Ingerid Reinertsen
A unified FLAIR hyperintensity segmentation model for various CNS tumor types and acquisition time points
Dec 19, 2025Abstract:T2-weighted fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) scans are important for diagnosis, treatment planning and monitoring of brain tumors. Depending on the brain tumor type, the FLAIR hyperintensity volume is an important measure to asses the tumor volume or surrounding edema, and an automatic segmentation of this would be useful in the clinic. In this study, around 5000 FLAIR images of various tumors types and acquisition time points from different centers were used to train a unified FLAIR hyperintensity segmentation model using an Attention U-Net architecture. The performance was compared against dataset specific models, and was validated on different tumor types, acquisition time points and against BraTS. The unified model achieved an average Dice score of 88.65\% for pre-operative meningiomas, 80.08% for pre-operative metastasis, 90.92% for pre-operative and 84.60% for post-operative gliomas from BraTS, and 84.47% for pre-operative and 61.27\% for post-operative lower grade gliomas. In addition, the results showed that the unified model achieved comparable segmentation performance to the dataset specific models on their respective datasets, and enables generalization across tumor types and acquisition time points, which facilitates the deployment in a clinical setting. The model is integrated into Raidionics, an open-source software for CNS tumor analysis.
Automatic and standardized surgical reporting for central nervous system tumors
Aug 12, 2025Abstract:Magnetic resonance (MR) imaging is essential for evaluating central nervous system (CNS) tumors, guiding surgical planning, treatment decisions, and assessing postoperative outcomes and complication risks. While recent work has advanced automated tumor segmentation and report generation, most efforts have focused on preoperative data, with limited attention to postoperative imaging analysis. This study introduces a comprehensive pipeline for standardized postsurtical reporting in CNS tumors. Using the Attention U-Net architecture, segmentation models were trained for the preoperative (non-enhancing) tumor core, postoperative contrast-enhancing residual tumor, and resection cavity. Additionally, MR sequence classification and tumor type identification for contrast-enhancing lesions were explored using the DenseNet architecture. The models were integrated into a reporting pipeline, following the RANO 2.0 guidelines. Training was conducted on multicentric datasets comprising 2000 to 7000 patients, using a 5-fold cross-validation. Evaluation included patient-, voxel-, and object-wise metrics, with benchmarking against the latest BraTS challenge results. The segmentation models achieved average voxel-wise Dice scores of 87%, 66%, 70%, and 77% for the tumor core, non-enhancing tumor core, contrast-enhancing residual tumor, and resection cavity, respectively. Classification models reached 99.5% balanced accuracy in MR sequence classification and 80% in tumor type classification. The pipeline presented in this study enables robust, automated segmentation, MR sequence classification, and standardized report generation aligned with RANO 2.0 guidelines, enhancing postoperative evaluation and clinical decision-making. The proposed models and methods were integrated into Raidionics, open-source software platform for CNS tumor analysis, now including a dedicated module for postsurgical analysis.
Automatic brain tumor segmentation in 2D intra-operative ultrasound images using MRI tumor annotations
Nov 21, 2024



Abstract:Automatic segmentation of brain tumors in intra-operative ultrasound (iUS) images could facilitate localization of tumor tissue during resection surgery. The lack of large annotated datasets limits the current models performances. In this paper, we investigate the use of tumor annotations in pre-operative MRI images, which are more easily accessible than annotations in iUS images, for training of deep learning models for iUS brain tumor segmentation. We used 180 annotated pre-operative MRI images with corresponding unannotated iUS images, and 29 annotated iUS images. Image registration was performed to transfer the MRI annotations to the corresponding iUS images before training models with the nnU-Net framework. To validate the use of MRI labels, the models were compared to a model trained with only US annotated tumors, and a model with both US and MRI annotated tumors. In addition, the results were compared to annotations validated by an expert neurosurgeon on the same test set to measure inter-observer variability. The results showed similar performance for a model trained with only MRI annotated tumors, compared to a model trained with only US annotated tumors. The model trained using both modalities obtained slightly better results with an average Dice score of 0.62, where external expert annotations achieved a score of 0.67. The results also showed that the deep learning models were comparable to expert annotation for larger tumors (> 200 mm2), but perform clearly worse for smaller tumors (< 200 mm2). This shows that MRI tumor annotations can be used as a substitute for US tumor annotations to train a deep learning model for automatic brain tumor segmentation in intra-operative ultrasound images. Small tumors is a limitation for the current models and will be the focus of future work. The main models are available here: https://github.com/mathildefaanes/us_brain_tumor_segmentation.
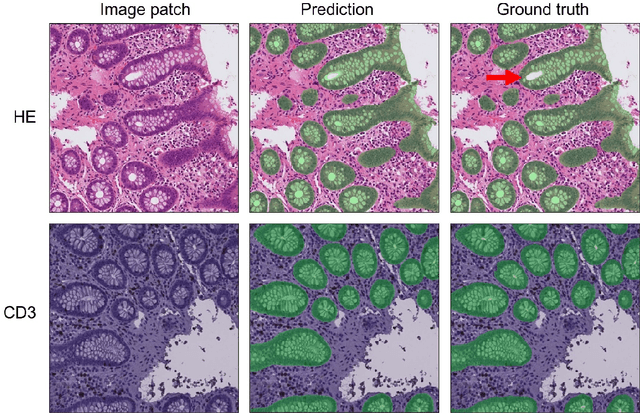
Immunohistochemistry guided segmentation of benign epithelial cells, in situ lesions, and invasive epithelial cells in breast cancer slides
Nov 22, 2023Abstract:Digital pathology enables automatic analysis of histopathological sections using artificial intelligence (AI). Automatic evaluation could improve diagnostic efficiency and help find associations between morphological features and clinical outcome. For development of such prediction models, identifying invasive epithelial cells, and separating these from benign epithelial cells and in situ lesions would be the first step. In this study, we aimed to develop an AI model for segmentation of epithelial cells in sections from breast cancer. We generated epithelial ground truth masks by restaining hematoxylin and eosin (HE) sections with cytokeratin (CK) AE1/AE3, and by pathologists' annotations. HE/CK image pairs were used to train a convolutional neural network, and data augmentation was used to make the model more robust. Tissue microarrays (TMAs) from 839 patients, and whole slide images from two patients were used for training and evaluation of the models. The sections were derived from four cohorts of breast cancer patients. TMAs from 21 patients from a fifth cohort was used as a second test set. In quantitative evaluation, a mean Dice score of 0.70, 0.79, and 0.75 for invasive epithelial cells, benign epithelial cells, and in situ lesions, respectively, were achieved. In qualitative scoring (0-5) by pathologists, results were best for all epithelium and invasive epithelium, with scores of 4.7 and 4.4. Scores for benign epithelium and in situ lesions were 3.7 and 2.0. The proposed model segmented epithelial cells in HE stained breast cancer slides well, but further work is needed for accurate division between the classes. Immunohistochemistry, together with pathologists' annotations, enabled the creation of accurate ground truths. The model is made freely available in FastPathology and the code is available at https://github.com/AICAN-Research/breast-epithelium-segmentation
Segmentation of glioblastomas in early post-operative multi-modal MRI with deep neural networks
Apr 18, 2023Abstract:Extent of resection after surgery is one of the main prognostic factors for patients diagnosed with glioblastoma. To achieve this, accurate segmentation and classification of residual tumor from post-operative MR images is essential. The current standard method for estimating it is subject to high inter- and intra-rater variability, and an automated method for segmentation of residual tumor in early post-operative MRI could lead to a more accurate estimation of extent of resection. In this study, two state-of-the-art neural network architectures for pre-operative segmentation were trained for the task. The models were extensively validated on a multicenter dataset with nearly 1000 patients, from 12 hospitals in Europe and the United States. The best performance achieved was a 61\% Dice score, and the best classification performance was about 80\% balanced accuracy, with a demonstrated ability to generalize across hospitals. In addition, the segmentation performance of the best models was on par with human expert raters. The predicted segmentations can be used to accurately classify the patients into those with residual tumor, and those with gross total resection.
RESECT-SEG: Open access annotations of intra-operative brain tumor ultrasound images
Jul 13, 2022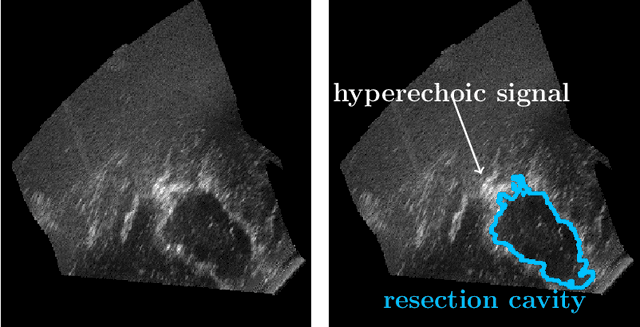
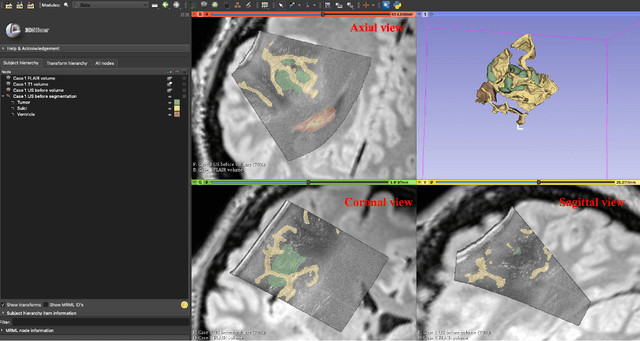
Abstract:Purpose: Registration and segmentation of magnetic resonance (MR) and ultrasound (US) images play an essential role in surgical planning and resection of brain tumors. However, validating these techniques is challenging due to the scarcity of publicly accessible sources with high-quality ground truth information. To this end, we propose a unique annotation dataset of tumor tissues and resection cavities from the previously published RESECT dataset (Xiao et al. 2017) to encourage a more rigorous assessments of image processing techniques. Acquisition and validation methods: The RESECT database consists of MR and intraoperative US (iUS) images of 23 patients who underwent resection surgeries. The proposed dataset contains tumor tissues and resection cavity annotations of the iUS images. The quality of annotations were validated by two highly experienced neurosurgeons through several assessment criteria. Data format and availability: Annotations of tumor tissues and resection cavities are provided in 3D NIFTI formats. Both sets of annotations are accessible online in the \url{https://osf.io/6y4db}. Discussion and potential applications: The proposed database includes tumor tissue and resection cavity annotations from real-world clinical ultrasound brain images to evaluate segmentation and registration methods. These labels could also be used to train deep learning approaches. Eventually, this dataset should further improve the quality of image guidance in neurosurgery.
Learn2Reg: comprehensive multi-task medical image registration challenge, dataset and evaluation in the era of deep learning
Dec 23, 2021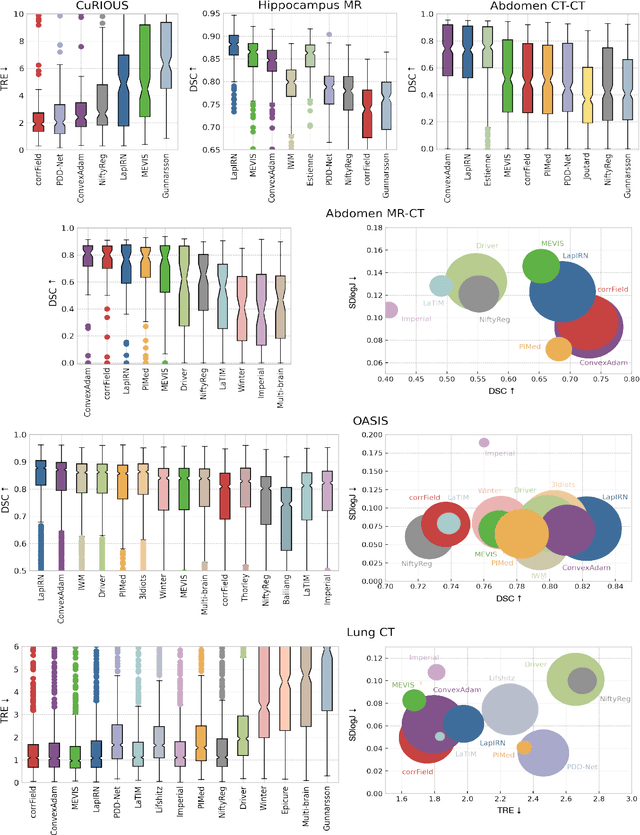
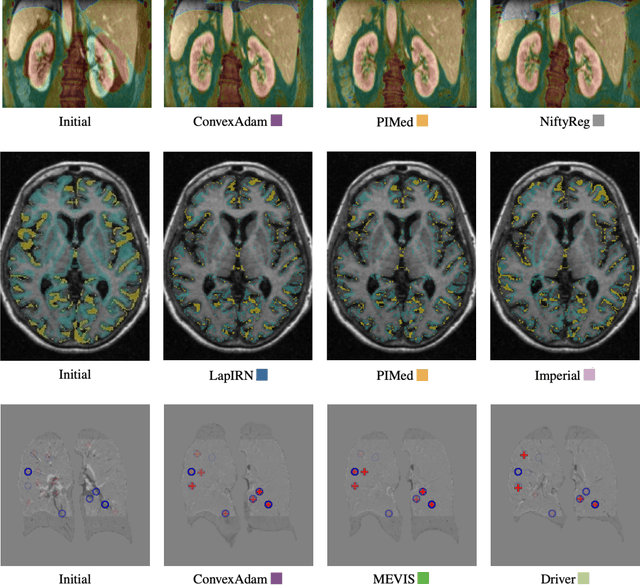
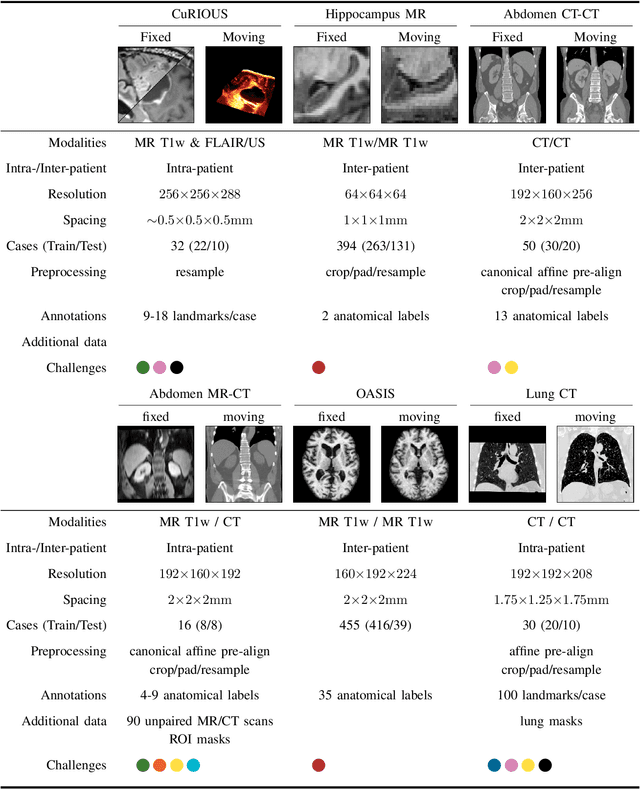
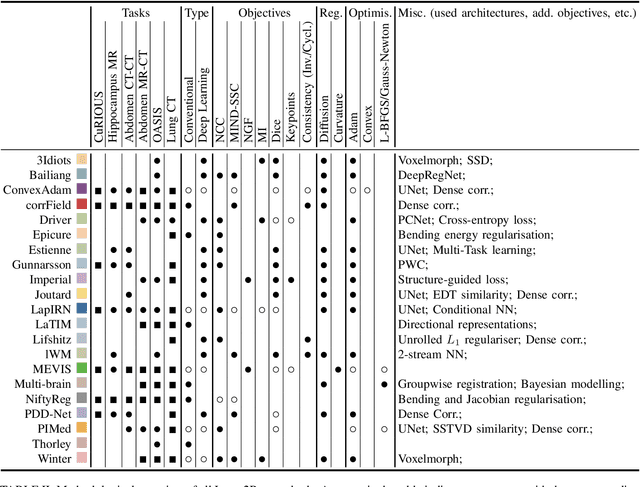
Abstract:Image registration is a fundamental medical image analysis task, and a wide variety of approaches have been proposed. However, only a few studies have comprehensively compared medical image registration approaches on a wide range of clinically relevant tasks, in part because of the lack of availability of such diverse data. This limits the development of registration methods, the adoption of research advances into practice, and a fair benchmark across competing approaches. The Learn2Reg challenge addresses these limitations by providing a multi-task medical image registration benchmark for comprehensive characterisation of deformable registration algorithms. A continuous evaluation will be possible at https://learn2reg.grand-challenge.org. Learn2Reg covers a wide range of anatomies (brain, abdomen, and thorax), modalities (ultrasound, CT, MR), availability of annotations, as well as intra- and inter-patient registration evaluation. We established an easily accessible framework for training and validation of 3D registration methods, which enabled the compilation of results of over 65 individual method submissions from more than 20 unique teams. We used a complementary set of metrics, including robustness, accuracy, plausibility, and runtime, enabling unique insight into the current state-of-the-art of medical image registration. This paper describes datasets, tasks, evaluation methods and results of the challenge, and the results of further analysis of transferability to new datasets, the importance of label supervision, and resulting bias.
Hybrid guiding: A multi-resolution refinement approach for semantic segmentation of gigapixel histopathological images
Dec 07, 2021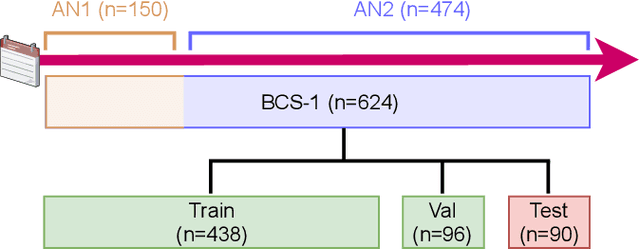
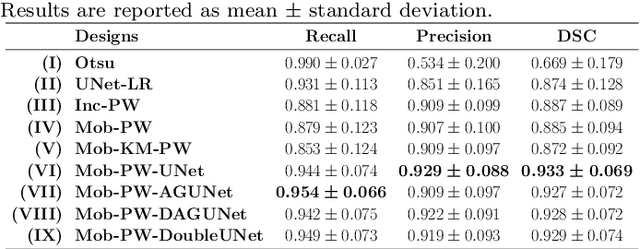
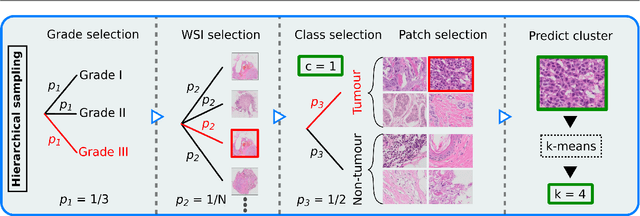
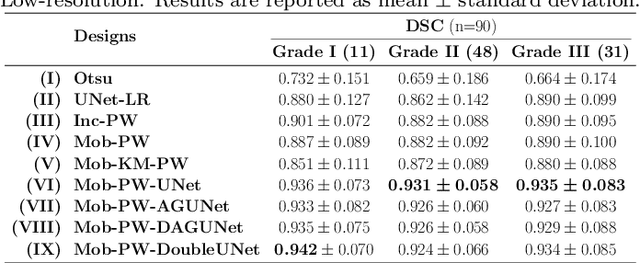
Abstract:Histopathological cancer diagnostics has become more complex, and the increasing number of biopsies is a challenge for most pathology laboratories. Thus, development of automatic methods for evaluation of histopathological cancer sections would be of value. In this study, we used 624 whole slide images (WSIs) of breast cancer from a Norwegian cohort. We propose a cascaded convolutional neural network design, called H2G-Net, for semantic segmentation of gigapixel histopathological images. The design involves a detection stage using a patch-wise method, and a refinement stage using a convolutional autoencoder. To validate the design, we conducted an ablation study to assess the impact of selected components in the pipeline on tumour segmentation. Guiding segmentation, using hierarchical sampling and deep heatmap refinement, proved to be beneficial when segmenting the histopathological images. We found a significant improvement when using a refinement network for postprocessing the generated tumour segmentation heatmaps. The overall best design achieved a Dice score of 0.933 on an independent test set of 90 WSIs. The design outperformed single-resolution approaches, such as cluster-guided, patch-wise high-resolution classification using MobileNetV2 (0.872) and a low-resolution U-Net (0.874). In addition, segmentation on a representative x400 WSI took ~58 seconds, using only the CPU. The findings demonstrate the potential of utilizing a refinement network to improve patch-wise predictions. The solution is efficient and does not require overlapping patch inference or ensembling. Furthermore, we showed that deep neural networks can be trained using a random sampling scheme that balances on multiple different labels simultaneously, without the need of storing patches on disk. Future work should involve more efficient patch generation and sampling, as well as improved clustering.
Code-free development and deployment of deep segmentation models for digital pathology
Nov 16, 2021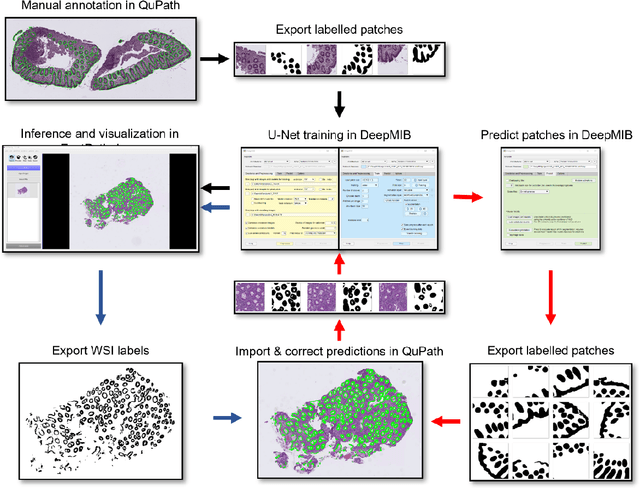
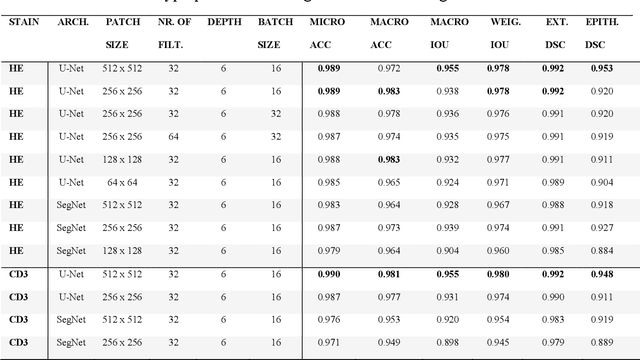
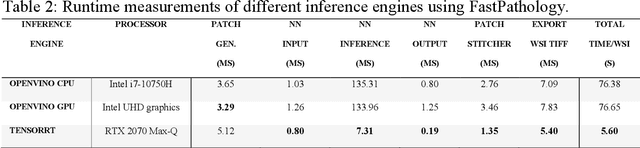
Abstract:Application of deep learning on histopathological whole slide images (WSIs) holds promise of improving diagnostic efficiency and reproducibility but is largely dependent on the ability to write computer code or purchase commercial solutions. We present a code-free pipeline utilizing free-to-use, open-source software (QuPath, DeepMIB, and FastPathology) for creating and deploying deep learning-based segmentation models for computational pathology. We demonstrate the pipeline on a use case of separating epithelium from stroma in colonic mucosa. A dataset of 251 annotated WSIs, comprising 140 hematoxylin-eosin (HE)-stained and 111 CD3 immunostained colon biopsy WSIs, were developed through active learning using the pipeline. On a hold-out test set of 36 HE and 21 CD3-stained WSIs a mean intersection over union score of 96.6% and 95.3% was achieved on epithelium segmentation. We demonstrate pathologist-level segmentation accuracy and clinical acceptable runtime performance and show that pathologists without programming experience can create near state-of-the-art segmentation solutions for histopathological WSIs using only free-to-use software. The study further demonstrates the strength of open-source solutions in its ability to create generalizable, open pipelines, of which trained models and predictions can seamlessly be exported in open formats and thereby used in external solutions. All scripts, trained models, a video tutorial, and the full dataset of 251 WSIs with ~31k epithelium annotations are made openly available at https://github.com/andreped/NoCodeSeg to accelerate research in the field.
Meningioma segmentation in T1-weighted MRI leveraging global context and attention mechanisms
Jan 19, 2021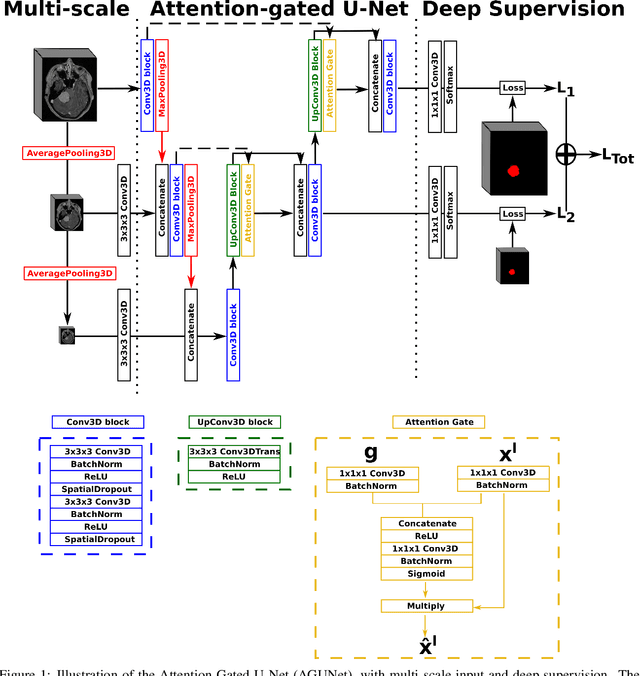
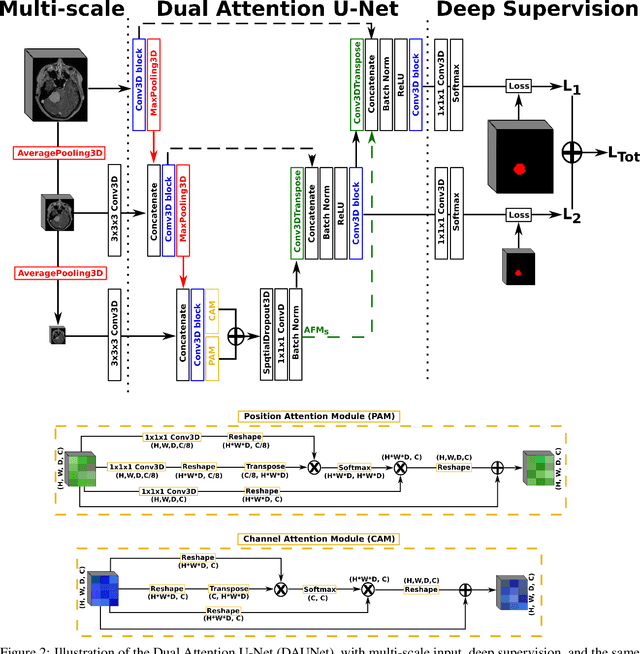
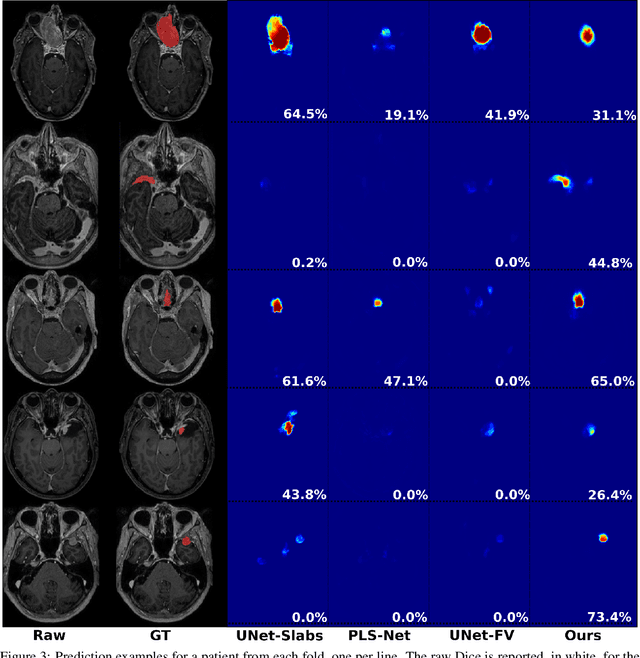
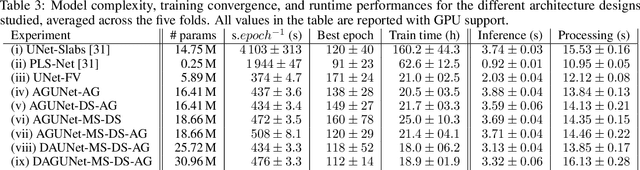
Abstract:Meningiomas are the most common type of primary brain tumor, accounting for approximately 30% of all brain tumors. A substantial number of these tumors are never surgically removed but rather monitored over time. Automatic and precise meningioma segmentation is therefore beneficial to enable reliable growth estimation and patient-specific treatment planning. In this study, we propose the inclusion of attention mechanisms over a U-Net architecture: (i) Attention-gated U-Net (AGUNet) and (ii) Dual Attention U-Net (DAUNet), using a 3D MRI volume as input. Attention has the potential to leverage the global context and identify features' relationships across the entire volume. To limit spatial resolution degradation and loss of detail inherent to encoder-decoder architectures, we studied the impact of multi-scale input and deep supervision components. The proposed architectures are trainable end-to-end and each concept can be seamlessly disabled for ablation studies. The validation studies were performed using a 5-fold cross validation over 600 T1-weighted MRI volumes from St. Olavs University Hospital, Trondheim, Norway. For the best performing architecture, an average Dice score of 81.6% was reached for an F1-score of 95.6%. With an almost perfect precision of 98%, meningiomas smaller than 3ml were occasionally missed hence reaching an overall recall of 93%. Leveraging global context from a 3D MRI volume provided the best performances, even if the native volume resolution could not be processed directly. Overall, near-perfect detection was achieved for meningiomas larger than 3ml which is relevant for clinical use. In the future, the use of multi-scale designs and refinement networks should be further investigated to improve the performance. A larger number of cases with meningiomas below 3ml might also be needed to improve the performance for the smallest tumors.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge