Johanna Vanel
Mediastinal lymph nodes segmentation using 3D convolutional neural network ensembles and anatomical priors guiding
Feb 11, 2021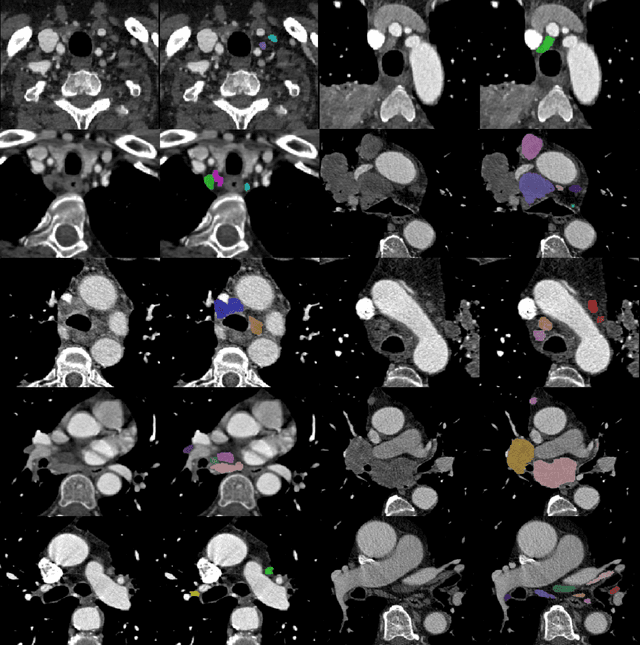
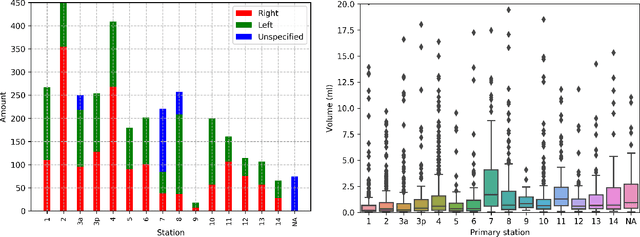
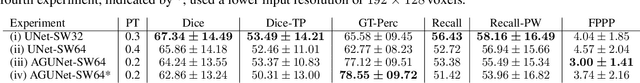
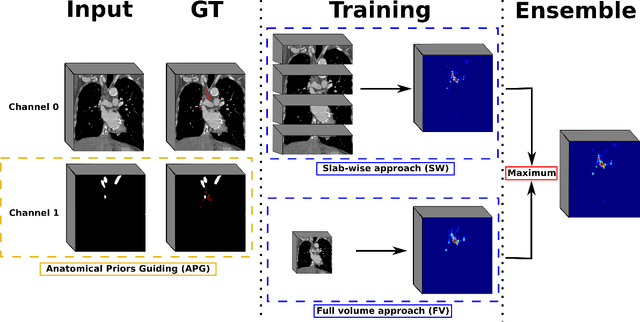
Abstract:As lung cancer evolves, the presence of enlarged and potentially malignant lymph nodes must be assessed to properly estimate disease progression and select the best treatment strategy. Following the clinical guidelines, estimation of short-axis diameter and mediastinum station are paramount for correct diagnosis. A method for accurate and automatic segmentation is hence decisive for quantitatively describing lymph nodes. In this study, the use of 3D convolutional neural networks, either through slab-wise schemes or the leveraging of downsampled entire volumes, is investigated. Furthermore, the potential impact from simple ensemble strategies is considered. As lymph nodes have similar attenuation values to nearby anatomical structures, we suggest using the knowledge of other organs as prior information to guide the segmentation task. To assess the segmentation and instance detection performances, a 5-fold cross-validation strategy was followed over a dataset of 120 contrast-enhanced CT volumes. For the 1178 lymph nodes with a short-axis diameter $\geq10$ mm, our best performing approach reached a patient-wise recall of 92%, a false positive per patient ratio of 5, and a segmentation overlap of 80.5%. The method performs similarly well across all stations. Fusing a slab-wise and a full volume approach within an ensemble scheme generated the best performances. The anatomical priors guiding strategy is promising, yet a larger set than four organs appears needed to generate an optimal benefit. A larger dataset is also mandatory, given the wide range of expressions a lymph node can exhibit (i.e., shape, location, and attenuation), and contrast uptake variations.
Fast meningioma segmentation in T1-weighted MRI volumes using a lightweight 3D deep learning architecture
Oct 14, 2020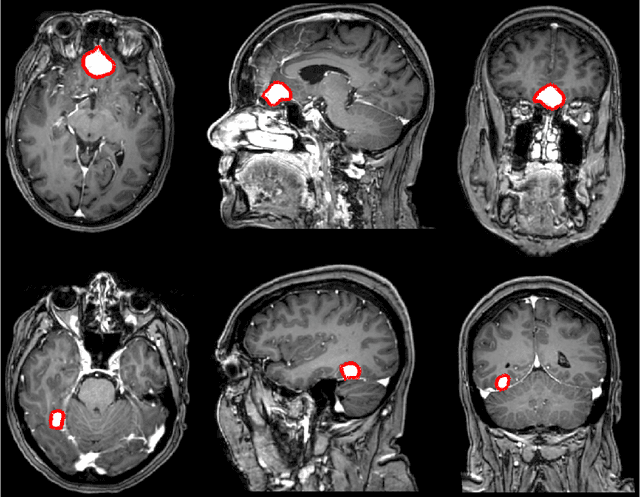
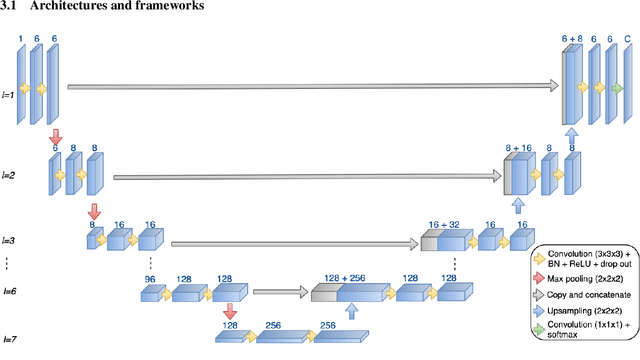
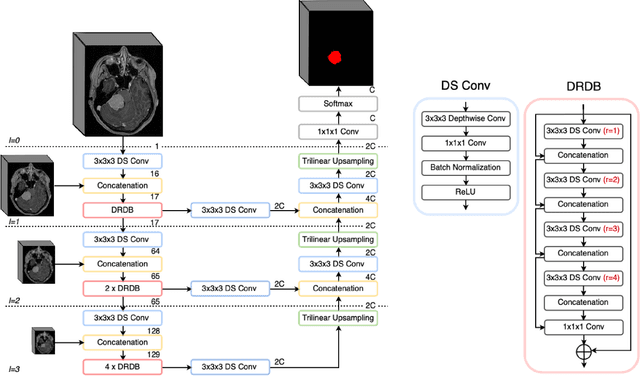
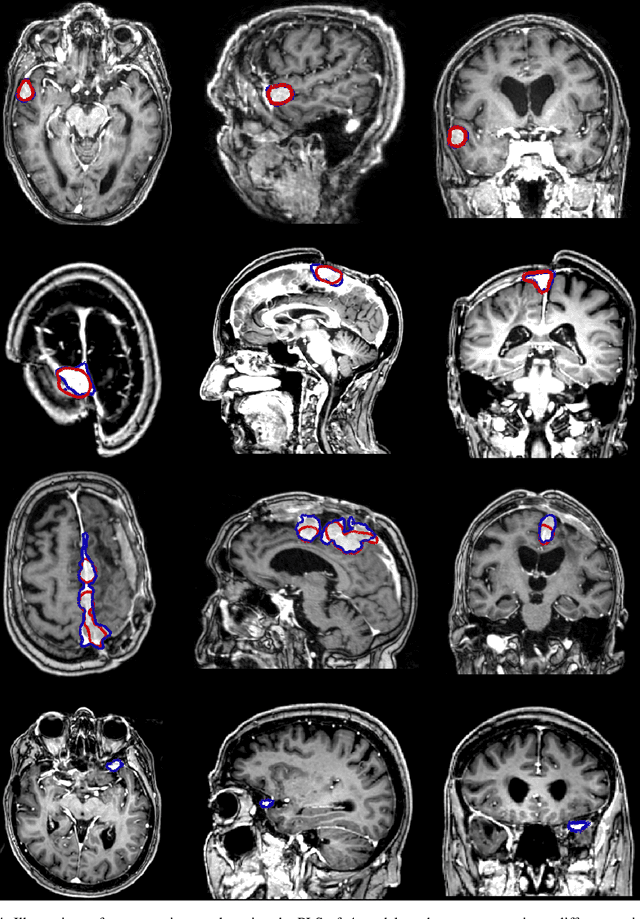
Abstract:Automatic and consistent meningioma segmentation in T1-weighted MRI volumes and corresponding volumetric assessment is of use for diagnosis, treatment planning, and tumor growth evaluation. In this paper, we optimized the segmentation and processing speed performances using a large number of both surgically treated meningiomas and untreated meningiomas followed at the outpatient clinic. We studied two different 3D neural network architectures: (i) a simple encoder-decoder similar to a 3D U-Net, and (ii) a lightweight multi-scale architecture (PLS-Net). In addition, we studied the impact of different training schemes. For the validation studies, we used 698 T1-weighted MR volumes from St. Olav University Hospital, Trondheim, Norway. The models were evaluated in terms of detection accuracy, segmentation accuracy and training/inference speed. While both architectures reached a similar Dice score of 70% on average, the PLS-Net was more accurate with an F1-score of up to 88%. The highest accuracy was achieved for the largest meningiomas. Speed-wise, the PLS-Net architecture tended to converge in about 50 hours while 130 hours were necessary for U-Net. Inference with PLS-Net takes less than a second on GPU and about 15 seconds on CPU. Overall, with the use of mixed precision training, it was possible to train competitive segmentation models in a relatively short amount of time using the lightweight PLS-Net architecture. In the future, the focus should be brought toward the segmentation of small meningiomas (less than 2ml) to improve clinical relevance for automatic and early diagnosis as well as speed of growth estimates.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge