Lance Downing
MedHELM: Holistic Evaluation of Large Language Models for Medical Tasks
May 26, 2025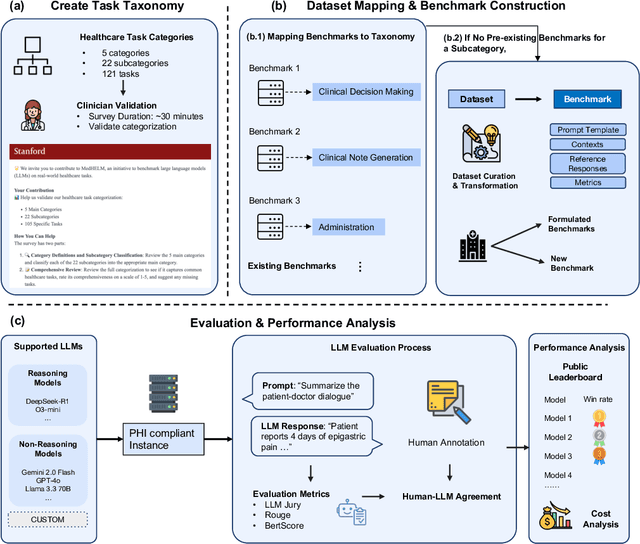
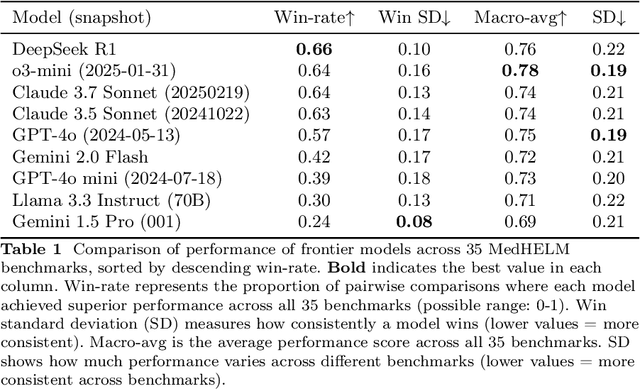
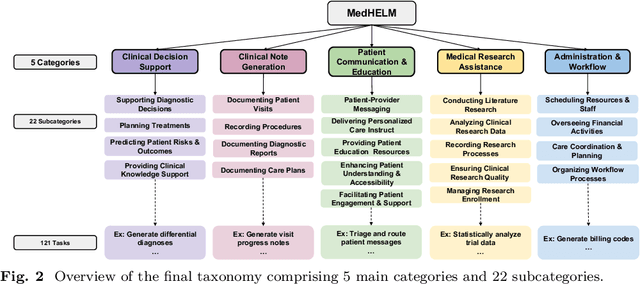
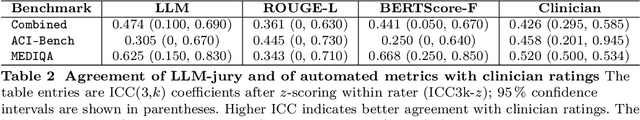
Abstract:While large language models (LLMs) achieve near-perfect scores on medical licensing exams, these evaluations inadequately reflect the complexity and diversity of real-world clinical practice. We introduce MedHELM, an extensible evaluation framework for assessing LLM performance for medical tasks with three key contributions. First, a clinician-validated taxonomy spanning 5 categories, 22 subcategories, and 121 tasks developed with 29 clinicians. Second, a comprehensive benchmark suite comprising 35 benchmarks (17 existing, 18 newly formulated) providing complete coverage of all categories and subcategories in the taxonomy. Third, a systematic comparison of LLMs with improved evaluation methods (using an LLM-jury) and a cost-performance analysis. Evaluation of 9 frontier LLMs, using the 35 benchmarks, revealed significant performance variation. Advanced reasoning models (DeepSeek R1: 66% win-rate; o3-mini: 64% win-rate) demonstrated superior performance, though Claude 3.5 Sonnet achieved comparable results at 40% lower estimated computational cost. On a normalized accuracy scale (0-1), most models performed strongly in Clinical Note Generation (0.73-0.85) and Patient Communication & Education (0.78-0.83), moderately in Medical Research Assistance (0.65-0.75), and generally lower in Clinical Decision Support (0.56-0.72) and Administration & Workflow (0.53-0.63). Our LLM-jury evaluation method achieved good agreement with clinician ratings (ICC = 0.47), surpassing both average clinician-clinician agreement (ICC = 0.43) and automated baselines including ROUGE-L (0.36) and BERTScore-F1 (0.44). Claude 3.5 Sonnet achieved comparable performance to top models at lower estimated cost. These findings highlight the importance of real-world, task-specific evaluation for medical use of LLMs and provides an open source framework to enable this.
Evaluation of GPT-3.5 and GPT-4 for supporting real-world information needs in healthcare delivery
May 01, 2023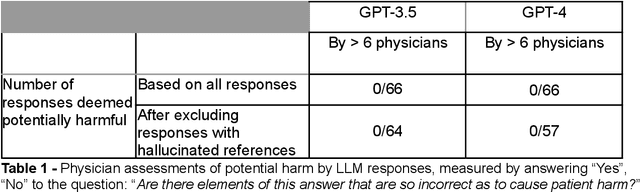
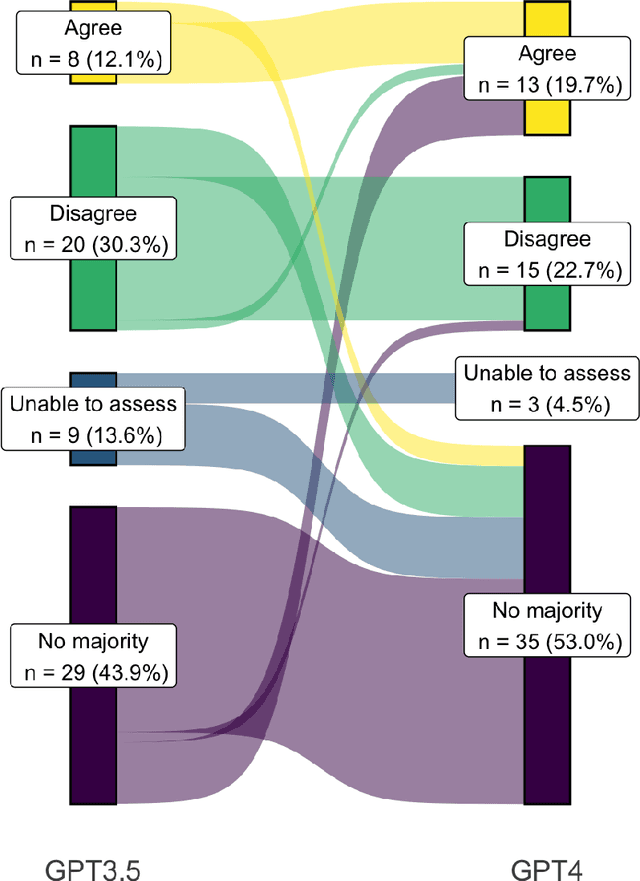
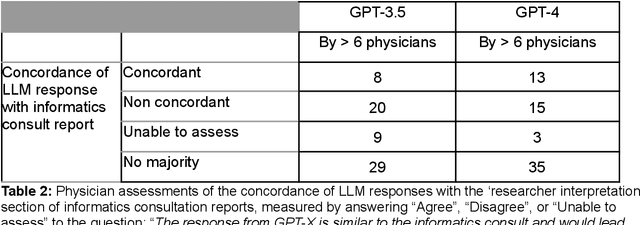
Abstract:Despite growing interest in using large language models (LLMs) in healthcare, current explorations do not assess the real-world utility and safety of LLMs in clinical settings. Our objective was to determine whether two LLMs can serve information needs submitted by physicians as questions to an informatics consultation service in a safe and concordant manner. Sixty six questions from an informatics consult service were submitted to GPT-3.5 and GPT-4 via simple prompts. 12 physicians assessed the LLM responses' possibility of patient harm and concordance with existing reports from an informatics consultation service. Physician assessments were summarized based on majority vote. For no questions did a majority of physicians deem either LLM response as harmful. For GPT-3.5, responses to 8 questions were concordant with the informatics consult report, 20 discordant, and 9 were unable to be assessed. There were 29 responses with no majority on "Agree", "Disagree", and "Unable to assess". For GPT-4, responses to 13 questions were concordant, 15 discordant, and 3 were unable to be assessed. There were 35 responses with no majority. Responses from both LLMs were largely devoid of overt harm, but less than 20% of the responses agreed with an answer from an informatics consultation service, responses contained hallucinated references, and physicians were divided on what constitutes harm. These results suggest that while general purpose LLMs are able to provide safe and credible responses, they often do not meet the specific information need of a given question. A definitive evaluation of the usefulness of LLMs in healthcare settings will likely require additional research on prompt engineering, calibration, and custom-tailoring of general purpose models.
Towards Vision-Based Smart Hospitals: A System for Tracking and Monitoring Hand Hygiene Compliance
Apr 24, 2018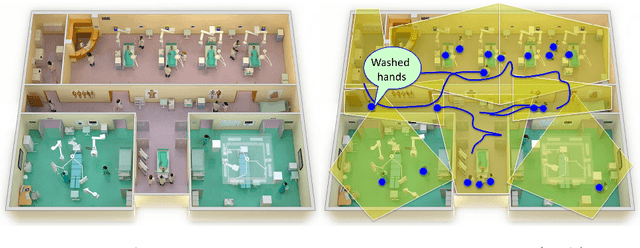
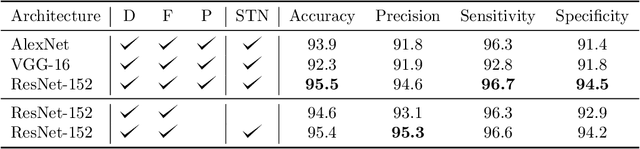


Abstract:One in twenty-five patients admitted to a hospital will suffer from a hospital acquired infection. If we can intelligently track healthcare staff, patients, and visitors, we can better understand the sources of such infections. We envision a smart hospital capable of increasing operational efficiency and improving patient care with less spending. In this paper, we propose a non-intrusive vision-based system for tracking people's activity in hospitals. We evaluate our method for the problem of measuring hand hygiene compliance. Empirically, our method outperforms existing solutions such as proximity-based techniques and covert in-person observational studies. We present intuitive, qualitative results that analyze human movement patterns and conduct spatial analytics which convey our method's interpretability. This work is a step towards a computer-vision based smart hospital and demonstrates promising results for reducing hospital acquired infections.
* Machine Learning for Healthcare Conference (MLHC)
Improving Palliative Care with Deep Learning
Nov 17, 2017



Abstract:Improving the quality of end-of-life care for hospitalized patients is a priority for healthcare organizations. Studies have shown that physicians tend to over-estimate prognoses, which in combination with treatment inertia results in a mismatch between patients wishes and actual care at the end of life. We describe a method to address this problem using Deep Learning and Electronic Health Record (EHR) data, which is currently being piloted, with Institutional Review Board approval, at an academic medical center. The EHR data of admitted patients are automatically evaluated by an algorithm, which brings patients who are likely to benefit from palliative care services to the attention of the Palliative Care team. The algorithm is a Deep Neural Network trained on the EHR data from previous years, to predict all-cause 3-12 month mortality of patients as a proxy for patients that could benefit from palliative care. Our predictions enable the Palliative Care team to take a proactive approach in reaching out to such patients, rather than relying on referrals from treating physicians, or conduct time consuming chart reviews of all patients. We also present a novel interpretation technique which we use to provide explanations of the model's predictions.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge