Zongsheng Hu
Sensitivity analysis of biological washout and depth selection for a machine learning based dose verification framework in proton therapy
Dec 21, 2022



Abstract:Dose verification based on proton-induced positron emitters is a promising quality assurance tool and may leverage the strength of artificial intelligence. To move a step closer towards practical application, the sensitivity analysis of two factors needs to be performed: biological washout and depth selection. selection. A bi-directional recurrent neural network (RNN) model was developed. The training dataset was generated based upon a CT image-based phantom (abdomen region) and multiple beam energies/pathways, using Monte-Carlo simulation (1 mm spatial resolution, no biological washout). For the modeling of biological washout, a simplified analytical model was applied to change raw activity profiles over a period of 5 minutes, incorporating both physical decay and biological washout. For the study of depth selection (a challenge linked to multi field/angle irradiation), truncations were applied at different window lengths (100, 125, 150 mm) to raw activity profiles. Finally, the performance of a worst-case scenario was examined by combining both factors (depth selection: 125 mm, biological washout: 5 mins). The accuracy was quantitatively evaluated in terms of range uncertainty, mean absolute error (MAE) and mean relative errors (MRE). Our proposed AI framework shows good immunity to the perturbation associated with two factors. The detection of proton-induced positron emitters, combined with machine learning, has great potential to implement online patient-specific verification in proton therapy.
Quantifying U-Net Uncertainty in Multi-Parametric MRI-based Glioma Segmentation by Spherical Image Projection
Oct 12, 2022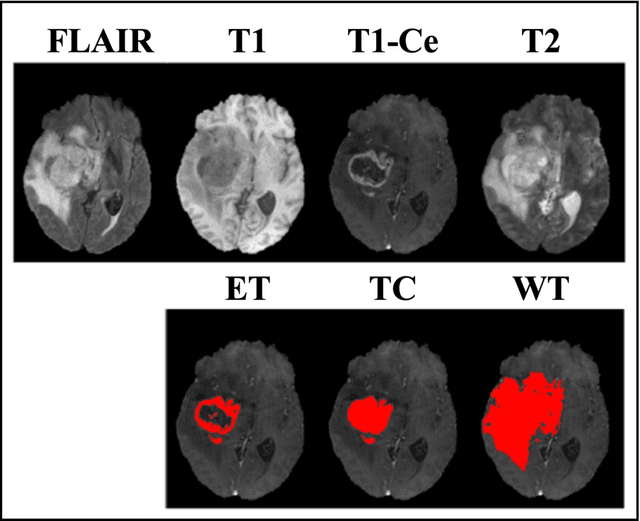
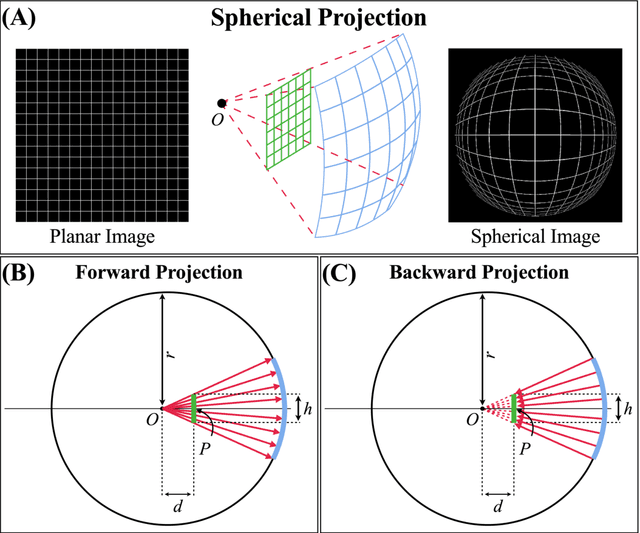
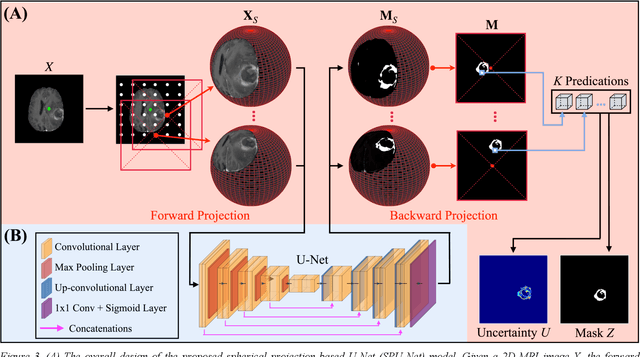
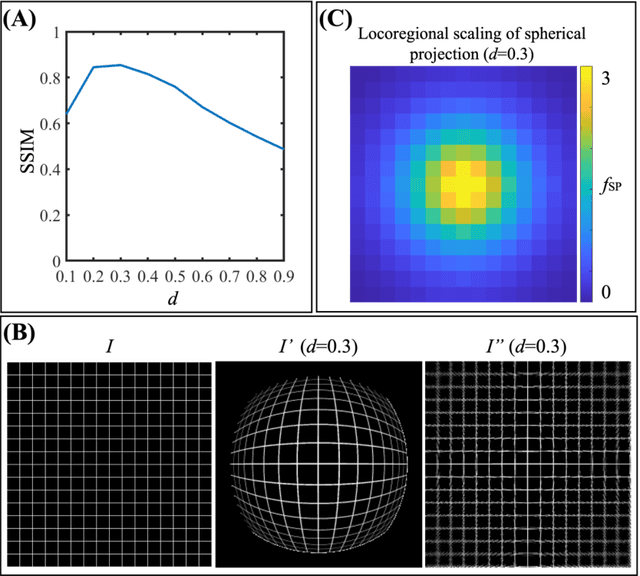
Abstract:Purpose: To develop a U-Net segmentation uncertainty quantification method based on spherical image projection of multi-parametric MRI (MP-MRI) in glioma segmentation. Methods: The projection of planar MRI onto a spherical surface retains global anatomical information. By incorporating such image transformation in our proposed spherical projection-based U-Net (SPU-Net) segmentation model design, multiple segmentation predictions can be obtained for a single MRI. The final segmentation is the average of all predictions, and the variation can be shown as an uncertainty map. An uncertainty score was introduced to compare the uncertainty measurements' performance. The SPU-Net model was implemented on 369 glioma patients with MP-MRI scans. Three SPU-Nets were trained to segment enhancing tumor (ET), tumor core (TC), and whole tumor (WT), respectively. The SPU-Net was compared with (1) classic U-Net with test-time augmentation (TTA) and (2) linear scaling-based U-Net (LSU-Net) in both segmentation accuracy (Dice coefficient) and uncertainty (uncertainty map and uncertainty score). Results: The SPU-Net achieved low uncertainty for correct segmentation predictions (e.g., tumor interior or healthy tissue interior) and high uncertainty for incorrect results (e.g., tumor boundaries). This model could allow the identification of missed tumor targets or segmentation errors in U-Net. The SPU-Net achieved the highest uncertainty scores for 3 targets (ET/TC/WT): 0.826/0.848/0.936, compared to 0.784/0.643/0.872 for the U-Net with TTA and 0.743/0.702/0.876 for the LSU-Net. The SPU-Net also achieved statistically significantly higher Dice coefficients. Conclusion: The SPU-Net offers a powerful tool to quantify glioma segmentation uncertainty while improving segmentation accuracy. The proposed method can be generalized to other medical image-related deep-learning applications for uncertainty evaluation.
A Neural Ordinary Differential Equation Model for Visualizing Deep Neural Network Behaviors in Multi-Parametric MRI based Glioma Segmentation
Mar 23, 2022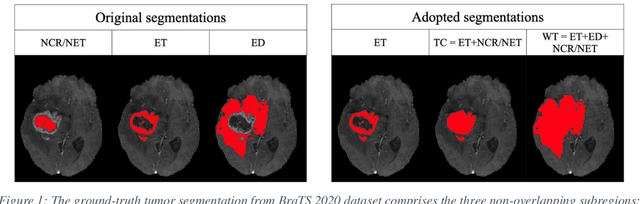
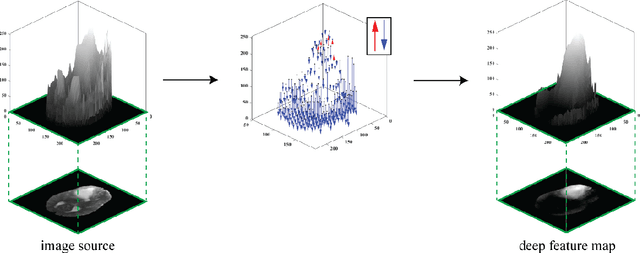
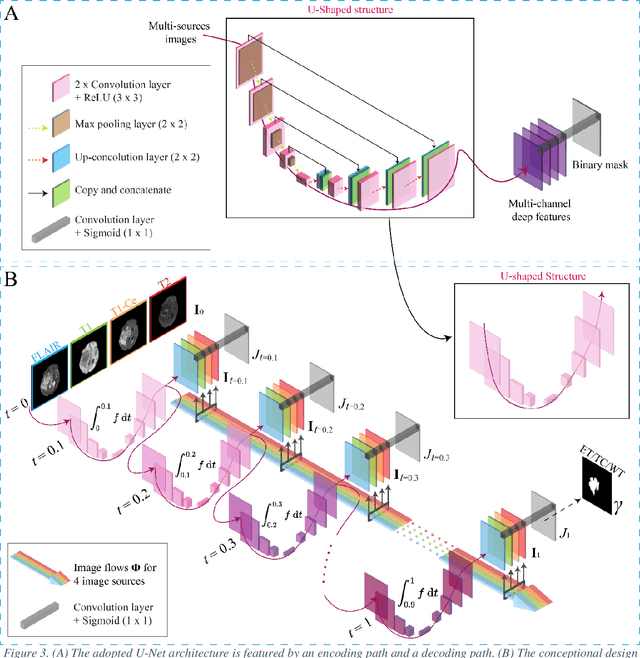
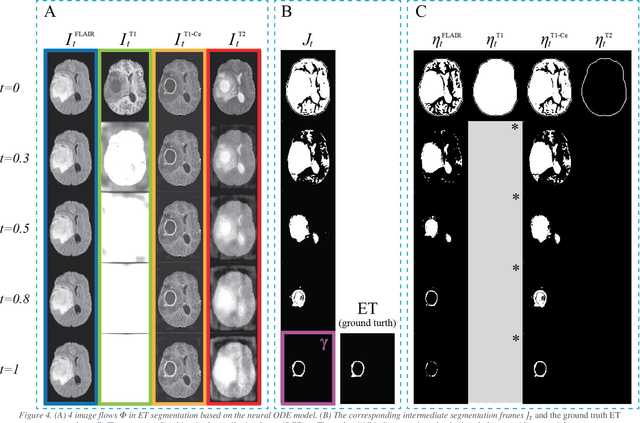
Abstract:Purpose: To develop a neural ordinary differential equation (ODE) model for visualizing deep neural network (DNN) behavior during multi-parametric MRI (mp-MRI) based glioma segmentation as a method to enhance deep learning explainability. Methods: By hypothesizing that deep feature extraction can be modeled as a spatiotemporally continuous process, we designed a novel deep learning model, neural ODE, in which deep feature extraction was governed by an ODE without explicit expression. The dynamics of 1) MR images after interactions with DNN and 2) segmentation formation can be visualized after solving ODE. An accumulative contribution curve (ACC) was designed to quantitatively evaluate the utilization of each MRI by DNN towards the final segmentation results. The proposed neural ODE model was demonstrated using 369 glioma patients with a 4-modality mp-MRI protocol: T1, contrast-enhanced T1 (T1-Ce), T2, and FLAIR. Three neural ODE models were trained to segment enhancing tumor (ET), tumor core (TC), and whole tumor (WT). The key MR modalities with significant utilization by DNN were identified based on ACC analysis. Segmentation results by DNN using only the key MR modalities were compared to the ones using all 4 MR modalities. Results: All neural ODE models successfully illustrated image dynamics as expected. ACC analysis identified T1-Ce as the only key modality in ET and TC segmentations, while both FLAIR and T2 were key modalities in WT segmentation. Compared to the U-Net results using all 4 MR modalities, Dice coefficient of ET (0.784->0.775), TC (0.760->0.758), and WT (0.841->0.837) using the key modalities only had minimal differences without significance. Conclusion: The neural ODE model offers a new tool for optimizing the deep learning model inputs with enhanced explainability. The presented methodology can be generalized to other medical image-related deep learning applications.
A Radiomics-Boosted Deep-Learning Model for COVID-19 and Non-COVID-19 Pneumonia Detection Using Chest X-ray Image
Jul 19, 2021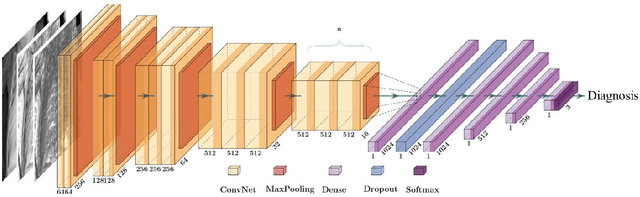
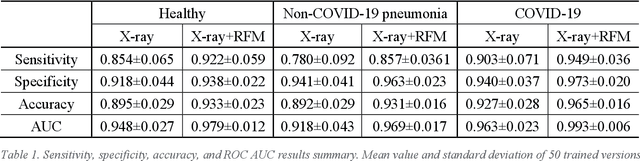
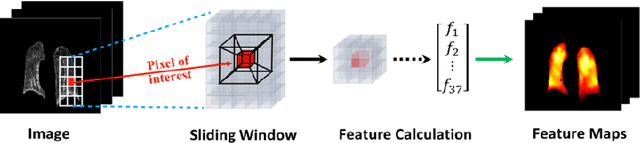
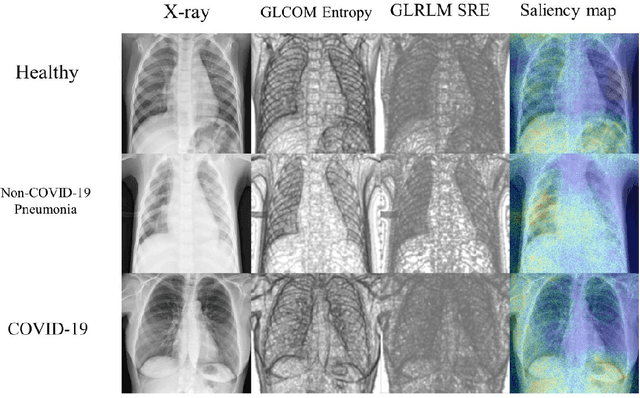
Abstract:To develop a deep-learning model that integrates radiomics analysis for enhanced performance of COVID-19 and Non-COVID-19 pneumonia detection using chest X-ray image, two deep-learning models were trained based on a pre-trained VGG-16 architecture: in the 1st model, X-ray image was the sole input; in the 2nd model, X-ray image and 2 radiomic feature maps (RFM) selected by the saliency map analysis of the 1st model were stacked as the input. Both models were developed using 812 chest X-ray images with 262/288/262 COVID-19/Non-COVID-19 pneumonia/healthy cases, and 649/163 cases were assigned as training-validation/independent test sets. In 1st model using X-ray as the sole input, the 1) sensitivity, 2) specificity, 3) accuracy, and 4) ROC Area-Under-the-Curve of COVID-19 vs Non-COVID-19 pneumonia detection were 1) 0.90$\pm$0.07 vs 0.78$\pm$0.09, 2) 0.94$\pm$0.04 vs 0.94$\pm$0.04, 3) 0.93$\pm$0.03 vs 0.89$\pm$0.03, and 4) 0.96$\pm$0.02 vs 0.92$\pm$0.04. In the 2nd model, two RFMs, Entropy and Short-Run-Emphasize, were selected with their highest cross-correlations with the saliency maps of the 1st model. The corresponding results demonstrated significant improvements (p<0.05) of COVID-19 vs Non-COVID-19 pneumonia detection: 1) 0.95$\pm$0.04 vs 0.85$\pm$0.04, 2) 0.97$\pm$0.02 vs 0.96$\pm$0.02, 3) 0.97$\pm$0.02 vs 0.93$\pm$0.02, and 4) 0.99$\pm$0.01 vs 0.97$\pm$0.02. The reduced variations suggested a superior robustness of 2nd model design.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge