Emma Chen
Slm-mux: Orchestrating small language models for reasoning
Oct 06, 2025Abstract:With the rapid development of language models, the number of small language models (SLMs) has grown significantly. Although they do not achieve state-of-the-art accuracy, they are more efficient and often excel at specific tasks. This raises a natural question: can multiple SLMs be orchestrated into a system where each contributes effectively, achieving higher accuracy than any individual model? Existing orchestration methods have primarily targeted frontier models (e.g., GPT-4) and perform suboptimally when applied to SLMs. To address this gap, we propose a three-stage approach for orchestrating SLMs. First, we introduce SLM-MUX, a multi-model architecture that effectively coordinates multiple SLMs. Building on this, we develop two optimization strategies: (i) a model selection search that identifies the most complementary SLMs from a given pool, and (ii) test-time scaling tailored to SLM-MUX. Our approach delivers strong results: Compared to existing orchestration methods, our approach achieves up to 13.4% improvement on MATH, 8.8% on GPQA, and 7.0% on GSM8K. With just two SLMS, SLM-MUX outperforms Qwen 2.5 72B on GPQA and GSM8K, and matches its performance on MATH. We further provide theoretical analyses to substantiate the advantages of our method. In summary, we demonstrate that SLMs can be effectively orchestrated into more accurate and efficient systems through the proposed approach.
Lifetime-Aware Design of Item-Level Intelligence
Sep 09, 2025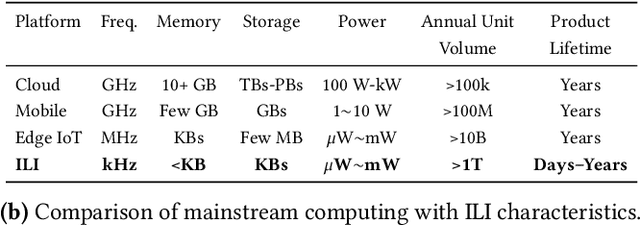
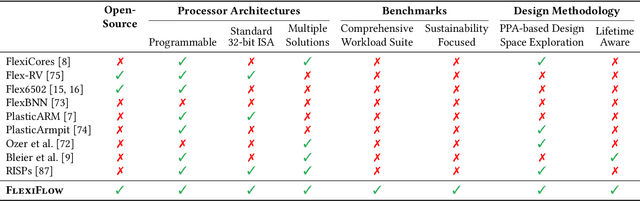

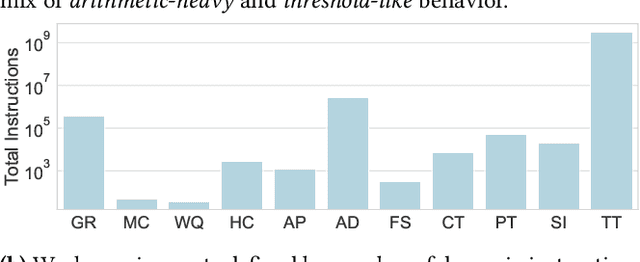
Abstract:We present FlexiFlow, a lifetime-aware design framework for item-level intelligence (ILI) where computation is integrated directly into disposable products like food packaging and medical patches. Our framework leverages natively flexible electronics which offer significantly lower costs than silicon but are limited to kHz speeds and several thousands of gates. Our insight is that unlike traditional computing with more uniform deployment patterns, ILI applications exhibit 1000X variation in operational lifetime, fundamentally changing optimal architectural design decisions when considering trillion-item deployment scales. To enable holistic design and optimization, we model the trade-offs between embodied carbon footprint and operational carbon footprint based on application-specific lifetimes. The framework includes: (1) FlexiBench, a workload suite targeting sustainability applications from spoilage detection to health monitoring; (2) FlexiBits, area-optimized RISC-V cores with 1/4/8-bit datapaths achieving 2.65X to 3.50X better energy efficiency per workload execution; and (3) a carbon-aware model that selects optimal architectures based on deployment characteristics. We show that lifetime-aware microarchitectural design can reduce carbon footprint by 1.62X, while algorithmic decisions can reduce carbon footprint by 14.5X. We validate our approach through the first tape-out using a PDK for flexible electronics with fully open-source tools, achieving 30.9kHz operation. FlexiFlow enables exploration of computing at the Extreme Edge where conventional design methodologies must be reevaluated to account for new constraints and considerations.
FactCheXcker: Mitigating Measurement Hallucinations in Chest X-ray Report Generation Models
Nov 27, 2024



Abstract:Medical vision-language model models often struggle with generating accurate quantitative measurements in radiology reports, leading to hallucinations that undermine clinical reliability. We introduce FactCheXcker, a modular framework that de-hallucinates radiology report measurements by leveraging an improved query-code-update paradigm. Specifically, FactCheXcker employs specialized modules and the code generation capabilities of large language models to solve measurement queries generated based on the original report. After extracting measurable findings, the results are incorporated into an updated report. We evaluate FactCheXcker on endotracheal tube placement, which accounts for an average of 78% of report measurements, using the MIMIC-CXR dataset and 11 medical report-generation models. Our results show that FactCheXcker significantly reduces hallucinations, improves measurement precision, and maintains the quality of the original reports. Specifically, FactCheXcker improves the performance of all 11 models and achieves an average improvement of 94.0% in reducing measurement hallucinations measured by mean absolute error.
Multimodal Clinical Benchmark for Emergency Care (MC-BEC): A Comprehensive Benchmark for Evaluating Foundation Models in Emergency Medicine
Nov 07, 2023Abstract:We propose the Multimodal Clinical Benchmark for Emergency Care (MC-BEC), a comprehensive benchmark for evaluating foundation models in Emergency Medicine using a dataset of 100K+ continuously monitored Emergency Department visits from 2020-2022. MC-BEC focuses on clinically relevant prediction tasks at timescales from minutes to days, including predicting patient decompensation, disposition, and emergency department (ED) revisit, and includes a standardized evaluation framework with train-test splits and evaluation metrics. The multimodal dataset includes a wide range of detailed clinical data, including triage information, prior diagnoses and medications, continuously measured vital signs, electrocardiogram and photoplethysmograph waveforms, orders placed and medications administered throughout the visit, free-text reports of imaging studies, and information on ED diagnosis, disposition, and subsequent revisits. We provide performance baselines for each prediction task to enable the evaluation of multimodal, multitask models. We believe that MC-BEC will encourage researchers to develop more effective, generalizable, and accessible foundation models for multimodal clinical data.
Machine Learning Sensors
Jun 07, 2022
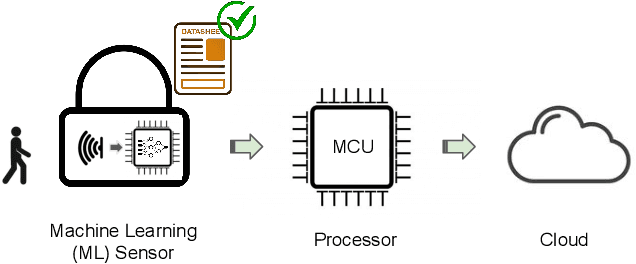
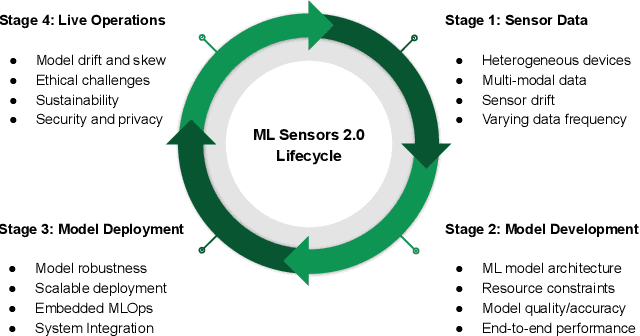
Abstract:Machine learning sensors represent a paradigm shift for the future of embedded machine learning applications. Current instantiations of embedded machine learning (ML) suffer from complex integration, lack of modularity, and privacy and security concerns from data movement. This article proposes a more data-centric paradigm for embedding sensor intelligence on edge devices to combat these challenges. Our vision for "sensor 2.0" entails segregating sensor input data and ML processing from the wider system at the hardware level and providing a thin interface that mimics traditional sensors in functionality. This separation leads to a modular and easy-to-use ML sensor device. We discuss challenges presented by the standard approach of building ML processing into the software stack of the controlling microprocessor on an embedded system and how the modularity of ML sensors alleviates these problems. ML sensors increase privacy and accuracy while making it easier for system builders to integrate ML into their products as a simple component. We provide examples of prospective ML sensors and an illustrative datasheet as a demonstration and hope that this will build a dialogue to progress us towards sensor 2.0.
CheXbreak: Misclassification Identification for Deep Learning Models Interpreting Chest X-rays
Mar 24, 2021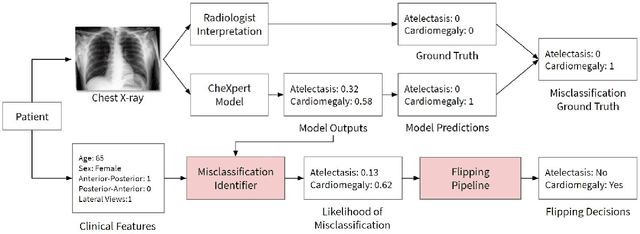
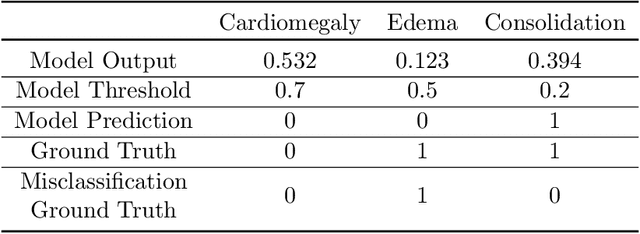
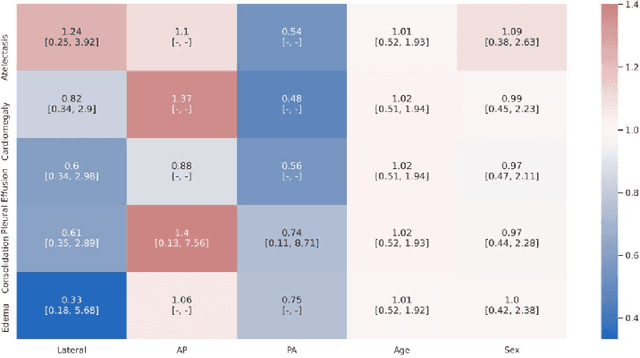
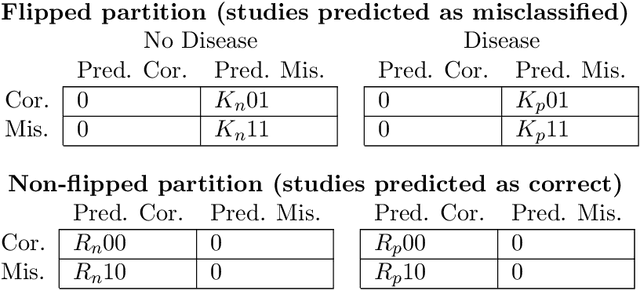
Abstract:A major obstacle to the integration of deep learning models for chest x-ray interpretation into clinical settings is the lack of understanding of their failure modes. In this work, we first investigate whether there are patient subgroups that chest x-ray models are likely to misclassify. We find that patient age and the radiographic finding of lung lesion, pneumothorax or support devices are statistically relevant features for predicting misclassification for some chest x-ray models. Second, we develop misclassification predictors on chest x-ray models using their outputs and clinical features. We find that our best performing misclassification identifier achieves an AUROC close to 0.9 for most diseases. Third, employing our misclassification identifiers, we develop a corrective algorithm to selectively flip model predictions that have high likelihood of misclassification at inference time. We observe F1 improvement on the prediction of Consolidation (0.008 [95\% CI 0.005, 0.010]) and Edema (0.003, [95\% CI 0.001, 0.006]). By carrying out our investigation on ten distinct and high-performing chest x-ray models, we are able to derive insights across model architectures and offer a generalizable framework applicable to other medical imaging tasks.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge