Bernhard Fuerst
On the Effectiveness of Virtual Reality-based Training for Robotic Setup
Mar 03, 2020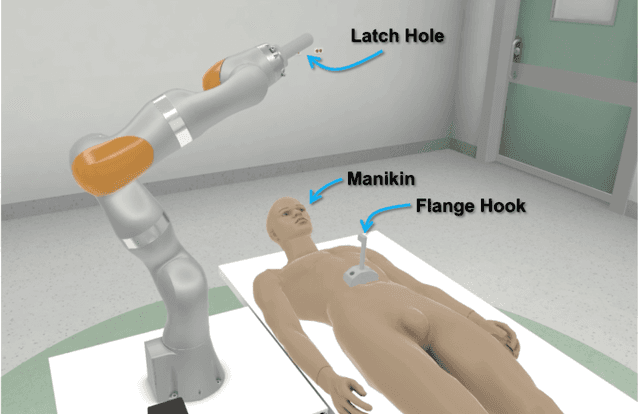
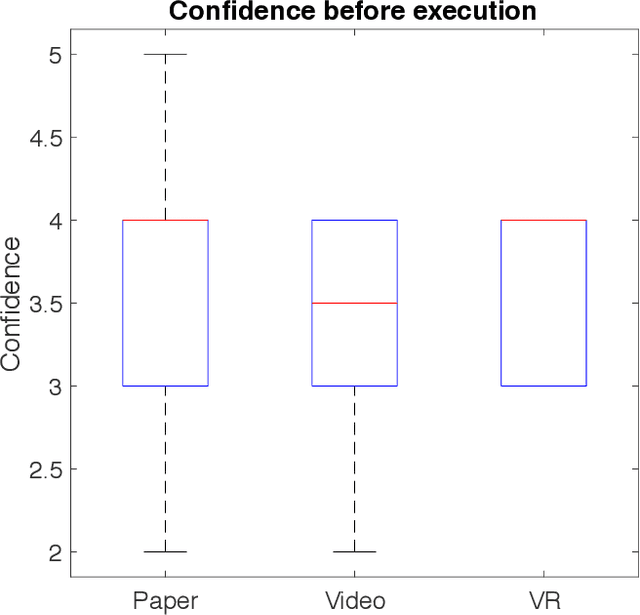
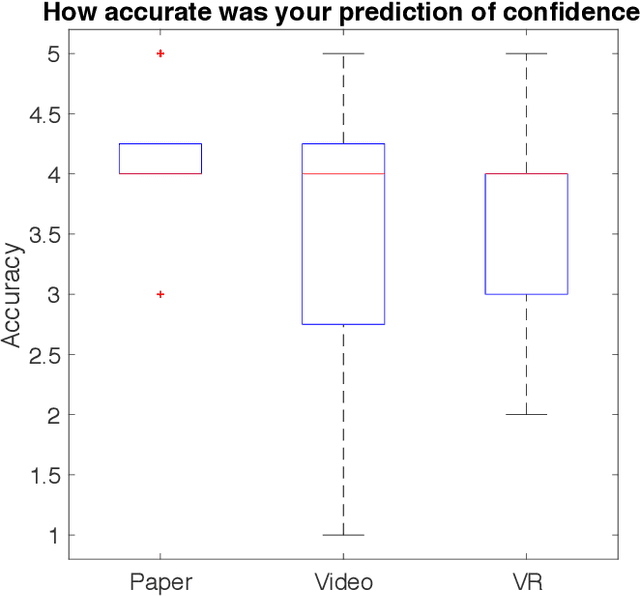
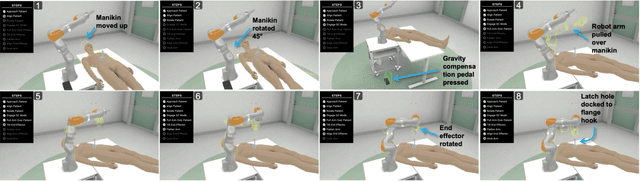
Abstract:Virtual Reality (VR) is rapidly increasing in popularity as a teaching tool. It allows for the creation of a highly immersive, three-dimensional virtual environment intended to simulate real-life environments. With more robots saturating the industry - from manufacturing to healthcare, there is a need to train end-users on how to set up, operate, tear down, and troubleshoot the robot. Even though VR has become widely used in training surgeons on the psychomotor skills associated with operating the robot, little research has been done to see how the benefits of VR could translate to teaching the bedside staff, tasked with supporting the robot during the full end-to-end surgical procedure. We trained 30 participants on how to set up a robotic arm in an environment mimicking clinical setup. We divided these participants equally into 3 groups with one group trained with paper-based instructions, one with video-based instructions and one with VR-based instructions. We then compared and contrasted these three different training methods. VR and paper-based were highly favored training mediums over video-based. VR-trained participants achieved slightly higher fidelity of individual robotic joint angles, suggesting better comprehension of the spatial awareness skills necessary to achieve desired arm positioning. In addition, VR resulted in higher reproducibility of setup fidelity and more consistency in user confidence levels as compared to paper and video-based training.
A Comparative Analysis of Virtual Reality Head-Mounted Display Systems
Dec 05, 2019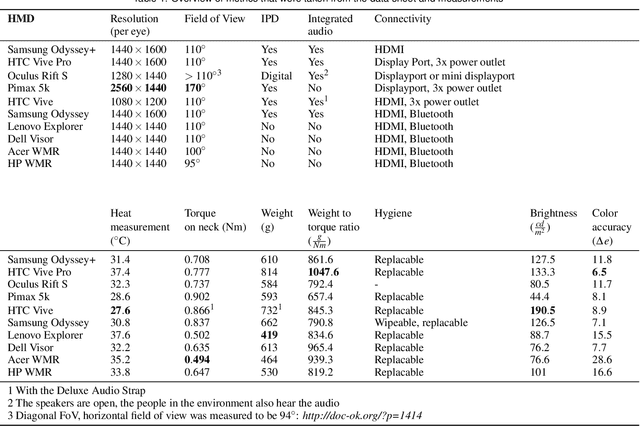
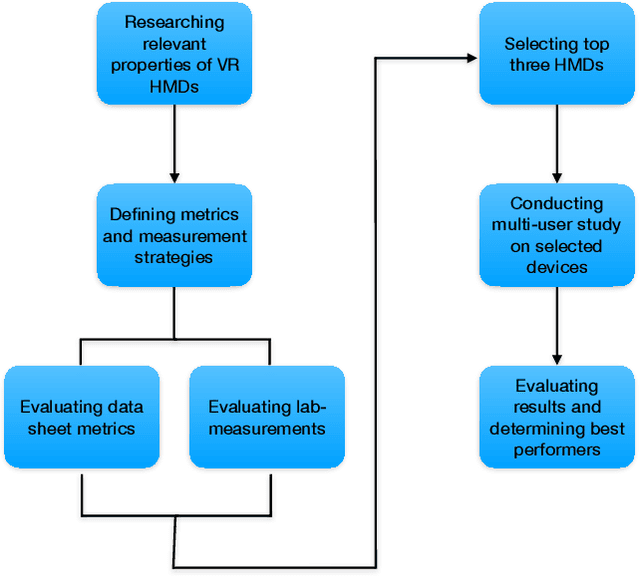
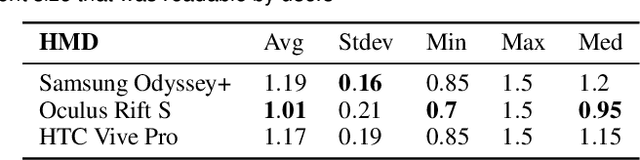
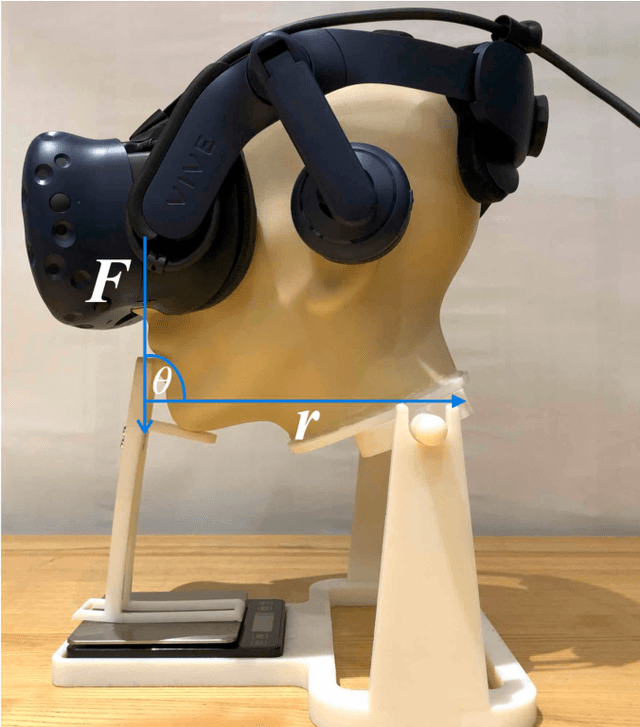
Abstract:With recent advances of Virtual Reality (VR) technology, the deployment of such will dramatically increase in non-entertainment environments, such as professional education and training, manufacturing, service, or low frequency/high risk scenarios. Clinical education is an area that especially stands to benefit from VR technology due to the complexity, high cost, and difficult logistics. The effectiveness of the deployment of VR systems, is subject to factors that may not be necessarily considered for devices targeting the entertainment market. In this work, we systematically compare a wide range of VR Head-Mounted Displays (HMDs) technologies and designs by defining a new set of metrics that are 1) relevant to most generic VR solutions and 2) are of paramount importance for VR-based education and training. We evaluated ten HMDs based on various criteria, including neck strain, heat development, and color accuracy. Other metrics such as text readability, comfort, and contrast perception were evaluated in a multi-user study on three selected HMDs, namely Oculus Rift S, HTC Vive Pro and Samsung Odyssey+. Results indicate that the HTC Vive Pro performs best with regards to comfort, display quality and compatibility with glasses.
Reflective-AR Display: An Interaction Methodology for Virtual-Real Alignment in Medical Robotics
Jul 23, 2019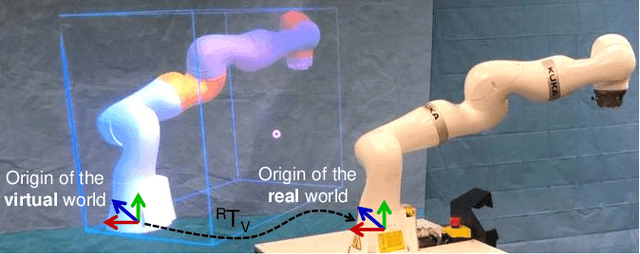
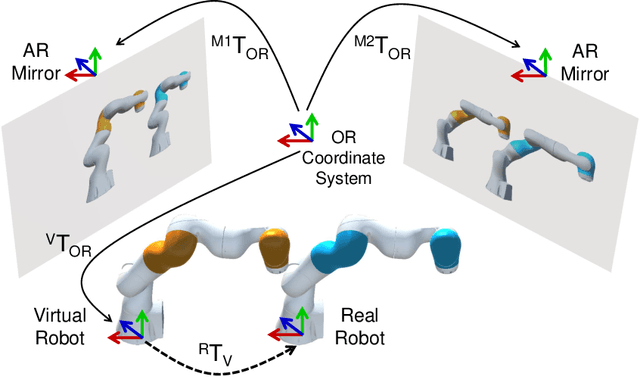
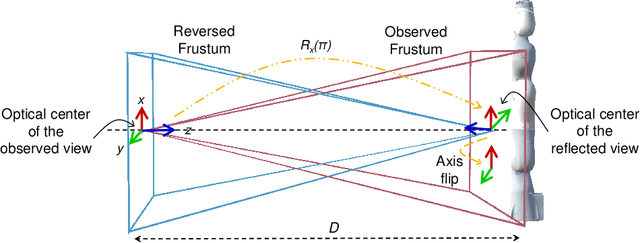
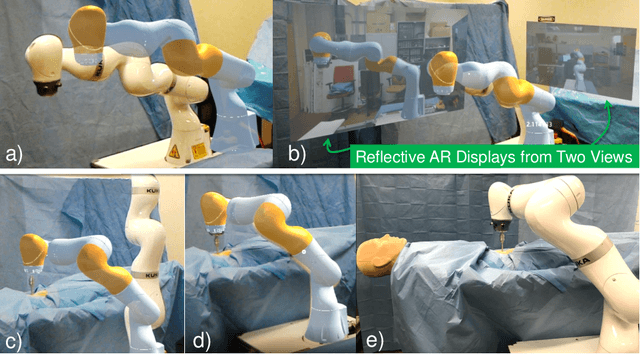
Abstract:Robot-assisted minimally invasive surgery has shown to improve patient outcomes, as well as reduce complications and recovery time for several clinical applications. However, increasingly configurable robotic arms require careful setup by surgical staff to maximize anatomical reach and avoid collisions. Furthermore, safety regulations prevent automatically driving robotic arms to this optimal positioning. We propose a Head-Mounted Display (HMD) based augmented reality (AR) guidance system for optimal surgical arm setup. In this case, the staff equipped with HMD aligns the robot with its planned virtual counterpart. The main challenge, however, is the perspective ambiguities hindering such collaborative robotic solution. To overcome this challenge, we introduce a novel registration concept for intuitive alignment of such AR content by providing a multi-view AR experience via reflective-AR displays that show the augmentations from multiple viewpoints. Using this system, operators can visualize different perspectives simultaneously while actively adjusting the pose to determine the registration transformation that most closely superimposes the virtual onto real. The experimental results demonstrate improvement in the interactive alignment of a virtual and real robot when using a reflective-AR display. We also present measurements from configuring a robotic manipulator in a simulated trocar placement surgery using the AR guidance methodology.
Plan in 2D, execute in 3D: An augmented reality solution for cup placement in total hip arthroplasty
Jan 04, 2018Abstract:Reproducibly achieving proper implant alignment is a critical step in total hip arthroplasty (THA) procedures that has been shown to substantially affect patient outcome. In current practice, correct alignment of the acetabular cup is verified in C-arm X-ray images that are acquired in an anterior-posterior (AP) view. Favorable surgical outcome is, therefore, heavily dependent on the surgeon's experience in understanding the 3D orientation of a hemispheric implant from 2D AP projection images. This work proposes an easy to use intra-operative component planning system based on two C-arm X-ray images that is combined with 3D augmented reality (AR) visualization that simplifies impactor and cup placement according to the planning by providing a real-time RGBD data overlay. We evaluate the feasibility of our system in a user study comprising four orthopedic surgeons at the Johns Hopkins Hospital, and also report errors in translation, anteversion, and abduction as low as 1.98 mm, 1.10 degrees, and 0.53 degrees, respectively. The promising performance of this AR solution shows that deploying this system could eliminate the need for excessive radiation, simplify the intervention, and enable reproducibly accurate placement of acetabular implants.
Towards MRI-Based Autonomous Robotic US Acquisitions: A First Feasibility Study
Jul 28, 2016



Abstract:Robotic ultrasound has the potential to assist and guide physicians during interventions. In this work, we present a set of methods and a workflow to enable autonomous MRI-guided ultrasound acquisitions. Our approach uses a structured-light 3D scanner for patient-to-robot and image-to-patient calibration, which in turn is used to plan 3D ultrasound trajectories. These MRI-based trajectories are followed autonomously by the robot and are further refined online using automatic MRI/US registration. Despite the low spatial resolution of structured light scanners, the initial planned acquisition path can be followed with an accuracy of 2.46 +/- 0.96 mm. This leads to a good initialization of the MRI/US registration: the 3D-scan-based alignment for planning and acquisition shows an accuracy (distance between planned ultrasound and MRI) of 4.47 mm, and 0.97 mm after an online-update of the calibration based on a closed loop registration.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge