Norbert Strobel
ProPLIKS: Probablistic 3D human body pose estimation
Dec 05, 2024

Abstract:We present a novel approach for 3D human pose estimation by employing probabilistic modeling. This approach leverages the advantages of normalizing flows in non-Euclidean geometries to address uncertain poses. Specifically, our method employs normalizing flow tailored to the SO(3) rotational group, incorporating a coupling mechanism based on the M\"obius transformation. This enables the framework to accurately represent any distribution on SO(3), effectively addressing issues related to discontinuities. Additionally, we reinterpret the challenge of reconstructing 3D human figures from 2D pixel-aligned inputs as the task of mapping these inputs to a range of probable poses. This perspective acknowledges the intrinsic ambiguity of the task and facilitates a straightforward integration method for multi-view scenarios. The combination of these strategies showcases the effectiveness of probabilistic models in complex scenarios for human pose estimation techniques. Our approach notably surpasses existing methods in the field of pose estimation. We also validate our methodology on human pose estimation from RGB images as well as medical X-Ray datasets.
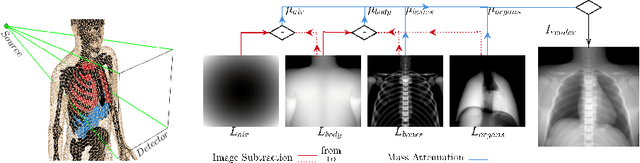
BOSS: Bones, Organs and Skin Shape Model
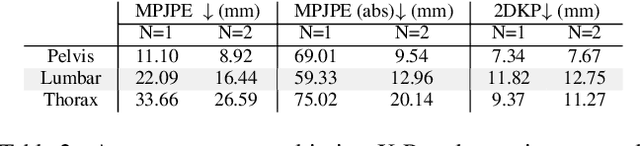
Mar 08, 2023Abstract:Objective: A digital twin of a patient can be a valuable tool for enhancing clinical tasks such as workflow automation, patient-specific X-ray dose optimization, markerless tracking, positioning, and navigation assistance in image-guided interventions. However, it is crucial that the patient's surface and internal organs are of high quality for any pose and shape estimates. At present, the majority of statistical shape models (SSMs) are restricted to a small number of organs or bones or do not adequately represent the general population. Method: To address this, we propose a deformable human shape and pose model that combines skin, internal organs, and bones, learned from CT images. By modeling the statistical variations in a pose-normalized space using probabilistic PCA while also preserving joint kinematics, our approach offers a holistic representation of the body that can benefit various medical applications. Results: We assessed our model's performance on a registered dataset, utilizing the unified shape space, and noted an average error of 3.6 mm for bones and 8.8 mm for organs. To further verify our findings, we conducted additional tests on publicly available datasets with multi-part segmentations, which confirmed the effectiveness of our model. Conclusion: This works shows that anatomically parameterized statistical shape models can be created accurately and in a computationally efficient manner. Significance: The proposed approach enables the construction of shape models that can be directly applied to various medical applications, including biomechanics and reconstruction.
PLIKS: A Pseudo-Linear Inverse Kinematic Solver for 3D Human Body Estimation
Nov 21, 2022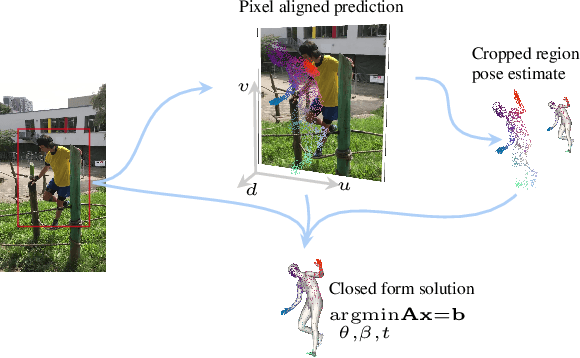
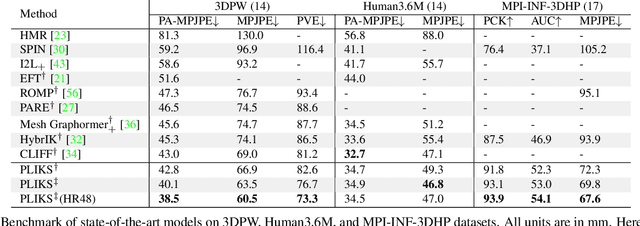
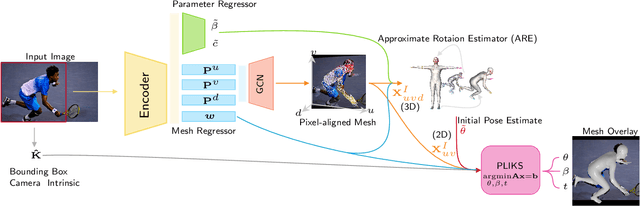
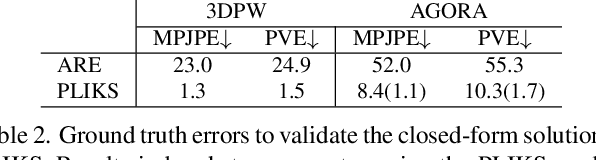
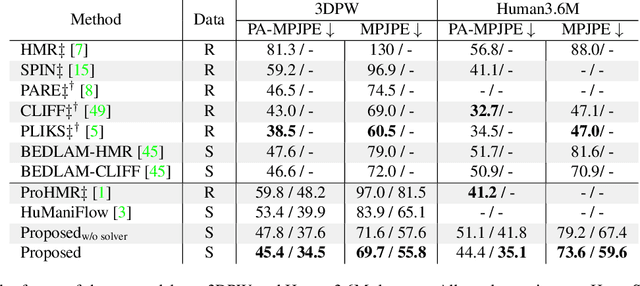
Abstract:We consider the problem of reconstructing a 3D mesh of the human body from a single 2D image as a model-in-the-loop optimization problem. Existing approaches often regress the shape, pose, and translation parameters of a parametric statistical model assuming a weak-perspective camera. In contrast, we first estimate 2D pixel-aligned vertices in image space and propose PLIKS (Pseudo-Linear Inverse Kinematic Solver) to regress the model parameters by minimizing a linear least squares problem. PLIKS is a linearized formulation of the parametric SMPL model, which provides an optimal pose and shape solution from an adequate initialization. Our method is based on analytically calculating an initial pose estimate from the network predicted 3D mesh followed by PLIKS to obtain an optimal solution for the given constraints. As our framework makes use of 2D pixel-aligned maps, it is inherently robust to partial occlusion. To demonstrate the performance of the proposed approach, we present quantitative evaluations which confirm that PLIKS achieves more accurate reconstruction with greater than 10% improvement compared to other state-of-the-art methods with respect to the standard 3D human pose and shape benchmarks while also obtaining a reconstruction error improvement of 12.9 mm on the newer AGORA dataset.
Deep Learning compatible Differentiable X-ray Projections for Inverse Rendering
Feb 04, 2021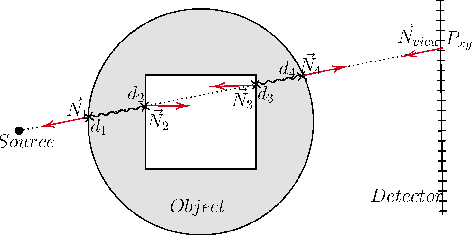

Abstract:Many minimally invasive interventional procedures still rely on 2D fluoroscopic imaging. Generating a patient-specific 3D model from these X-ray projection data would allow to improve the procedural workflow, e.g. by providing assistance functions such as automatic positioning. To accomplish this, two things are required. First, a statistical human shape model of the human anatomy and second, a differentiable X-ray renderer. In this work, we propose a differentiable renderer by deriving the distance travelled by a ray inside mesh structures to generate a distance map. To demonstrate its functioning, we use it for simulating X-ray images from human shape models. Then we show its application by solving the inverse problem, namely reconstructing 3D models from real 2D fluoroscopy images of the pelvis, which is an ideal anatomical structure for patient registration. This is accomplished by an iterative optimization strategy using gradient descent. With the majority of the pelvis being in the fluoroscopic field of view, we achieve a mean Hausdorff distance of 30 mm between the reconstructed model and the ground truth segmentation.
X-ray Scatter Estimation Using Deep Splines
Jan 22, 2021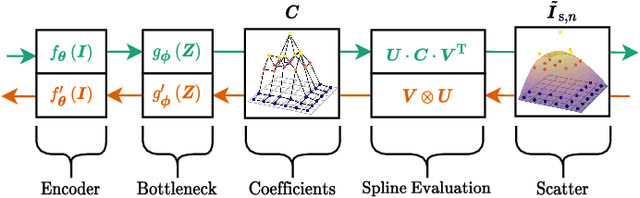
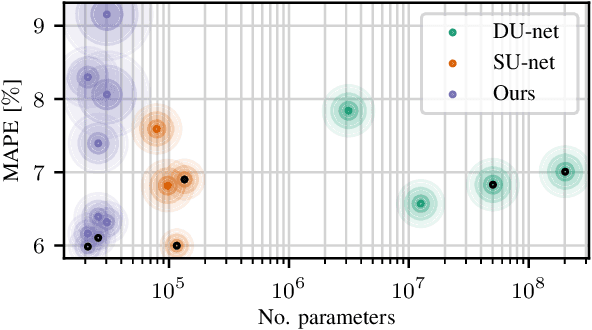
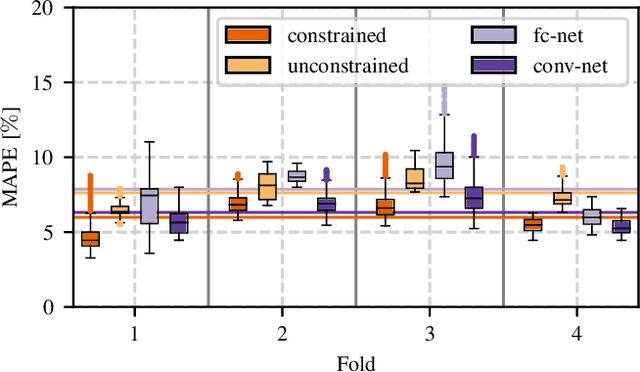
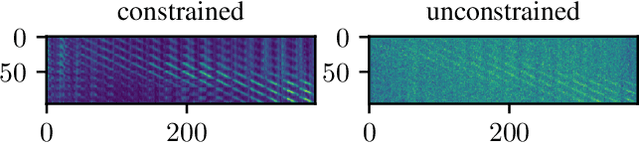
Abstract:Algorithmic X-ray scatter compensation is a desirable technique in flat-panel X-ray imaging and cone-beam computed tomography. State-of-the-art U-net based image translation approaches yielded promising results. As there are no physics constraints applied to the output of the U-Net, it cannot be ruled out that it yields spurious results. Unfortunately, those may be misleading in the context of medical imaging. To overcome this problem, we propose to embed B-splines as a known operator into neural networks. This inherently limits their predictions to well-behaved and smooth functions. In a study using synthetic head and thorax data as well as real thorax phantom data, we found that our approach performed on par with U-net when comparing both algorithms based on quantitative performance metrics. However, our approach not only reduces runtime and parameter complexity, but we also found it much more robust to unseen noise levels. While the U-net responded with visible artifacts, our approach preserved the X-ray signal's frequency characteristics.
Simultaneous Estimation of X-ray Back-Scatter and Forward-Scatter using Multi-Task Learning
Jul 08, 2020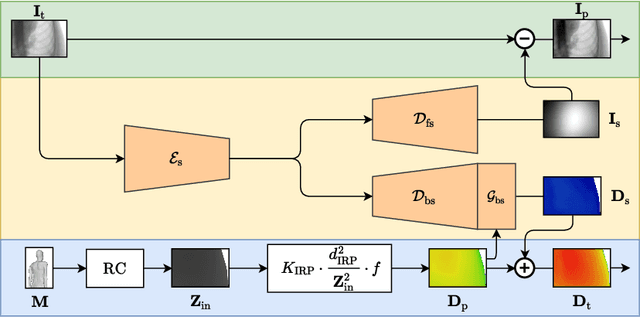
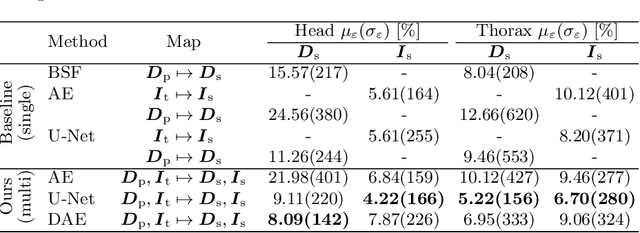
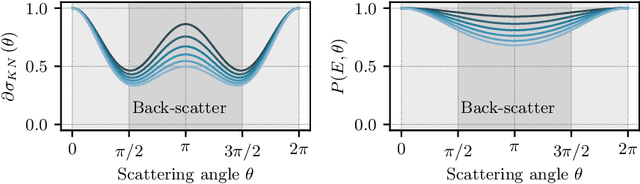
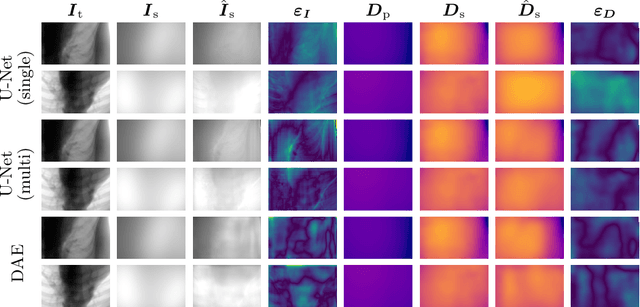
Abstract:Scattered radiation is a major concern impacting X-ray image-guided procedures in two ways. First, back-scatter significantly contributes to patient (skin) dose during complicated interventions. Second, forward-scattered radiation reduces contrast in projection images and introduces artifacts in 3-D reconstructions. While conventionally employed anti-scatter grids improve image quality by blocking X-rays, the additional attenuation due to the anti-scatter grid at the detector needs to be compensated for by a higher patient entrance dose. This also increases the room dose affecting the staff caring for the patient. For skin dose quantification, back-scatter is usually accounted for by applying pre-determined scalar back-scatter factors or linear point spread functions to a primary kerma forward projection onto a patient surface point. However, as patients come in different shapes, the generalization of conventional methods is limited. Here, we propose a novel approach combining conventional techniques with learning-based methods to simultaneously estimate the forward-scatter reaching the detector as well as the back-scatter affecting the patient skin dose. Knowing the forward-scatter, we can correct X-ray projections, while a good estimate of the back-scatter component facilitates an improved skin dose assessment. To simultaneously estimate forward-scatter as well as back-scatter, we propose a multi-task approach for joint back- and forward-scatter estimation by combining X-ray physics with neural networks. We show that, in theory, highly accurate scatter estimation in both cases is possible. In addition, we identify research directions for our multi-task framework and learning-based scatter estimation in general.
Action Learning for 3D Point Cloud Based Organ Segmentation
Jun 14, 2018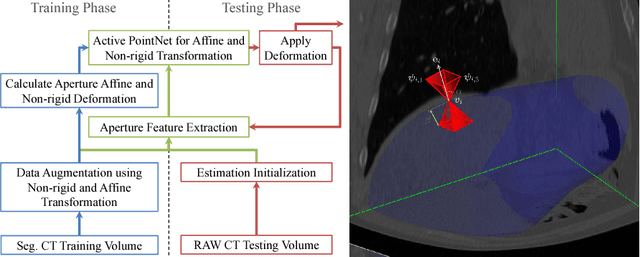
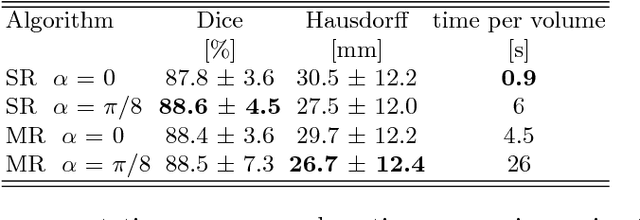
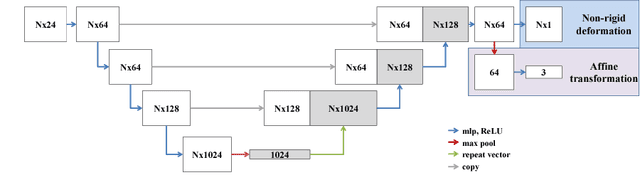
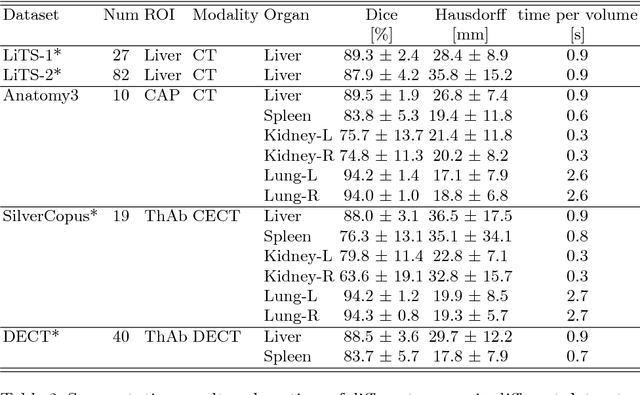
Abstract:We propose a novel point cloud based 3D organ segmentation pipeline utilizing deep Q-learning. In order to preserve shape properties, the learning process is guided using a statistical shape model. The trained agent directly predicts piece-wise linear transformations for all vertices in each iteration. This mapping between the ideal transformation for an object outline estimation is learned based on image features. To this end, we introduce aperture features that extract gray values by sampling the 3D volume within the cone centered around the associated vertex and its normal vector. Our approach is also capable of estimating a hierarchical pyramid of non rigid deformations for multi-resolution meshes. In the application phase, we use a marginal approach to gradually estimate affine as well as non-rigid transformations. We performed extensive evaluations to highlight the robust performance of our approach on a variety of challenge data as well as clinical data. Additionally, our method has a run time ranging from 0.3 to 2.7 seconds to segment each organ. In addition, we show that the proposed method can be applied to different organs, X-ray based modalities, and scanning protocols without the need of transfer learning. As we learn actions, even unseen reference meshes can be processed as demonstrated in an example with the Visible Human. From this we conclude that our method is robust, and we believe that our method can be successfully applied to many more applications, in particular, in the interventional imaging space.
3-D/2-D Registration of Cardiac Structures by 3-D Contrast Agent Distribution Estimation
Jan 22, 2016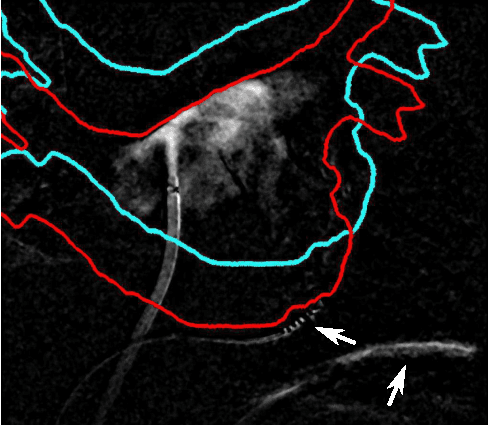
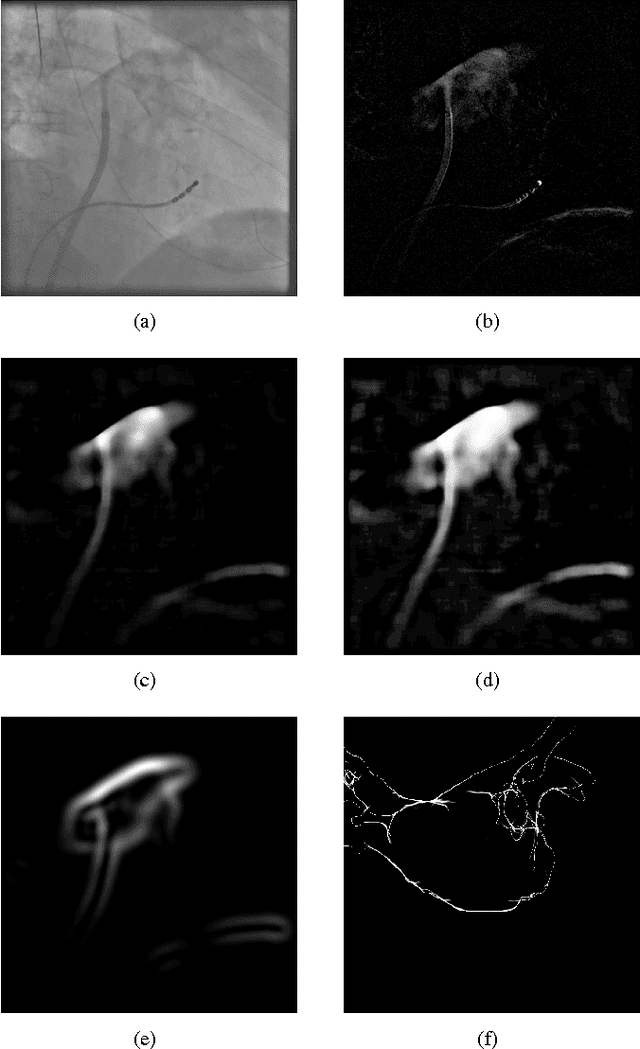
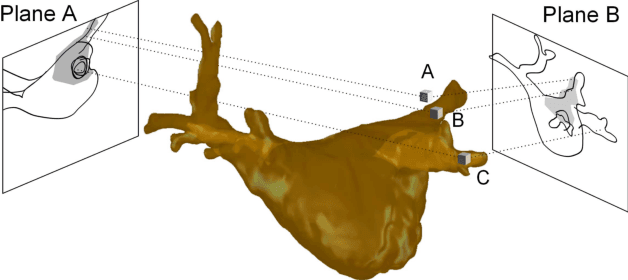
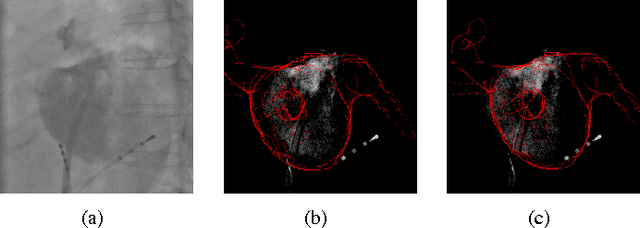
Abstract:For augmented fluoroscopy during cardiac catheter ablation procedures, a preoperatively acquired 3-D model of the left atrium of the patient can be registered to X-ray images. Therefore the 3D-model is matched with the contrast agent based appearance of the left atrium. Commonly, only small amounts of contrast agent (CA) are used to locate the left atrium. This is why we focus on robust registration methods that work also if the structure of interest is only partially contrasted. In particular, we propose two similarity measures for CA-based registration: The first similarity measure, explicit apparent edges, focuses on edges of the patient anatomy made visible by contrast agent and can be computed quickly on the GPU. The second novel similarity measure computes a contrast agent distribution estimate (CADE) inside the 3-D model and rates its consistency with the CA seen in biplane fluoroscopic images. As the CADE computation involves a reconstruction of CA in 3-D using the CA within the fluoroscopic images, it is slower. Using a combination of both methods, our evaluation on 11 well-contrasted clinical datasets yielded an error of 7.9+/-6.3 mm over all frames. For 10 datasets with little CA, we obtained an error of 8.8+/-6.7 mm. Our new methods outperform a registration based on the projected shadow significantly (p<0.05).
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge