Andrea Davidson
MANDARIN: Mixture-of-Experts Framework for Dynamic Delirium and Coma Prediction in ICU Patients: Development and Validation of an Acute Brain Dysfunction Prediction Model
Mar 08, 2025Abstract:Acute brain dysfunction (ABD) is a common, severe ICU complication, presenting as delirium or coma and leading to prolonged stays, increased mortality, and cognitive decline. Traditional screening tools like the Glasgow Coma Scale (GCS), Confusion Assessment Method (CAM), and Richmond Agitation-Sedation Scale (RASS) rely on intermittent assessments, causing delays and inconsistencies. In this study, we propose MANDARIN (Mixture-of-Experts Framework for Dynamic Delirium and Coma Prediction in ICU Patients), a 1.5M-parameter mixture-of-experts neural network to predict ABD in real-time among ICU patients. The model integrates temporal and static data from the ICU to predict the brain status in the next 12 to 72 hours, using a multi-branch approach to account for current brain status. The MANDARIN model was trained on data from 92,734 patients (132,997 ICU admissions) from 2 hospitals between 2008-2019 and validated externally on data from 11,719 patients (14,519 ICU admissions) from 15 hospitals and prospectively on data from 304 patients (503 ICU admissions) from one hospital in 2021-2024. Three datasets were used: the University of Florida Health (UFH) dataset, the electronic ICU Collaborative Research Database (eICU), and the Medical Information Mart for Intensive Care (MIMIC)-IV dataset. MANDARIN significantly outperforms the baseline neurological assessment scores (GCS, CAM, and RASS) for delirium prediction in both external (AUROC 75.5% CI: 74.2%-76.8% vs 68.3% CI: 66.9%-69.5%) and prospective (AUROC 82.0% CI: 74.8%-89.2% vs 72.7% CI: 65.5%-81.0%) cohorts, as well as for coma prediction (external AUROC 87.3% CI: 85.9%-89.0% vs 72.8% CI: 70.6%-74.9%, and prospective AUROC 93.4% CI: 88.5%-97.9% vs 67.7% CI: 57.7%-76.8%) with a 12-hour lead time. This tool has the potential to assist clinicians in decision-making by continuously monitoring the brain status of patients in the ICU.
MANGO: Multimodal Acuity traNsformer for intelliGent ICU Outcomes
Dec 13, 2024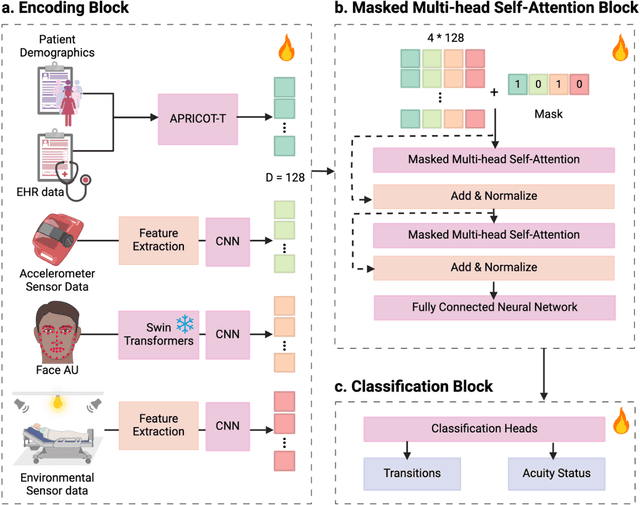
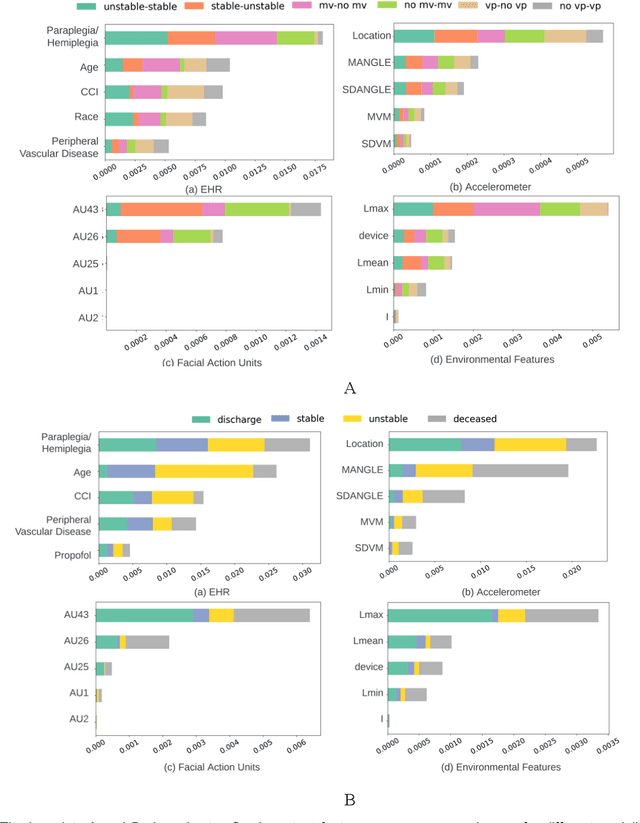
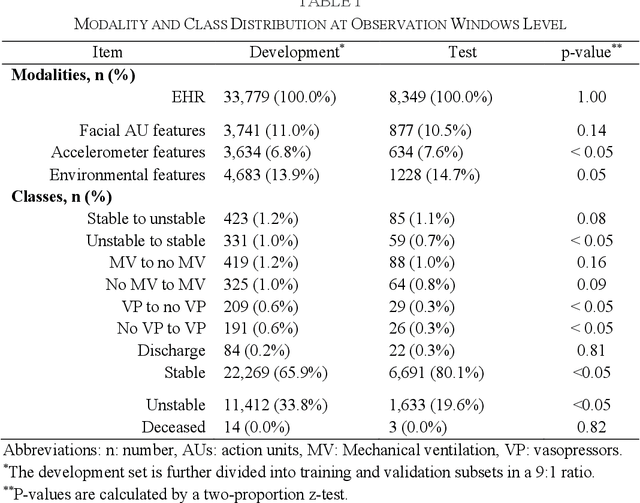
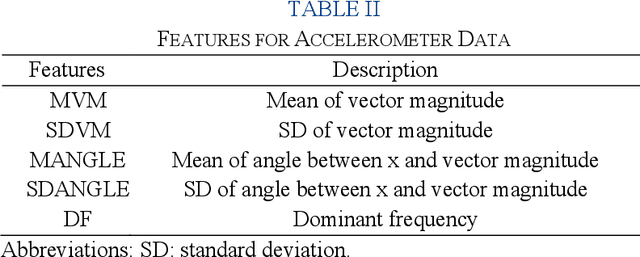
Abstract:Estimation of patient acuity in the Intensive Care Unit (ICU) is vital to ensure timely and appropriate interventions. Advances in artificial intelligence (AI) technologies have significantly improved the accuracy of acuity predictions. However, prior studies using machine learning for acuity prediction have predominantly relied on electronic health records (EHR) data, often overlooking other critical aspects of ICU stay, such as patient mobility, environmental factors, and facial cues indicating pain or agitation. To address this gap, we present MANGO: the Multimodal Acuity traNsformer for intelliGent ICU Outcomes, designed to enhance the prediction of patient acuity states, transitions, and the need for life-sustaining therapy. We collected a multimodal dataset ICU-Multimodal, incorporating four key modalities, EHR data, wearable sensor data, video of patient's facial cues, and ambient sensor data, which we utilized to train MANGO. The MANGO model employs a multimodal feature fusion network powered by Transformer masked self-attention method, enabling it to capture and learn complex interactions across these diverse data modalities even when some modalities are absent. Our results demonstrated that integrating multiple modalities significantly improved the model's ability to predict acuity status, transitions, and the need for life-sustaining therapy. The best-performing models achieved an area under the receiver operating characteristic curve (AUROC) of 0.76 (95% CI: 0.72-0.79) for predicting transitions in acuity status and the need for life-sustaining therapy, while 0.82 (95% CI: 0.69-0.89) for acuity status prediction...
DeLLiriuM: A large language model for delirium prediction in the ICU using structured EHR
Oct 22, 2024



Abstract:Delirium is an acute confusional state that has been shown to affect up to 31% of patients in the intensive care unit (ICU). Early detection of this condition could lead to more timely interventions and improved health outcomes. While artificial intelligence (AI) models have shown great potential for ICU delirium prediction using structured electronic health records (EHR), most of them have not explored the use of state-of-the-art AI models, have been limited to single hospitals, or have been developed and validated on small cohorts. The use of large language models (LLM), models with hundreds of millions to billions of parameters, with structured EHR data could potentially lead to improved predictive performance. In this study, we propose DeLLiriuM, a novel LLM-based delirium prediction model using EHR data available in the first 24 hours of ICU admission to predict the probability of a patient developing delirium during the rest of their ICU admission. We develop and validate DeLLiriuM on ICU admissions from 104,303 patients pertaining to 195 hospitals across three large databases: the eICU Collaborative Research Database, the Medical Information Mart for Intensive Care (MIMIC)-IV, and the University of Florida Health's Integrated Data Repository. The performance measured by the area under the receiver operating characteristic curve (AUROC) showed that DeLLiriuM outperformed all baselines in two external validation sets, with 0.77 (95% confidence interval 0.76-0.78) and 0.84 (95% confidence interval 0.83-0.85) across 77,543 patients spanning 194 hospitals. To the best of our knowledge, DeLLiriuM is the first LLM-based delirium prediction tool for the ICU based on structured EHR data, outperforming deep learning baselines which employ structured features and can provide helpful information to clinicians for timely interventions.
The Potential of Wearable Sensors for Assessing Patient Acuity in Intensive Care Unit (ICU)
Nov 03, 2023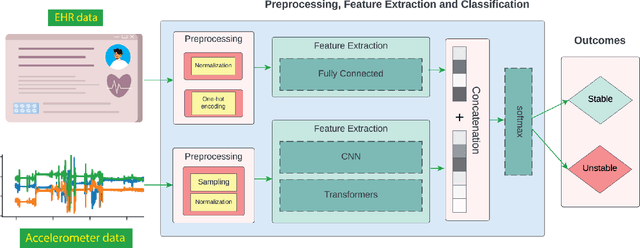
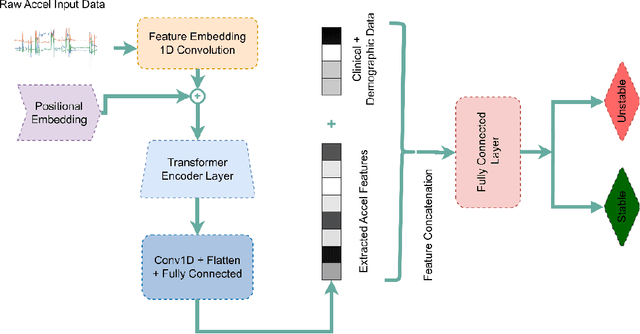

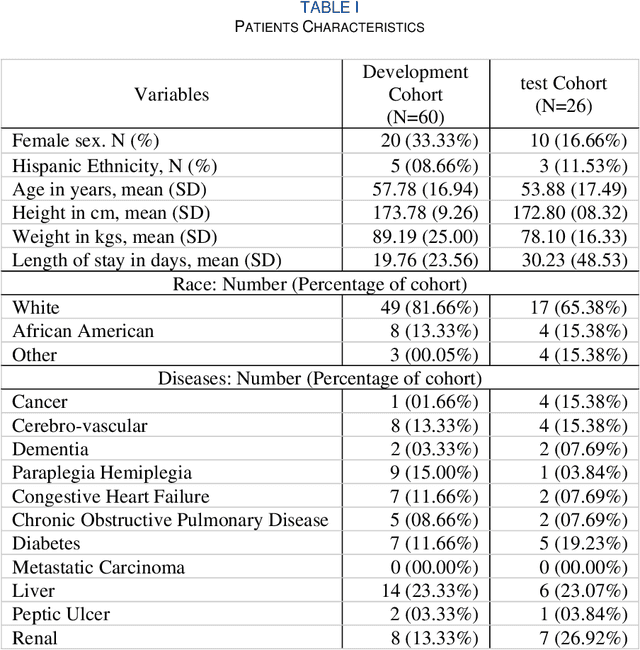
Abstract:Acuity assessments are vital in critical care settings to provide timely interventions and fair resource allocation. Traditional acuity scores rely on manual assessments and documentation of physiological states, which can be time-consuming, intermittent, and difficult to use for healthcare providers. Furthermore, such scores do not incorporate granular information such as patients' mobility level, which can indicate recovery or deterioration in the ICU. We hypothesized that existing acuity scores could be potentially improved by employing Artificial Intelligence (AI) techniques in conjunction with Electronic Health Records (EHR) and wearable sensor data. In this study, we evaluated the impact of integrating mobility data collected from wrist-worn accelerometers with clinical data obtained from EHR for developing an AI-driven acuity assessment score. Accelerometry data were collected from 86 patients wearing accelerometers on their wrists in an academic hospital setting. The data was analyzed using five deep neural network models: VGG, ResNet, MobileNet, SqueezeNet, and a custom Transformer network. These models outperformed a rule-based clinical score (SOFA= Sequential Organ Failure Assessment) used as a baseline, particularly regarding the precision, sensitivity, and F1 score. The results showed that while a model relying solely on accelerometer data achieved limited performance (AUC 0.50, Precision 0.61, and F1-score 0.68), including demographic information with the accelerometer data led to a notable enhancement in performance (AUC 0.69, Precision 0.75, and F1-score 0.67). This work shows that the combination of mobility and patient information can successfully differentiate between stable and unstable states in critically ill patients.
Detecting Visual Cues in the Intensive Care Unit and Association with Patient Clinical Status
Nov 01, 2023



Abstract:Intensive Care Units (ICU) provide close supervision and continuous care to patients with life-threatening conditions. However, continuous patient assessment in the ICU is still limited due to time constraints and the workload on healthcare providers. Existing patient assessments in the ICU such as pain or mobility assessment are mostly sporadic and administered manually, thus introducing the potential for human errors. Developing Artificial intelligence (AI) tools that can augment human assessments in the ICU can be beneficial for providing more objective and granular monitoring capabilities. For example, capturing the variations in a patient's facial cues related to pain or agitation can help in adjusting pain-related medications or detecting agitation-inducing conditions such as delirium. Additionally, subtle changes in visual cues during or prior to adverse clinical events could potentially aid in continuous patient monitoring when combined with high-resolution physiological signals and Electronic Health Record (EHR) data. In this paper, we examined the association between visual cues and patient condition including acuity status, acute brain dysfunction, and pain. We leveraged our AU-ICU dataset with 107,064 frames collected in the ICU annotated with facial action units (AUs) labels by trained annotators. We developed a new "masked loss computation" technique that addresses the data imbalance problem by maximizing data resource utilization. We trained the model using our AU-ICU dataset in conjunction with three external datasets to detect 18 AUs. The SWIN Transformer model achieved 0.57 mean F1-score and 0.89 mean accuracy on the test set. Additionally, we performed AU inference on 634,054 frames to evaluate the association between facial AUs and clinically important patient conditions such as acuity status, acute brain dysfunction, and pain.
Predicting risk of delirium from ambient noise and light information in the ICU
Mar 11, 2023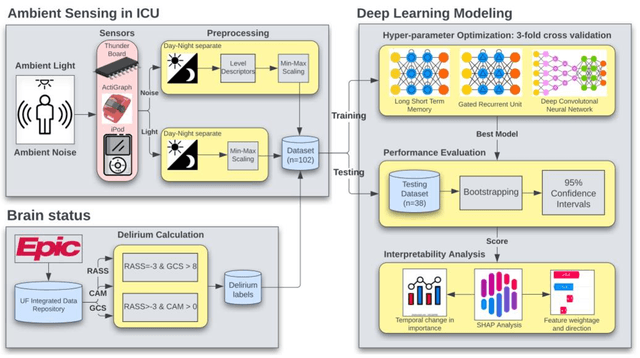
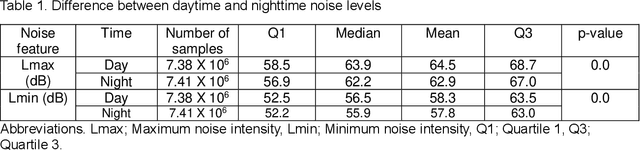
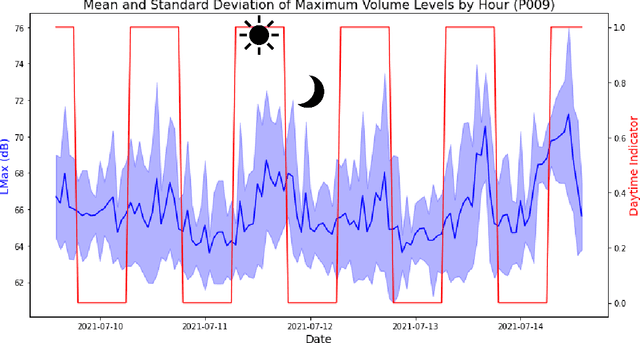
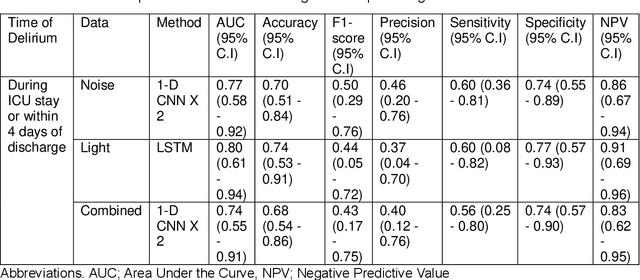
Abstract:Existing Intensive Care Unit (ICU) delirium prediction models do not consider environmental factors despite strong evidence of their influence on delirium. This study reports the first deep-learning based delirium prediction model for ICU patients using only ambient noise and light information. Ambient light and noise intensities were measured from ICU rooms of 102 patients from May 2021 to September 2022 using Thunderboard, ActiGraph sensors and an iPod with AudioTools application. These measurements were divided into daytime (0700 to 1859) and nighttime (1900 to 0659). Deep learning models were trained using this data to predict the incidence of delirium during ICU stay or within 4 days of discharge. Finally, outcome scores were analyzed to evaluate the importance and directionality of every feature. Daytime noise levels were significantly higher than nighttime noise levels. When using only noise features or a combination of noise and light features 1-D convolutional neural networks (CNN) achieved the strongest performance: AUC=0.77, 0.74; Sensitivity=0.60, 0.56; Specificity=0.74, 0.74; Precision=0.46, 0.40 respectively. Using only light features, Long Short-Term Memory (LSTM) networks performed best: AUC=0.80, Sensitivity=0.60, Specificity=0.77, Precision=0.37. Maximum nighttime and minimum daytime noise levels were the strongest positive and negative predictors of delirium respectively. Nighttime light level was a stronger predictor of delirium than daytime light level. Total influence of light features outweighed that of noise features on the second and fourth day of ICU stay. This study shows that ambient light and noise intensities are strong predictors of long-term delirium incidence in the ICU. It reveals that daytime and nighttime environmental factors might influence delirium differently and that the importance of light and noise levels vary over the course of an ICU stay.
End-to-End Machine Learning Framework for Facial AU Detection in Intensive Care Units
Nov 12, 2022



Abstract:Pain is a common occurrence among patients admitted to Intensive Care Units. Pain assessment in ICU patients still remains a challenge for clinicians and ICU staff, specifically in cases of non-verbal sedated, mechanically ventilated, and intubated patients. Current manual observation-based pain assessment tools are limited by the frequency of pain observations administered and are subjective to the observer. Facial behavior is a major component in observation-based tools. Furthermore, previous literature shows the feasibility of painful facial expression detection using facial action units (AUs). However, these approaches are limited to controlled or semi-controlled environments and have never been validated in clinical settings. In this study, we present our Pain-ICU dataset, the largest dataset available targeting facial behavior analysis in the dynamic ICU environment. Our dataset comprises 76,388 patient facial image frames annotated with AUs obtained from 49 adult patients admitted to ICUs at the University of Florida Health Shands hospital. In this work, we evaluated two vision transformer models, namely ViT and SWIN, for AU detection on our Pain-ICU dataset and also external datasets. We developed a completely end-to-end AU detection pipeline with the objective of performing real-time AU detection in the ICU. The SWIN transformer Base variant achieved 0.88 F1-score and 0.85 accuracy on the held-out test partition of the Pain-ICU dataset.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge