Ethan Goh
MedHELM: Holistic Evaluation of Large Language Models for Medical Tasks
May 26, 2025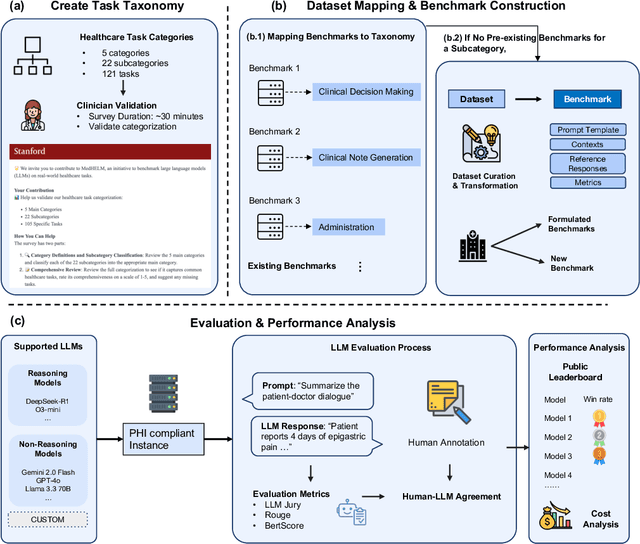
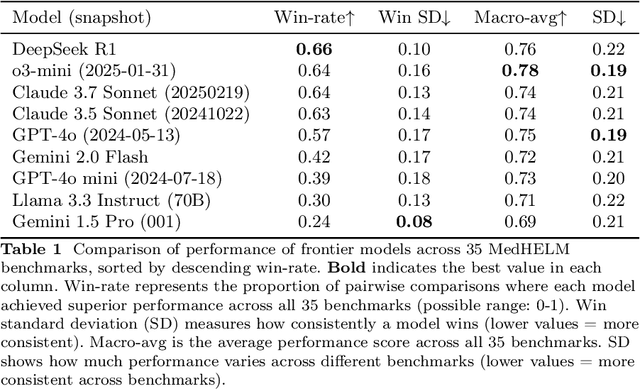
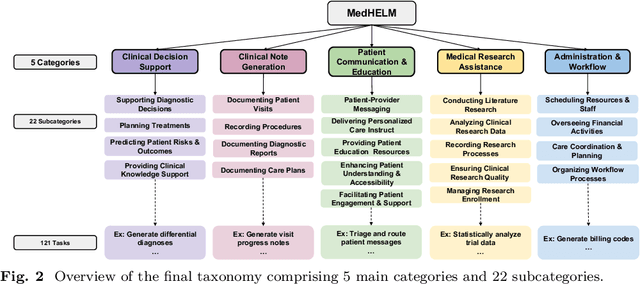
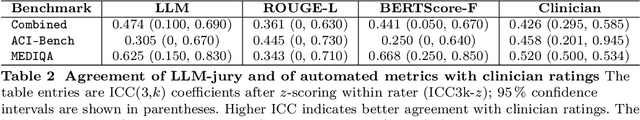
Abstract:While large language models (LLMs) achieve near-perfect scores on medical licensing exams, these evaluations inadequately reflect the complexity and diversity of real-world clinical practice. We introduce MedHELM, an extensible evaluation framework for assessing LLM performance for medical tasks with three key contributions. First, a clinician-validated taxonomy spanning 5 categories, 22 subcategories, and 121 tasks developed with 29 clinicians. Second, a comprehensive benchmark suite comprising 35 benchmarks (17 existing, 18 newly formulated) providing complete coverage of all categories and subcategories in the taxonomy. Third, a systematic comparison of LLMs with improved evaluation methods (using an LLM-jury) and a cost-performance analysis. Evaluation of 9 frontier LLMs, using the 35 benchmarks, revealed significant performance variation. Advanced reasoning models (DeepSeek R1: 66% win-rate; o3-mini: 64% win-rate) demonstrated superior performance, though Claude 3.5 Sonnet achieved comparable results at 40% lower estimated computational cost. On a normalized accuracy scale (0-1), most models performed strongly in Clinical Note Generation (0.73-0.85) and Patient Communication & Education (0.78-0.83), moderately in Medical Research Assistance (0.65-0.75), and generally lower in Clinical Decision Support (0.56-0.72) and Administration & Workflow (0.53-0.63). Our LLM-jury evaluation method achieved good agreement with clinician ratings (ICC = 0.47), surpassing both average clinician-clinician agreement (ICC = 0.43) and automated baselines including ROUGE-L (0.36) and BERTScore-F1 (0.44). Claude 3.5 Sonnet achieved comparable performance to top models at lower estimated cost. These findings highlight the importance of real-world, task-specific evaluation for medical use of LLMs and provides an open source framework to enable this.
Superhuman performance of a large language model on the reasoning tasks of a physician
Dec 14, 2024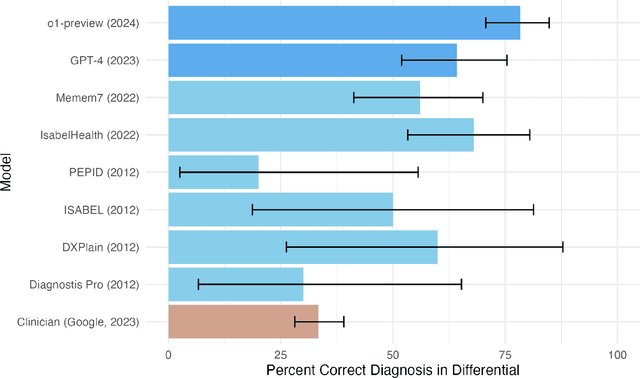
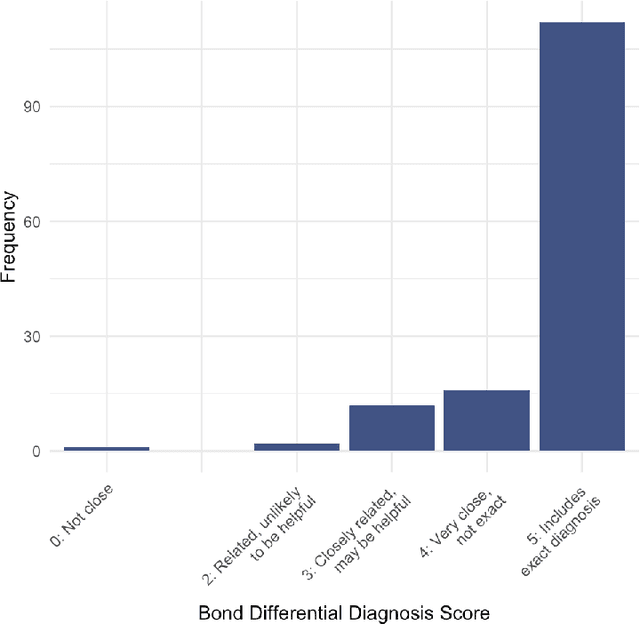
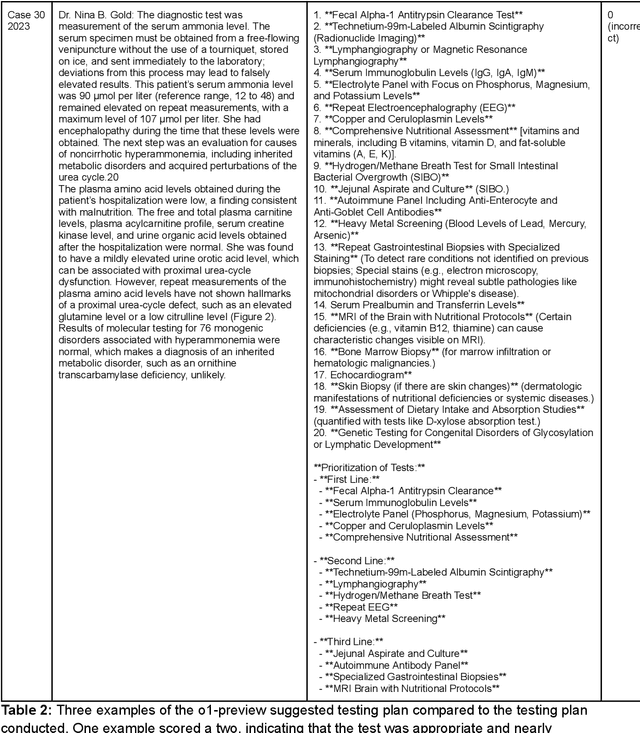
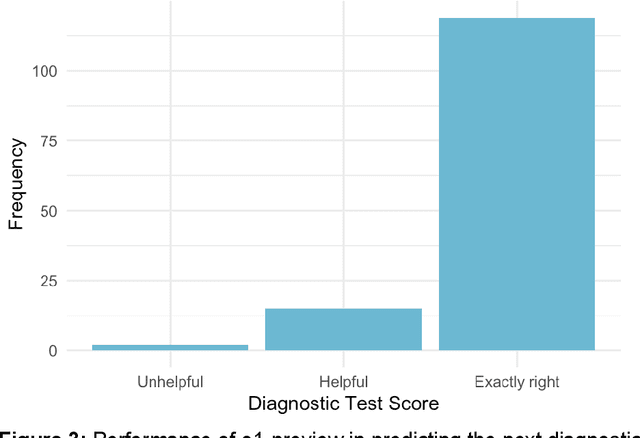
Abstract:Performance of large language models (LLMs) on medical tasks has traditionally been evaluated using multiple choice question benchmarks. However, such benchmarks are highly constrained, saturated with repeated impressive performance by LLMs, and have an unclear relationship to performance in real clinical scenarios. Clinical reasoning, the process by which physicians employ critical thinking to gather and synthesize clinical data to diagnose and manage medical problems, remains an attractive benchmark for model performance. Prior LLMs have shown promise in outperforming clinicians in routine and complex diagnostic scenarios. We sought to evaluate OpenAI's o1-preview model, a model developed to increase run-time via chain of thought processes prior to generating a response. We characterize the performance of o1-preview with five experiments including differential diagnosis generation, display of diagnostic reasoning, triage differential diagnosis, probabilistic reasoning, and management reasoning, adjudicated by physician experts with validated psychometrics. Our primary outcome was comparison of the o1-preview output to identical prior experiments that have historical human controls and benchmarks of previous LLMs. Significant improvements were observed with differential diagnosis generation and quality of diagnostic and management reasoning. No improvements were observed with probabilistic reasoning or triage differential diagnosis. This study highlights o1-preview's ability to perform strongly on tasks that require complex critical thinking such as diagnosis and management while its performance on probabilistic reasoning tasks was similar to past models. New robust benchmarks and scalable evaluation of LLM capabilities compared to human physicians are needed along with trials evaluating AI in real clinical settings.
MedAlign: A Clinician-Generated Dataset for Instruction Following with Electronic Medical Records
Aug 27, 2023
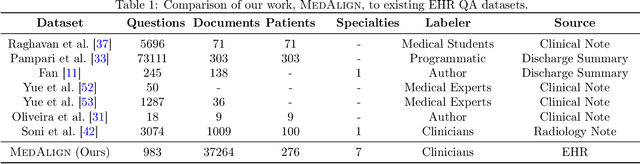
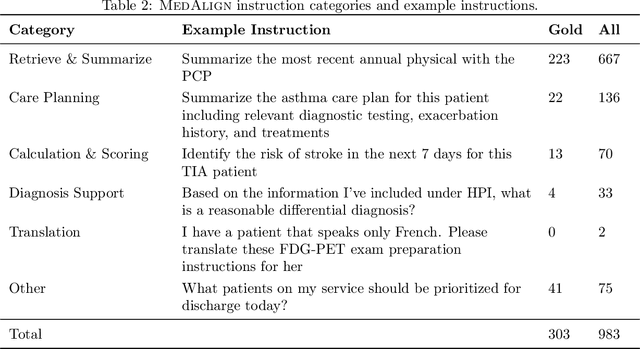

Abstract:The ability of large language models (LLMs) to follow natural language instructions with human-level fluency suggests many opportunities in healthcare to reduce administrative burden and improve quality of care. However, evaluating LLMs on realistic text generation tasks for healthcare remains challenging. Existing question answering datasets for electronic health record (EHR) data fail to capture the complexity of information needs and documentation burdens experienced by clinicians. To address these challenges, we introduce MedAlign, a benchmark dataset of 983 natural language instructions for EHR data. MedAlign is curated by 15 clinicians (7 specialities), includes clinician-written reference responses for 303 instructions, and provides 276 longitudinal EHRs for grounding instruction-response pairs. We used MedAlign to evaluate 6 general domain LLMs, having clinicians rank the accuracy and quality of each LLM response. We found high error rates, ranging from 35% (GPT-4) to 68% (MPT-7B-Instruct), and an 8.3% drop in accuracy moving from 32k to 2k context lengths for GPT-4. Finally, we report correlations between clinician rankings and automated natural language generation metrics as a way to rank LLMs without human review. We make MedAlign available under a research data use agreement to enable LLM evaluations on tasks aligned with clinician needs and preferences.
Evaluation of GPT-3.5 and GPT-4 for supporting real-world information needs in healthcare delivery
May 01, 2023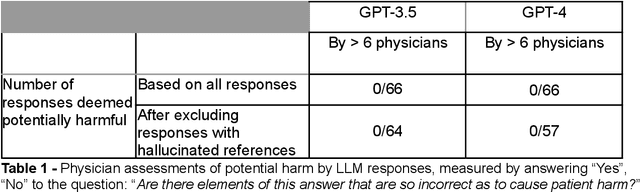
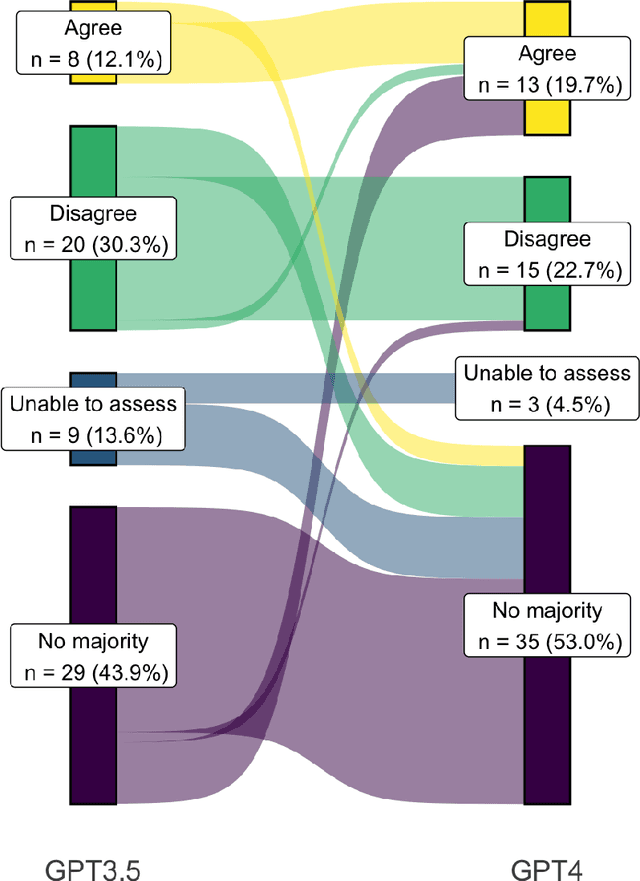
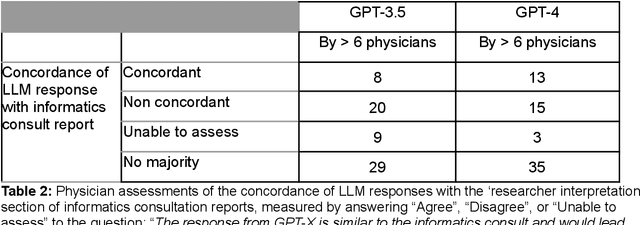
Abstract:Despite growing interest in using large language models (LLMs) in healthcare, current explorations do not assess the real-world utility and safety of LLMs in clinical settings. Our objective was to determine whether two LLMs can serve information needs submitted by physicians as questions to an informatics consultation service in a safe and concordant manner. Sixty six questions from an informatics consult service were submitted to GPT-3.5 and GPT-4 via simple prompts. 12 physicians assessed the LLM responses' possibility of patient harm and concordance with existing reports from an informatics consultation service. Physician assessments were summarized based on majority vote. For no questions did a majority of physicians deem either LLM response as harmful. For GPT-3.5, responses to 8 questions were concordant with the informatics consult report, 20 discordant, and 9 were unable to be assessed. There were 29 responses with no majority on "Agree", "Disagree", and "Unable to assess". For GPT-4, responses to 13 questions were concordant, 15 discordant, and 3 were unable to be assessed. There were 35 responses with no majority. Responses from both LLMs were largely devoid of overt harm, but less than 20% of the responses agreed with an answer from an informatics consultation service, responses contained hallucinated references, and physicians were divided on what constitutes harm. These results suggest that while general purpose LLMs are able to provide safe and credible responses, they often do not meet the specific information need of a given question. A definitive evaluation of the usefulness of LLMs in healthcare settings will likely require additional research on prompt engineering, calibration, and custom-tailoring of general purpose models.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge