed PG-SSL framework achieves AUCs of 0.765 and 0.776 for AS and AR screening, respectively, significantly outperforming supervised baselines trained on limited labeled data. Multivariable analysis further validates the model output as an independent digital biomarker with sustained prognostic value after adjustment for standard clinical risk factors. This study demonstrates that PG-SSL provides an effective, domain knowledge-driven solution to label scarcity in medical artificial intelligence and shows strong potential for enabling low-cost, large-scale early screening of aortic valve disease.
AnyECG: Evolved ECG Foundation Model for Holistic Health Profiling
Jan 12, 2026Abstract:Background: Artificial intelligence enabled electrocardiography (AI-ECG) has demonstrated the ability to detect diverse pathologies, but most existing models focus on single disease identification, neglecting comorbidities and future risk prediction. Although ECGFounder expanded cardiac disease coverage, a holistic health profiling model remains needed. Methods: We constructed a large multicenter dataset comprising 13.3 million ECGs from 2.98 million patients. Using transfer learning, ECGFounder was fine-tuned to develop AnyECG, a foundation model for holistic health profiling. Performance was evaluated using external validation cohorts and a 10-year longitudinal cohort for current diagnosis, future risk prediction, and comorbidity identification. Results: AnyECG demonstrated systemic predictive capability across 1172 conditions, achieving an AUROC greater than 0.7 for 306 diseases. The model revealed novel disease associations, robust comorbidity patterns, and future disease risks. Representative examples included high diagnostic performance for hyperparathyroidism (AUROC 0.941), type 2 diabetes (0.803), Crohn disease (0.817), lymphoid leukemia (0.856), and chronic obstructive pulmonary disease (0.773). Conclusion: The AnyECG foundation model provides substantial evidence that AI-ECG can serve as a systemic tool for concurrent disease detection and long-term risk prediction.
Artificial Intelligence-Enabled Spirometry for Early Detection of Right Heart Failure
Nov 17, 2025Abstract:Right heart failure (RHF) is a disease characterized by abnormalities in the structure or function of the right ventricle (RV), which is associated with high morbidity and mortality. Lung disease often causes increased right ventricular load, leading to RHF. Therefore, it is very important to screen out patients with cor pulmonale who develop RHF from people with underlying lung diseases. In this work, we propose a self-supervised representation learning method to early detecting RHF from patients with cor pulmonale, which uses spirogram time series to predict patients with RHF at an early stage. The proposed model is divided into two stages. The first stage is the self-supervised representation learning-based spirogram embedding (SLSE) network training process, where the encoder of the Variational autoencoder (VAE-encoder) learns a robust low-dimensional representation of the spirogram time series from the data-augmented unlabeled data. Second, this low-dimensional representation is fused with demographic information and fed into a CatBoost classifier for the downstream RHF prediction task. Trained and tested on a carefully selected subset of 26,617 individuals from the UK Biobank, our model achieved an AUROC of 0.7501 in detecting RHF, demonstrating strong population-level distinction ability. We further evaluated the model on high-risk clinical subgroups, achieving AUROC values of 0.8194 on a test set of 74 patients with chronic kidney disease (CKD) and 0.8413 on a set of 64 patients with valvular heart disease (VHD). These results highlight the model's potential utility in predicting RHF among clinically elevated-risk populations. In conclusion, this study presents a self-supervised representation learning approach combining spirogram time series and demographic data, demonstrating promising potential for early RHF detection in clinical practice.
AnyECG-Lab: An Exploration Study of Fine-tuning an ECG Foundation Model to Estimate Laboratory Values from Single-Lead ECG Signals
Oct 25, 2025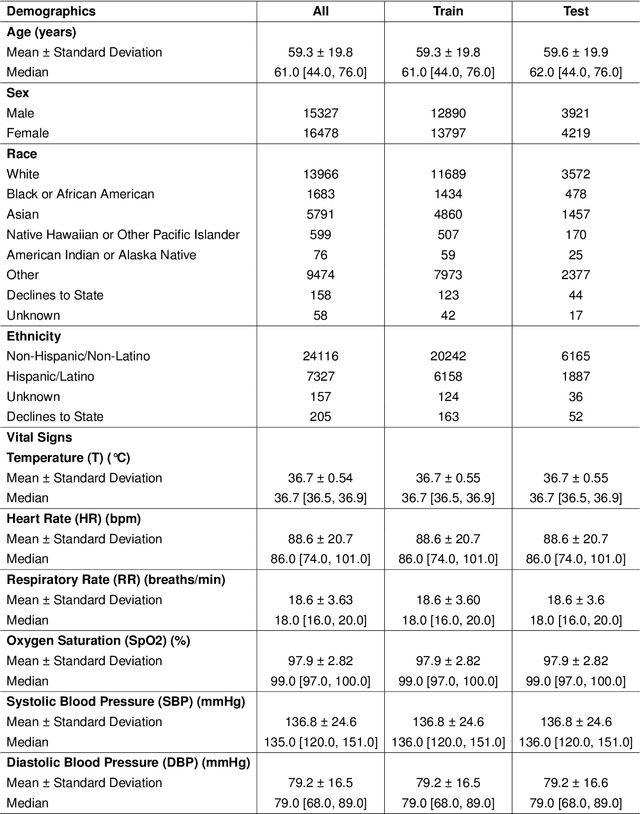
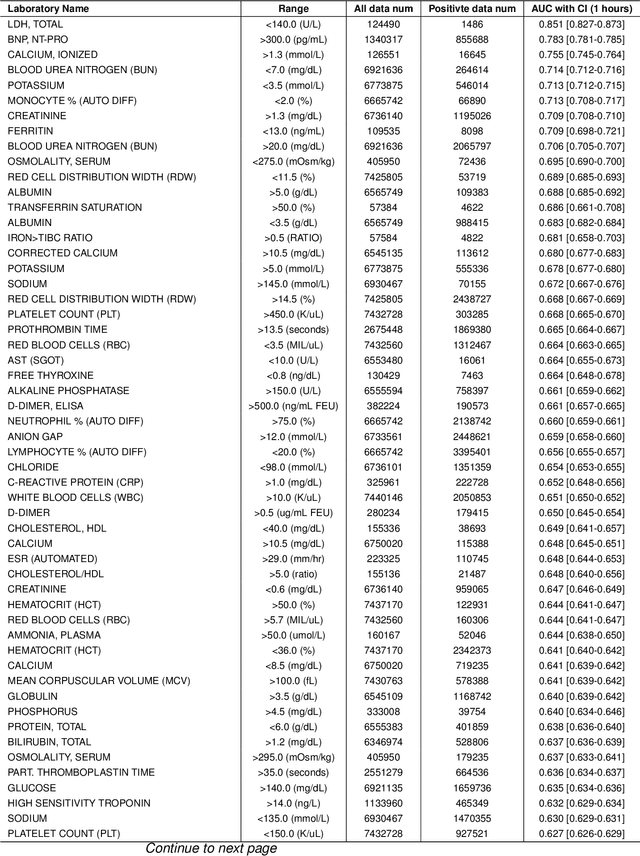
Abstract:Timely access to laboratory values is critical for clinical decision-making, yet current approaches rely on invasive venous sampling and are intrinsically delayed. Electrocardiography (ECG), as a non-invasive and widely available signal, offers a promising modality for rapid laboratory estimation. Recent progress in deep learning has enabled the extraction of latent hematological signatures from ECGs. However, existing models are constrained by low signal-to-noise ratios, substantial inter-individual variability, limited data diversity, and suboptimal generalization, especially when adapted to low-lead wearable devices. In this work, we conduct an exploratory study leveraging transfer learning to fine-tune ECGFounder, a large-scale pre-trained ECG foundation model, on the Multimodal Clinical Monitoring in the Emergency Department (MC-MED) dataset from Stanford. We generated a corpus of more than 20 million standardized ten-second ECG segments to enhance sensitivity to subtle biochemical correlates. On internal validation, the model demonstrated strong predictive performance (area under the curve above 0.65) for thirty-three laboratory indicators, moderate performance (between 0.55 and 0.65) for fifty-nine indicators, and limited performance (below 0.55) for sixteen indicators. This study provides an efficient artificial-intelligence driven solution and establishes the feasibility scope for real-time, non-invasive estimation of laboratory values.
GEM: Empowering MLLM for Grounded ECG Understanding with Time Series and Images
Mar 08, 2025Abstract:While recent multimodal large language models (MLLMs) have advanced automated ECG interpretation, they still face two key limitations: (1) insufficient multimodal synergy between time series signals and visual ECG representations, and (2) limited explainability in linking diagnoses to granular waveform evidence. We introduce GEM, the first MLLM unifying ECG time series, 12-lead ECG images and text for grounded and clinician-aligned ECG interpretation. GEM enables feature-grounded analysis, evidence-driven reasoning, and a clinician-like diagnostic process through three core innovations: a dual-encoder framework extracting complementary time series and image features, cross-modal alignment for effective multimodal understanding, and knowledge-guided instruction generation for generating high-granularity grounding data (ECG-Grounding) linking diagnoses to measurable parameters ($e.g.$, QRS/PR Intervals). Additionally, we propose the Grounded ECG Understanding task, a clinically motivated benchmark designed to comprehensively assess the MLLM's capability in grounded ECG understanding. Experimental results on both existing and our proposed benchmarks show GEM significantly improves predictive performance (CSN $7.4\% \uparrow$), explainability ($22.7\% \uparrow$), and grounding ($24.8\% \uparrow$), making it more suitable for real-world clinical applications. GitHub repository: https://github.com/lanxiang1017/GEM.git
Accuracy of Wearable ECG Parameter Calculation Method for Long QT and First-Degree A-V Block Detection: A Multi-Center Real-World Study with External Validations Compared to Standard ECG Machines and Cardiologist Assessments
Feb 21, 2025Abstract:In recent years, wearable devices have revolutionized cardiac monitoring by enabling continuous, non-invasive ECG recording in real-world settings. Despite these advances, the accuracy of ECG parameter calculations (PR interval, QRS interval, QT interval, etc.) from wearables remains to be rigorously validated against conventional ECG machines and expert clinician assessments. In this large-scale, multicenter study, we evaluated FeatureDB, a novel algorithm for automated computation of ECG parameters from wearable single-lead signals Three diverse datasets were employed: the AHMU-FH dataset (n=88,874), the CSE dataset (n=106), and the HeartVoice-ECG-lite dataset (n=369) with annotations provided by two experienced cardiologists. FeatureDB demonstrates a statistically significant correlation with key parameters (PR interval, QRS duration, QT interval, and QTc) calculated by standard ECG machines and annotated by clinical doctors. Bland-Altman analysis confirms a high level of agreement.Moreover,FeatureDB exhibited robust diagnostic performance in detecting Long QT syndrome (LQT) and atrioventricular block interval abnormalities (AVBI),with excellent area under the ROC curve (LQT: 0.836, AVBI: 0.861),accuracy (LQT: 0.856, AVBI: 0.845),sensitivity (LQT: 0.815, AVBI: 0.877),and specificity (LQT: 0.856, AVBI: 0.845).This further validates its clinical reliability. These results validate the clinical applicability of FeatureDB for wearable ECG analysis and highlight its potential to bridge the gap between traditional diagnostic methods and emerging wearable technologies.Ultimately,this study supports integrating wearable ECG devices into large-scale cardiovascular disease management and early intervention strategies,and it highlights the potential of wearable ECG technologies to deliver accurate,clinically relevant cardiac monitoring while advancing broader applications in cardiovascular care.
Artificial Intelligence-derived Vascular Age from Photoplethysmography: A Novel Digital Biomarker for Cardiovascular Health
Feb 19, 2025Abstract:With the increasing availability of wearable devices, photoplethysmography (PPG) has emerged as a promising non-invasive tool for monitoring human hemodynamics. We propose a deep learning framework to estimate vascular age (AI-vascular age) from PPG signals, incorporating a distribution-aware loss to address biases caused by imbalanced data. The model was developed using data from the UK Biobank (UKB), with 98,672 participants in the development cohort and 113,559 participants (144,683 data pairs) for clinical evaluation. After adjusting for key confounders, individuals with a vascular age gap (AI-vascular age minus calendar age) exceeding 9 years had a significantly higher risk of major adverse cardiovascular and cerebrovascular events (MACCE) (HR = 2.37, p < 0.005) and secondary outcomes, including diabetes (HR = 2.69, p < 0.005), hypertension (HR = 2.88, p < 0.005), coronary heart disease (HR = 2.20, p < 0.005), heart failure (HR = 2.15, p < 0.005), myocardial infarction (HR = 2.51, p < 0.005), stroke (HR = 2.55, p < 0.005), and all-cause mortality (HR = 2.51, p < 0.005). Conversely, participants with a vascular age gap below -9 years exhibited a significantly lower incidence of these outcomes. We further evaluated the longitudinal applicability of AI-vascular age using serial PPG data from the UKB, demonstrating its value in risk stratification by leveraging AI-vascular age at two distinct time points to predict future MACCE incidence. External validation was performed on a MIMIC-III-derived cohort (n = 2,343), where each one-year increase in vascular age gap was significantly associated with elevated in-hospital mortality risk (OR = 1.02, p < 0.005). In conclusion, our study establishes AI-vascular age as a novel, non-invasive digital biomarker for cardiovascular health assessment.
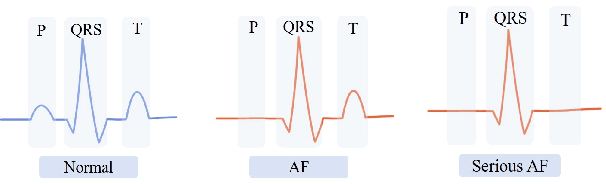
Deep Imbalanced Regression to Estimate Vascular Age from PPG Data: a Novel Digital Biomarker for Cardiovascular Health
Jun 21, 2024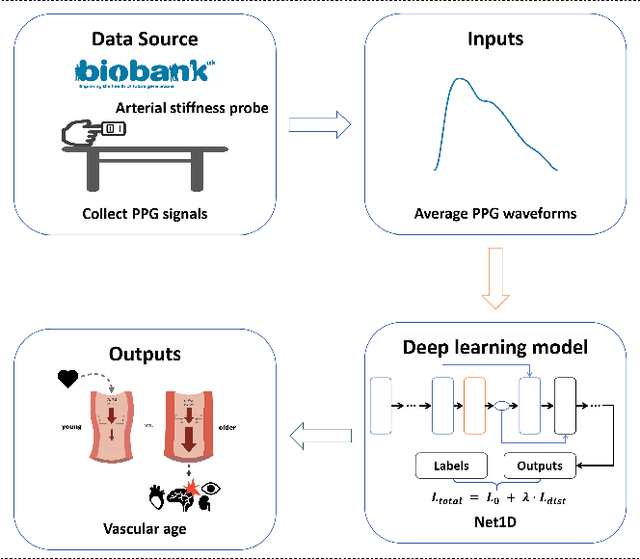
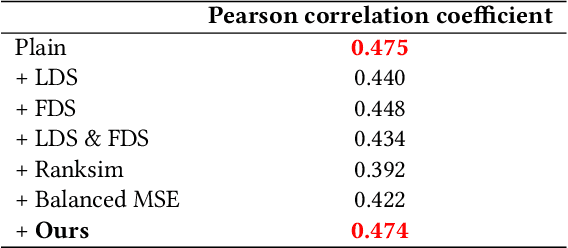
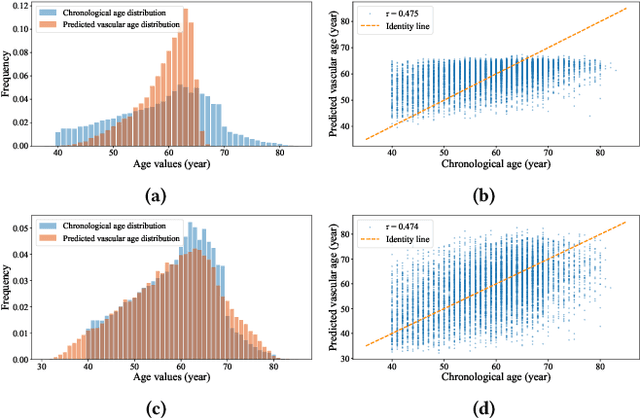
Abstract:Photoplethysmography (PPG) is emerging as a crucial tool for monitoring human hemodynamics, with recent studies highlighting its potential in assessing vascular aging through deep learning. However, real-world age distributions are often imbalanced, posing significant challenges for deep learning models. In this paper, we introduce a novel, simple, and effective loss function named the Dist Loss to address deep imbalanced regression tasks. We trained a one-dimensional convolutional neural network (Net1D) incorporating the Dist Loss on the extensive UK Biobank dataset (n=502,389) to estimate vascular age from PPG signals and validate its efficacy in characterizing cardiovascular health. The model's performance was validated on a 40% held-out test set, achieving state-of-the-art results, especially in regions with small sample sizes. Furthermore, we divided the population into three subgroups based on the difference between predicted vascular age and chronological age: less than -10 years, between -10 and 10 years, and greater than 10 years. We analyzed the relationship between predicted vascular age and several cardiovascular events over a follow-up period of up to 10 years, including death, coronary heart disease, and heart failure. Our results indicate that the predicted vascular age has significant potential to reflect an individual's cardiovascular health status. Our code will be available at https://github.com/Ngk03/AI-vascular-age.
Deep Learning for Detecting and Early Predicting Chronic Obstructive Pulmonary Disease from Spirogram Time Series: A UK Biobank Study
May 06, 2024



Abstract:Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung condition that causes airflow obstruction. The existing methods can only detect patients who already have COPD based on obvious features shown in the spirogram (In this article, the spirogram specifically involves measuring Volume-Flow curve time series). Early prediction of COPD risk is vital for monitoring COPD disease progression, slowing it down, or even preventing its onset. However, these methods fail to early predict an individual's probability of COPD in the future based on subtle features in the spirogram. To address this gap, for the first time, we propose DeepSpiro, a method based on deep learning for early prediction of future COPD risk. DeepSpiro consists of four parts. First, we construct Volume-Flow curves guided by Time-Volume instability smoothing (SpiroSmoother) to enhance the stability of the original Volume-Flow curves precisely. Second, we extract critical features from the evolution of varied-length key patches (SpiroEncoder) to capture the key temporal evolution from original high-dimensional dynamic sequences to a unified low-dimensional temporal representation. Third, we explain the model based on temporal attention and heterogeneous feature fusion (SpiroExplainer), which integrates information from heterogeneous data such as spirogram and demographic information. Fourth, we predict the risk of COPD based on the evolution of key patch concavity (SpiroPredictor), enabling accurate prediction of the risk of disease in high-risk patients who are not yet diagnosed, for up to 1, 2, 3, 4, 5 years, and beyond. We conduct experiments on the UK Biobank dataset. Results show that DeepSpiro achieves an AUC value of 0.8328 in the task of detecting COPD. In early prediction tasks, high-risk and low-risk groups show significant differences in the future, with a p-value of <0.001.
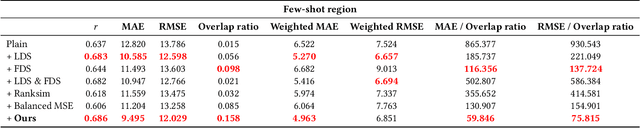
A Deep Learning Method for Beat-Level Risk Analysis and Interpretation of Atrial Fibrillation Patients during Sinus Rhythm
Mar 18, 2024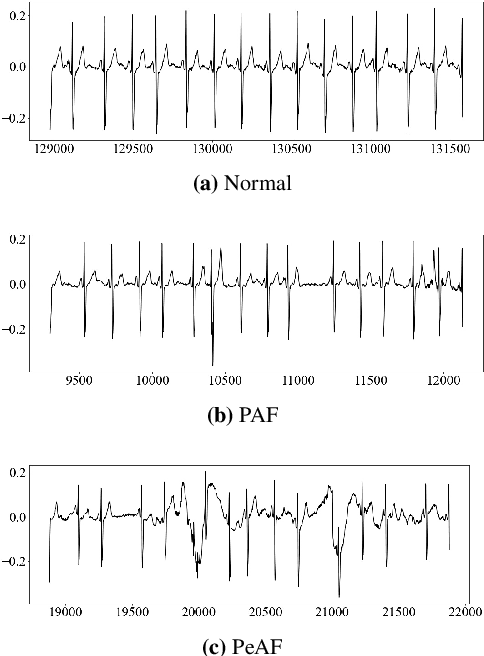

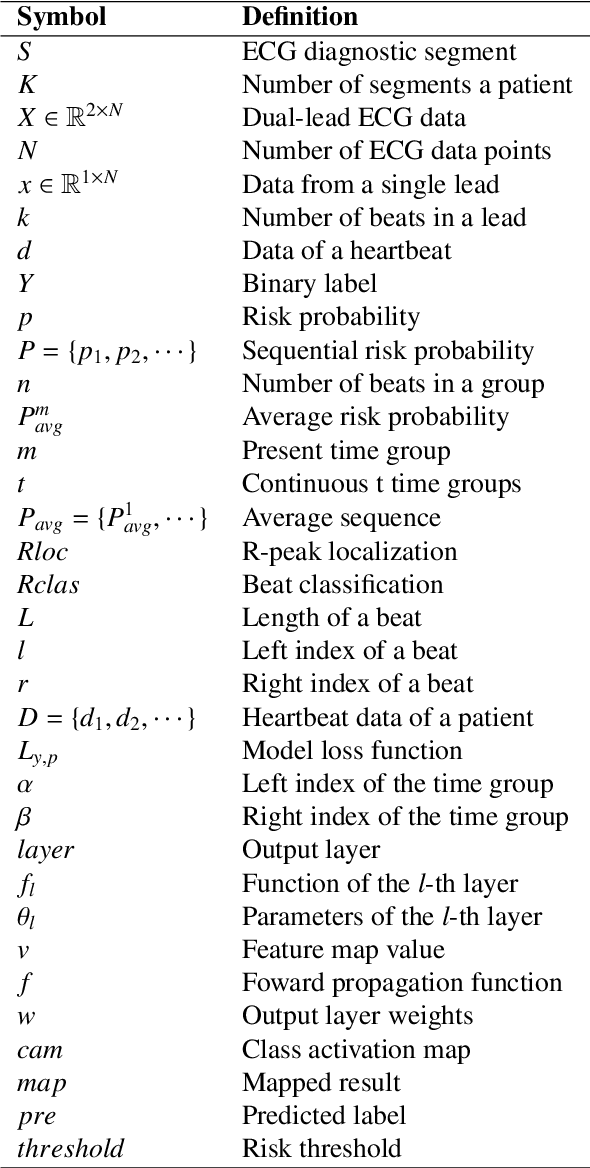
Abstract:Atrial Fibrillation (AF) is a common cardiac arrhythmia. Many AF patients experience complications such as stroke and other cardiovascular issues. Early detection of AF is crucial. Existing algorithms can only distinguish ``AF rhythm in AF patients'' from ``sinus rhythm in normal individuals'' . However, AF patients do not always exhibit AF rhythm, posing a challenge for diagnosis when the AF rhythm is absent. To address this, this paper proposes a novel artificial intelligence (AI) algorithm to distinguish ``sinus rhythm in AF patients'' and ``sinus rhythm in normal individuals'' in beat-level. We introduce beat-level risk interpreters, trend risk interpreters, addressing the interpretability issues of deep learning models and the difficulty in explaining AF risk trends. Additionally, the beat-level information fusion decision is presented to enhance model accuracy. The experimental results demonstrate that the average AUC for single beats used as testing data from CPSC 2021 dataset is 0.7314. By employing 150 beats for information fusion decision algorithm, the average AUC can reach 0.7591. Compared to previous segment-level algorithms, we utilized beats as input, reducing data dimensionality and making the model more lightweight, facilitating deployment on portable medical devices. Furthermore, we draw new and interesting findings through average beat analysis and subgroup analysis, considering varying risk levels.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge