Kevin Cleary
Towards Fluorescence-Guided Autonomous Robotic Partial Nephrectomy on Novel Tissue-Mimicking Hydrogel Phantoms
Mar 04, 2025Abstract:Autonomous robotic systems hold potential for improving renal tumor resection accuracy and patient outcomes. We present a fluorescence-guided robotic system capable of planning and executing incision paths around exophytic renal tumors with a clinically relevant resection margin. Leveraging point cloud observations, the system handles irregular tumor shapes and distinguishes healthy from tumorous tissue based on near-infrared imaging, akin to indocyanine green staining in partial nephrectomy. Tissue-mimicking phantoms are crucial for the development of autonomous robotic surgical systems for interventions where acquiring ex-vivo animal tissue is infeasible, such as cancer of the kidney and renal pelvis. To this end, we propose novel hydrogel-based kidney phantoms with exophytic tumors that mimic the physical and visual behavior of tissue, and are compatible with electrosurgical instruments, a common limitation of silicone-based phantoms. In contrast to previous hydrogel phantoms, we mix the material with near-infrared dye to enable fluorescence-guided tumor segmentation. Autonomous real-world robotic experiments validate our system and phantoms, achieving an average margin accuracy of 1.44 mm in a completion time of 69 sec.
A Surgical Platform for Intracerebral Hemorrhage Robotic Evacuation (ASPIHRE): A Non-metallic MR-guided Concentric Tube Robot
Jun 20, 2022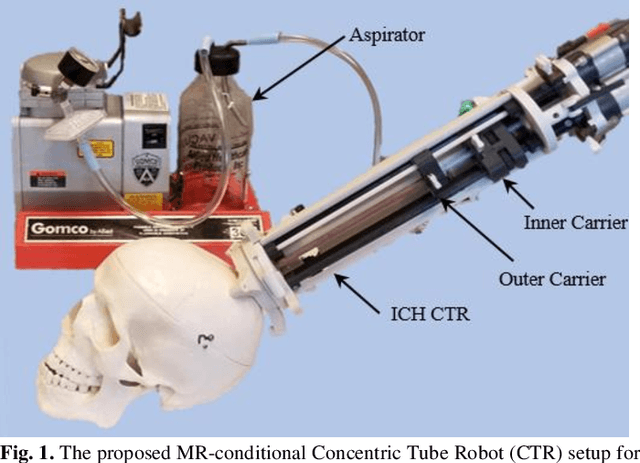
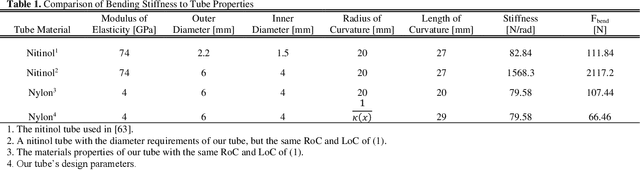
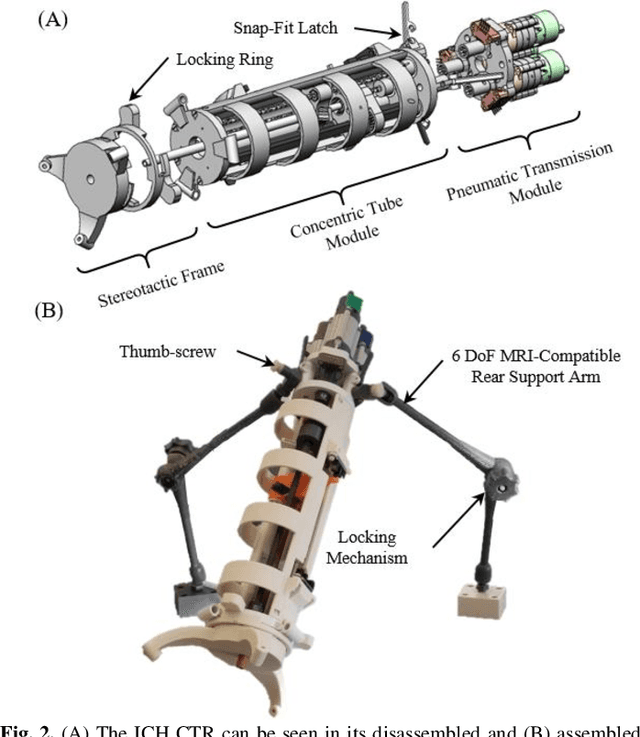
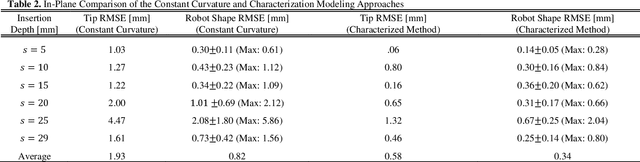
Abstract:Intracerebral hemorrhage (ICH) is the deadliest stroke sub-type, with a one-month mortality rate as high as 52%. Due to the potential cortical disruption caused by craniotomy, conservative management (watchful waiting) has historically been a common method of treatment. Minimally invasive evacuation has recently become an accepted method of treatment for patients with deep-seated hematoma 30-50 mL in volume, but proper visualization and tool dexterity remain constrained in conventional endoscopic approaches, particularly with larger hematoma volumes (> 50 mL). In this article we describe the development of ASPIHRE (A Surgical Platform for Intracerebral Hemorrhage Robotic Evacuation), the first-ever concentric tube robot that uses off-the-shelf plastic tubes for MR-guided ICH evacuation, improving tool dexterity and procedural visualization. The robot kinematics model is developed based on a calibration-based method and tube mechanics modeling, allowing the models to consider both variable curvature and torsional deflection. The MR-safe pneumatic motors are controlled using a variable gain PID algorithm producing a rotational accuracy of 0.317 +/- 0.3 degrees. The hardware and theoretical models are validated in a series of systematic bench-top and MRI experiments resulting in positional accuracy of the tube tip of 1.39 +\- 0.54 mm. Following validation of targeting accuracy, the evacuation efficacy of the robot was tested in an MR-guided phantom clot evacuation experiment. The robot was able to evacuate an initially 38.36 mL clot in 5 minutes, leaving a residual hematoma of 8.14 mL, well below the 15 mL guideline suggesting good post-ICH evacuation clinical outcomes.
Surgical Data Science -- from Concepts to Clinical Translation
Oct 30, 2020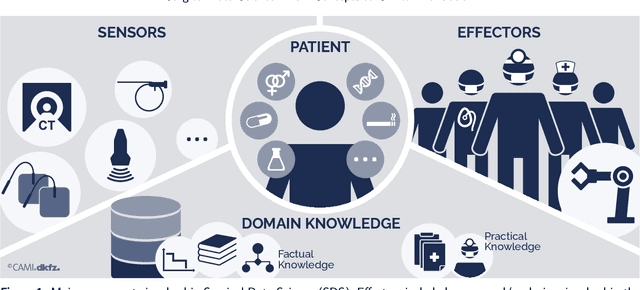
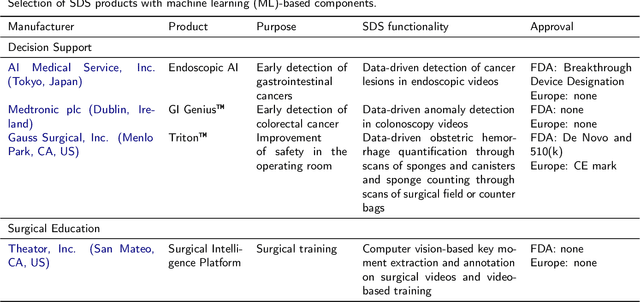
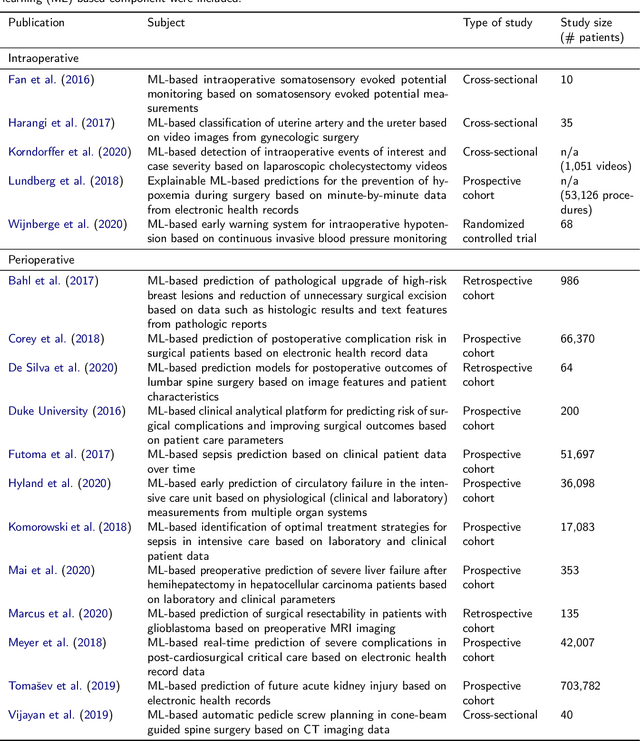
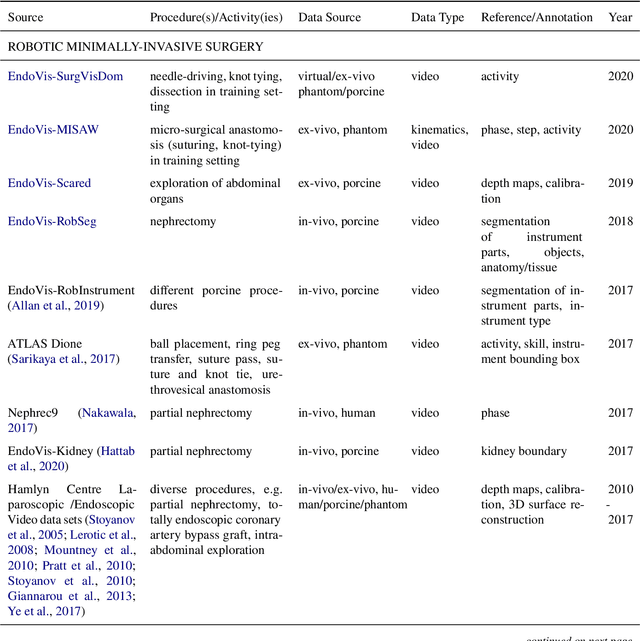
Abstract:Recent developments in data science in general and machine learning in particular have transformed the way experts envision the future of surgery. Surgical data science is a new research field that aims to improve the quality of interventional healthcare through the capture, organization, analysis and modeling of data. While an increasing number of data-driven approaches and clinical applications have been studied in the fields of radiological and clinical data science, translational success stories are still lacking in surgery. In this publication, we shed light on the underlying reasons and provide a roadmap for future advances in the field. Based on an international workshop involving leading researchers in the field of surgical data science, we review current practice, key achievements and initiatives as well as available standards and tools for a number of topics relevant to the field, namely (1) technical infrastructure for data acquisition, storage and access in the presence of regulatory constraints, (2) data annotation and sharing and (3) data analytics. Drawing from this extensive review, we present current challenges for technology development and (4) describe a roadmap for faster clinical translation and exploitation of the full potential of surgical data science.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge