Leo Celi
Evaluating Progress on Machine Learning for Longitudinal Electronic Healthcare Data
Oct 02, 2020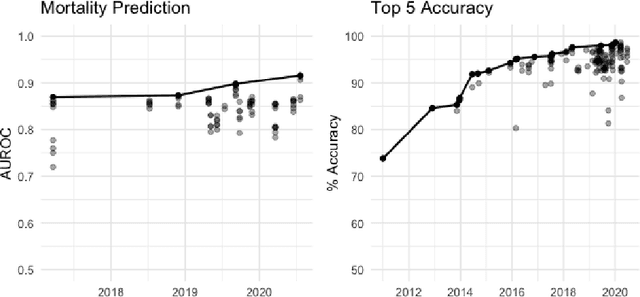
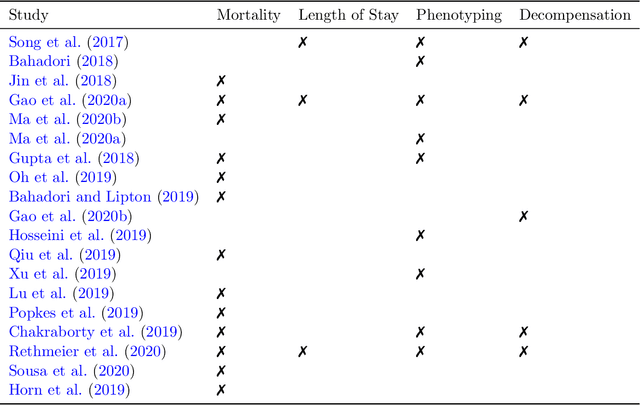
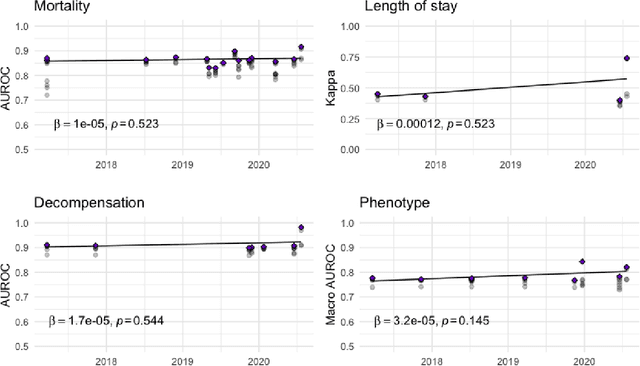
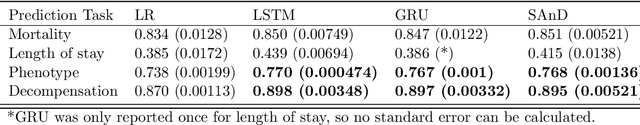
Abstract:The Large Scale Visual Recognition Challenge based on the well-known Imagenet dataset catalyzed an intense flurry of progress in computer vision. Benchmark tasks have propelled other sub-fields of machine learning forward at an equally impressive pace, but in healthcare it has primarily been image processing tasks, such as in dermatology and radiology, that have experienced similar benchmark-driven progress. In the present study, we performed a comprehensive review of benchmarks in medical machine learning for structured data, identifying one based on the Medical Information Mart for Intensive Care (MIMIC-III) that allows the first direct comparison of predictive performance and thus the evaluation of progress on four clinical prediction tasks: mortality, length of stay, phenotyping, and patient decompensation. We find that little meaningful progress has been made over a 3 year period on these tasks, despite significant community engagement. Through our meta-analysis, we find that the performance of deep recurrent models is only superior to logistic regression on certain tasks. We conclude with a synthesis of these results, possible explanations, and a list of desirable qualities for future benchmarks in medical machine learning.
Regional Tree Regularization for Interpretability in Black Box Models
Aug 13, 2019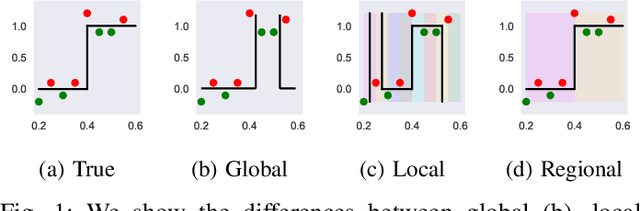
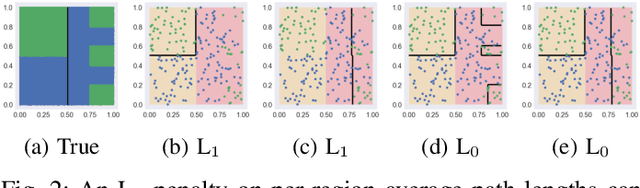
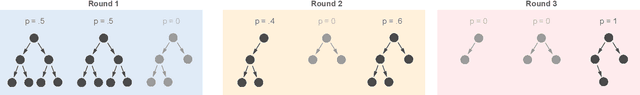
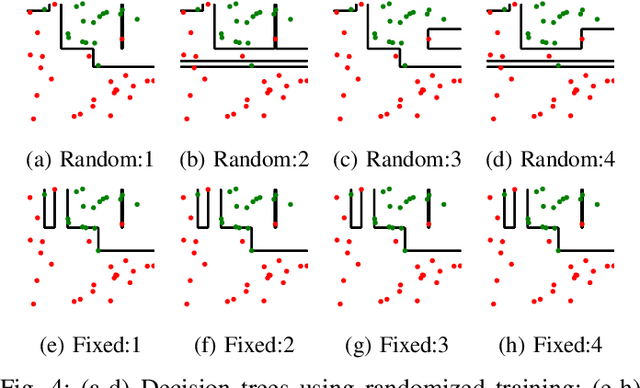
Abstract:The lack of interpretability remains a barrier to the adoption of deep neural networks. Recently, tree regularization has been proposed to encourage deep neural networks to resemble compact, axis-aligned decision trees without significant compromises in accuracy. However, it may be unreasonable to expect that a single tree can predict well across all possible inputs. In this work, we propose regional tree regularization, which encourages a deep model to be well-approximated by several separate decision trees specific to predefined regions of the input space. Practitioners can define regions based on domain knowledge of contexts where different decision-making logic is needed. Across many datasets, our approach delivers more accurate predictions than simply training separate decision trees for each region, while producing simpler explanations than other neural net regularization schemes without sacrificing predictive power. Two healthcare case studies in critical care and HIV demonstrate how experts can improve understanding of deep models via our approach.
Predicting Blood Pressure Response to Fluid Bolus Therapy Using Attention-Based Neural Networks for Clinical Interpretability
Dec 03, 2018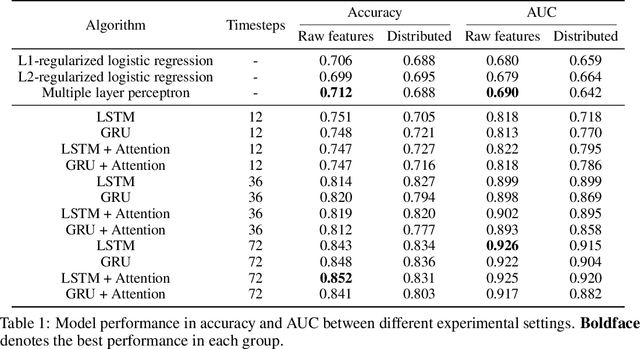
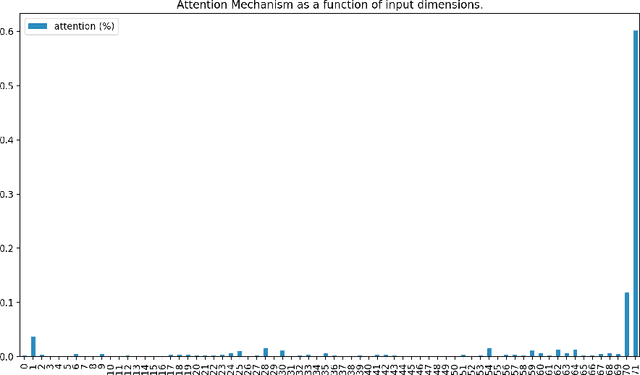
Abstract:Determining whether hypotensive patients in intensive care units (ICUs) should receive fluid bolus therapy (FBT) has been an extremely challenging task for intensive care physicians as the corresponding increase in blood pressure has been hard to predict. Our study utilized regression models and attention-based recurrent neural network (RNN) algorithms and a multi-clinical information system large-scale database to build models that can predict the successful response to FBT among hypotensive patients in ICUs. We investigated both time-aggregated modeling using logistic regression algorithms with regularization and time-series modeling using the long short term memory network (LSTM) and the gated recurrent units network (GRU) with the attention mechanism for clinical interpretability. Among all modeling strategies, the stacked LSTM with the attention mechanism yielded the most predictable model with the highest accuracy of 0.852 and area under the curve (AUC) value of 0.925. The study results may help identify hypotensive patients in ICUs who will have sufficient blood pressure recovery after FBT.
Improved survival of cancer patients admitted to the ICU between 2002 and 2011 at a U.S. teaching hospital
Aug 06, 2018Abstract:Over the past decades, both critical care and cancer care have improved substantially. Due to increased cancer-specific survival, we hypothesized that both the number of cancer patients admitted to the ICU and overall survival have increased since the millennium change. MIMIC-III, a freely accessible critical care database of Beth Israel Deaconess Medical Center, Boston, USA was used to retrospectively study trends and outcomes of cancer patients admitted to the ICU between 2002 and 2011. Multiple logistic regression analysis was performed to adjust for confounders of 28-day and 1-year mortality. Out of 41,468 unique ICU admissions, 1,100 hemato-oncologic, 3,953 oncologic and 49 patients with both a hematological and solid malignancy were analyzed. Hematological patients had higher critical illness scores than non-cancer patients, while oncologic patients had similar APACHE-III and SOFA-scores compared to non-cancer patients. In the univariate analysis, cancer was strongly associated with mortality (OR= 2.74, 95%CI: 2.56, 2.94). Over the 10-year study period, 28-day mortality of cancer patients decreased by 30%. This trend persisted after adjustment for covariates, with cancer patients having significantly higher mortality (OR=2.63, 95%CI: 2.38, 2.88). Between 2002 and 2011, both the adjusted odds of 28-day mortality and the adjusted odds of 1-year mortality for cancer patients decreased by 6% (95%CI: 4%, 9%). Having cancer was the strongest single predictor of 1-year mortality in the multivariate model (OR=4.47, 95%CI: 4.11, 4.84).
Deep Reinforcement Learning for Sepsis Treatment
Nov 27, 2017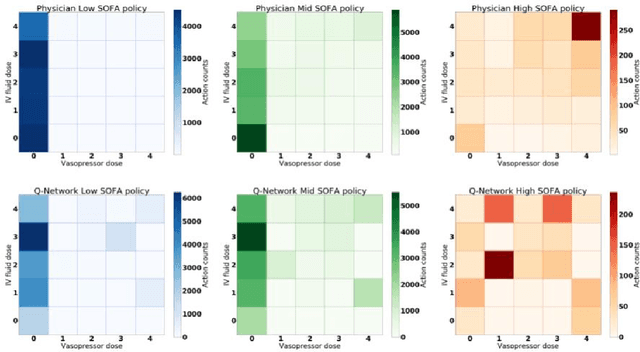

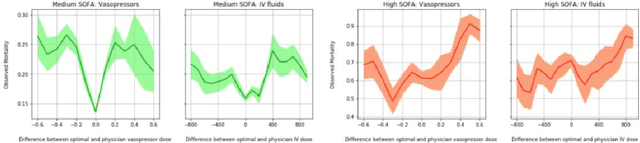
Abstract:Sepsis is a leading cause of mortality in intensive care units and costs hospitals billions annually. Treating a septic patient is highly challenging, because individual patients respond very differently to medical interventions and there is no universally agreed-upon treatment for sepsis. In this work, we propose an approach to deduce treatment policies for septic patients by using continuous state-space models and deep reinforcement learning. Our model learns clinically interpretable treatment policies, similar in important aspects to the treatment policies of physicians. The learned policies could be used to aid intensive care clinicians in medical decision making and improve the likelihood of patient survival.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge