Kyle Lafata
Digital staining in optical microscopy using deep learning -- a review
Mar 14, 2023Abstract:Until recently, conventional biochemical staining had the undisputed status as well-established benchmark for most biomedical problems related to clinical diagnostics, fundamental research and biotechnology. Despite this role as gold-standard, staining protocols face several challenges, such as a need for extensive, manual processing of samples, substantial time delays, altered tissue homeostasis, limited choice of contrast agents for a given sample, 2D imaging instead of 3D tomography and many more. Label-free optical technologies, on the other hand, do not rely on exogenous and artificial markers, by exploiting intrinsic optical contrast mechanisms, where the specificity is typically less obvious to the human observer. Over the past few years, digital staining has emerged as a promising concept to use modern deep learning for the translation from optical contrast to established biochemical contrast of actual stainings. In this review article, we provide an in-depth analysis of the current state-of-the-art in this field, suggest methods of good practice, identify pitfalls and challenges and postulate promising advances towards potential future implementations and applications.
Quantifying U-Net Uncertainty in Multi-Parametric MRI-based Glioma Segmentation by Spherical Image Projection
Oct 12, 2022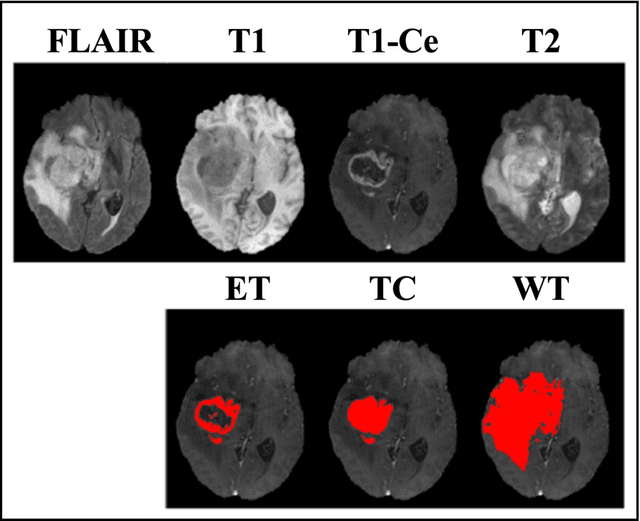
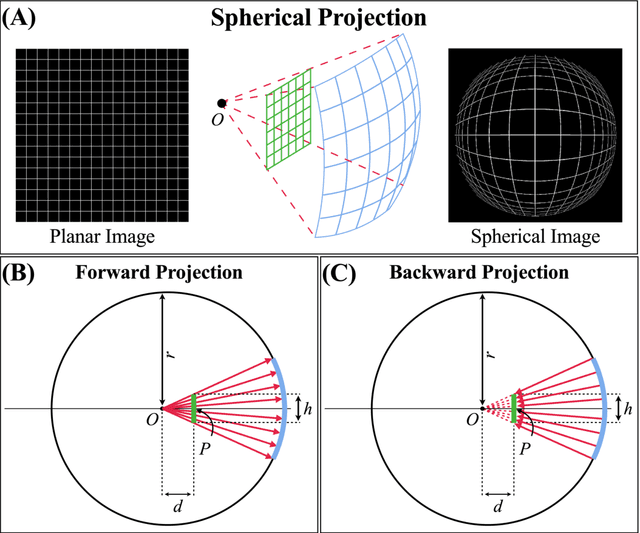
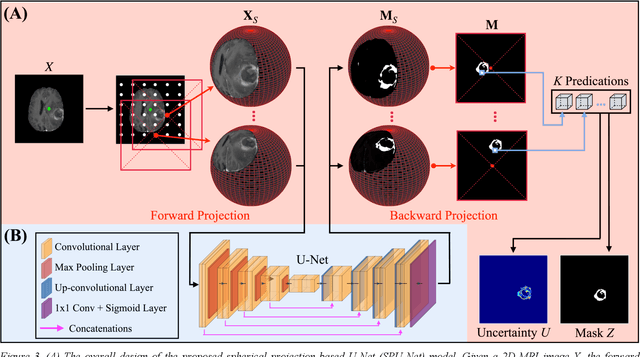
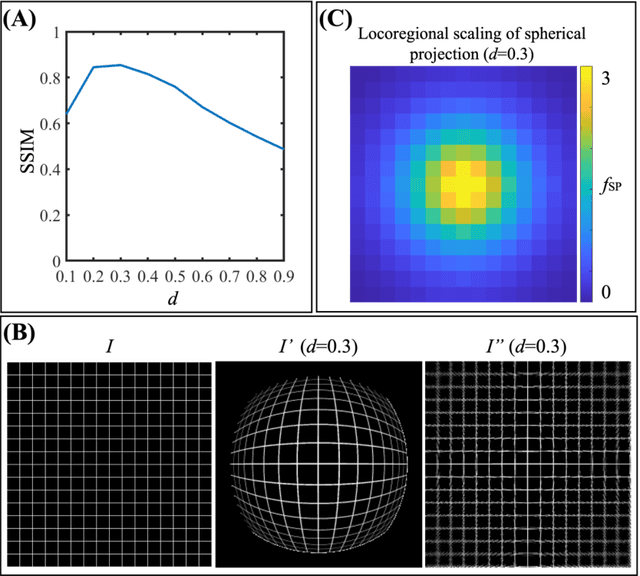
Abstract:Purpose: To develop a U-Net segmentation uncertainty quantification method based on spherical image projection of multi-parametric MRI (MP-MRI) in glioma segmentation. Methods: The projection of planar MRI onto a spherical surface retains global anatomical information. By incorporating such image transformation in our proposed spherical projection-based U-Net (SPU-Net) segmentation model design, multiple segmentation predictions can be obtained for a single MRI. The final segmentation is the average of all predictions, and the variation can be shown as an uncertainty map. An uncertainty score was introduced to compare the uncertainty measurements' performance. The SPU-Net model was implemented on 369 glioma patients with MP-MRI scans. Three SPU-Nets were trained to segment enhancing tumor (ET), tumor core (TC), and whole tumor (WT), respectively. The SPU-Net was compared with (1) classic U-Net with test-time augmentation (TTA) and (2) linear scaling-based U-Net (LSU-Net) in both segmentation accuracy (Dice coefficient) and uncertainty (uncertainty map and uncertainty score). Results: The SPU-Net achieved low uncertainty for correct segmentation predictions (e.g., tumor interior or healthy tissue interior) and high uncertainty for incorrect results (e.g., tumor boundaries). This model could allow the identification of missed tumor targets or segmentation errors in U-Net. The SPU-Net achieved the highest uncertainty scores for 3 targets (ET/TC/WT): 0.826/0.848/0.936, compared to 0.784/0.643/0.872 for the U-Net with TTA and 0.743/0.702/0.876 for the LSU-Net. The SPU-Net also achieved statistically significantly higher Dice coefficients. Conclusion: The SPU-Net offers a powerful tool to quantify glioma segmentation uncertainty while improving segmentation accuracy. The proposed method can be generalized to other medical image-related deep-learning applications for uncertainty evaluation.
A Neural Ordinary Differential Equation Model for Visualizing Deep Neural Network Behaviors in Multi-Parametric MRI based Glioma Segmentation
Mar 23, 2022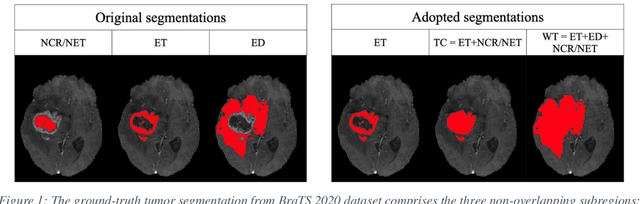
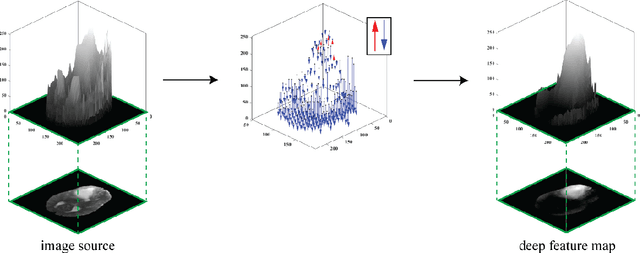
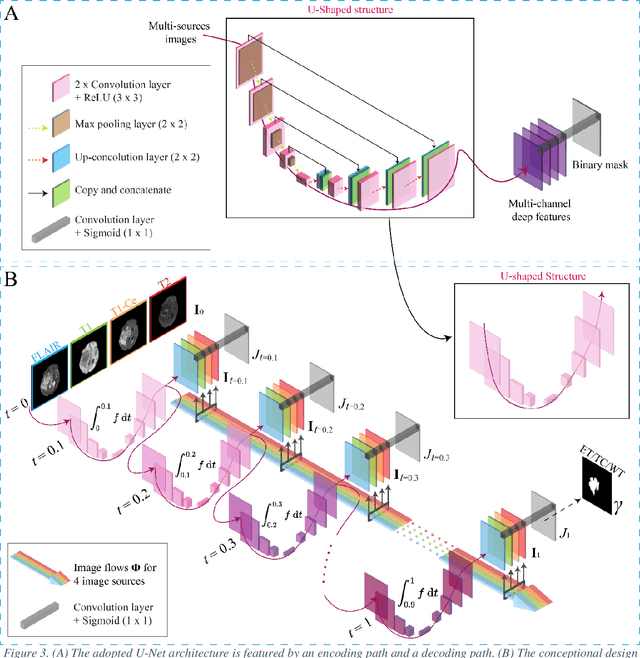
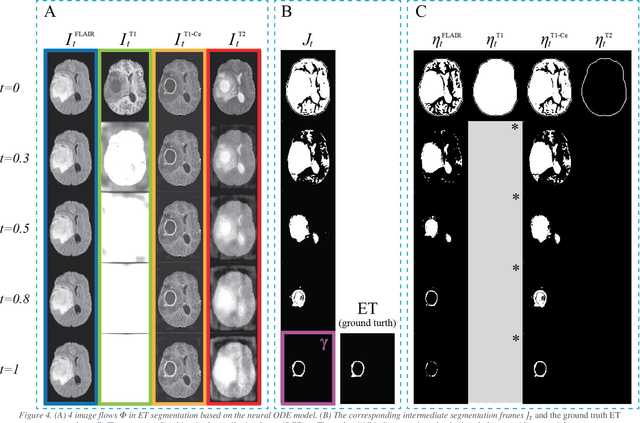
Abstract:Purpose: To develop a neural ordinary differential equation (ODE) model for visualizing deep neural network (DNN) behavior during multi-parametric MRI (mp-MRI) based glioma segmentation as a method to enhance deep learning explainability. Methods: By hypothesizing that deep feature extraction can be modeled as a spatiotemporally continuous process, we designed a novel deep learning model, neural ODE, in which deep feature extraction was governed by an ODE without explicit expression. The dynamics of 1) MR images after interactions with DNN and 2) segmentation formation can be visualized after solving ODE. An accumulative contribution curve (ACC) was designed to quantitatively evaluate the utilization of each MRI by DNN towards the final segmentation results. The proposed neural ODE model was demonstrated using 369 glioma patients with a 4-modality mp-MRI protocol: T1, contrast-enhanced T1 (T1-Ce), T2, and FLAIR. Three neural ODE models were trained to segment enhancing tumor (ET), tumor core (TC), and whole tumor (WT). The key MR modalities with significant utilization by DNN were identified based on ACC analysis. Segmentation results by DNN using only the key MR modalities were compared to the ones using all 4 MR modalities. Results: All neural ODE models successfully illustrated image dynamics as expected. ACC analysis identified T1-Ce as the only key modality in ET and TC segmentations, while both FLAIR and T2 were key modalities in WT segmentation. Compared to the U-Net results using all 4 MR modalities, Dice coefficient of ET (0.784->0.775), TC (0.760->0.758), and WT (0.841->0.837) using the key modalities only had minimal differences without significance. Conclusion: The neural ODE model offers a new tool for optimizing the deep learning model inputs with enhanced explainability. The presented methodology can be generalized to other medical image-related deep learning applications.
Post-Radiotherapy PET Image Outcome Prediction by Deep Learning under Biological Model Guidance: A Feasibility Study of Oropharyngeal Cancer Application
May 22, 2021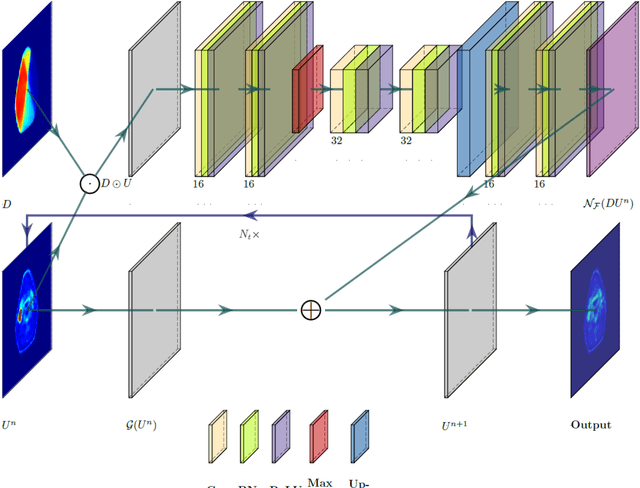
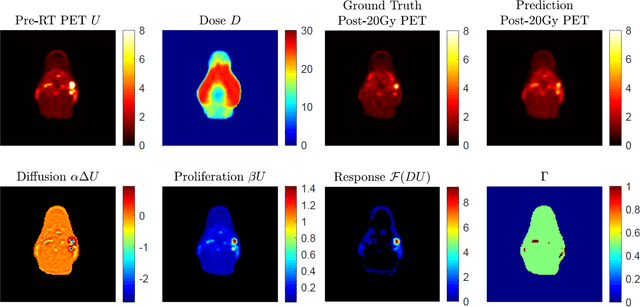
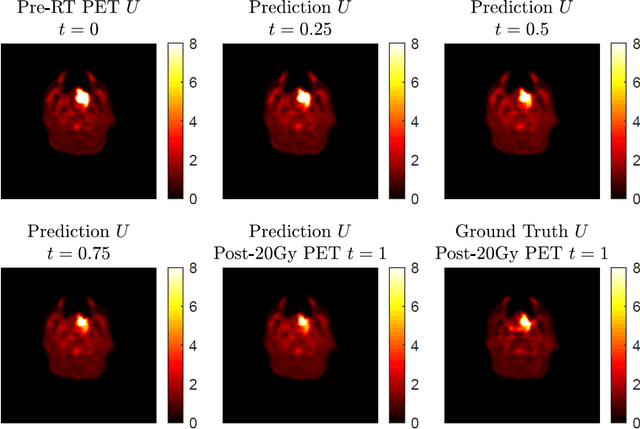
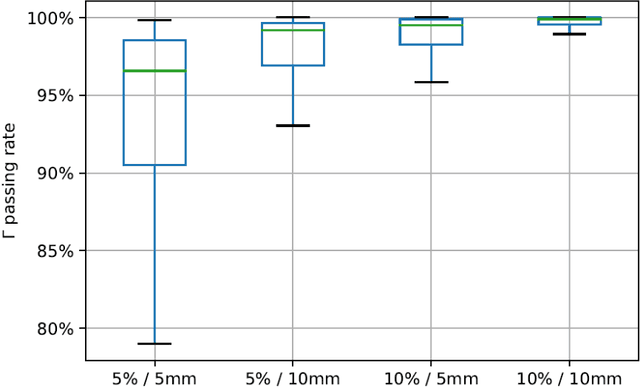
Abstract:This paper develops a method of biologically guided deep learning for post-radiation FDG-PET image outcome prediction based on pre-radiation images and radiotherapy dose information. Based on the classic reaction-diffusion mechanism, a novel biological model was proposed using a partial differential equation that incorporates spatial radiation dose distribution as a patient-specific treatment information variable. A 7-layer encoder-decoder-based convolutional neural network (CNN) was designed and trained to learn the proposed biological model. As such, the model could generate post-radiation FDG-PET image outcome predictions with possible time-series transition from pre-radiotherapy image states to post-radiotherapy states. The proposed method was developed using 64 oropharyngeal patients with paired FDG-PET studies before and after 20Gy delivery (2Gy/daily fraction) by IMRT. In a two-branch deep learning execution, the proposed CNN learns specific terms in the biological model from paired FDG-PET images and spatial dose distribution as in one branch, and the biological model generates post-20Gy FDG-PET image prediction in the other branch. The proposed method successfully generated post-20Gy FDG-PET image outcome prediction with breakdown illustrations of biological model components. Time-series FDG-PET image predictions were generated to demonstrate the feasibility of disease response rendering. The developed biologically guided deep learning method achieved post-20Gy FDG-PET image outcome predictions in good agreement with ground-truth results. With break-down biological modeling components, the outcome image predictions could be used in adaptive radiotherapy decision-making to optimize personalized plans for the best outcome in the future.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge