Nicolas Lenhart
Enhancing Interpretability of Vertebrae Fracture Grading using Human-interpretable Prototypes
Apr 03, 2024
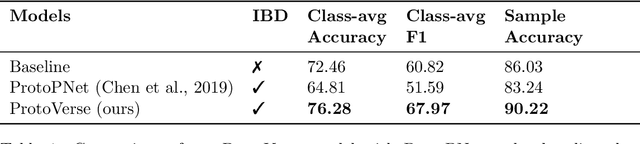
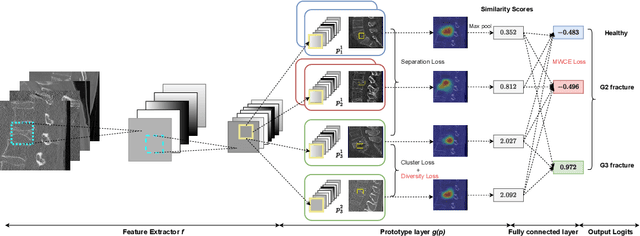
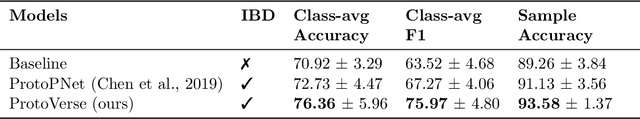
Abstract:Vertebral fracture grading classifies the severity of vertebral fractures, which is a challenging task in medical imaging and has recently attracted Deep Learning (DL) models. Only a few works attempted to make such models human-interpretable despite the need for transparency and trustworthiness in critical use cases like DL-assisted medical diagnosis. Moreover, such models either rely on post-hoc methods or additional annotations. In this work, we propose a novel interpretable-by-design method, ProtoVerse, to find relevant sub-parts of vertebral fractures (prototypes) that reliably explain the model's decision in a human-understandable way. Specifically, we introduce a novel diversity-promoting loss to mitigate prototype repetitions in small datasets with intricate semantics. We have experimented with the VerSe'19 dataset and outperformed the existing prototype-based method. Further, our model provides superior interpretability against the post-hoc method. Importantly, expert radiologists validated the visual interpretability of our results, showing clinical applicability.
Evaluation of GPT-4 for chest X-ray impression generation: A reader study on performance and perception
Nov 12, 2023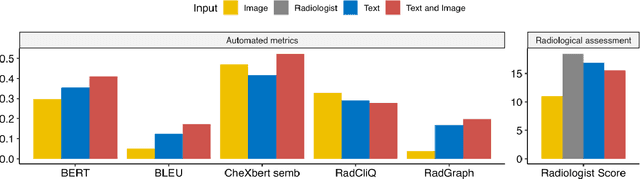
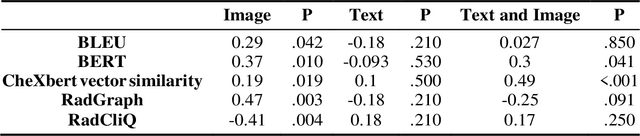
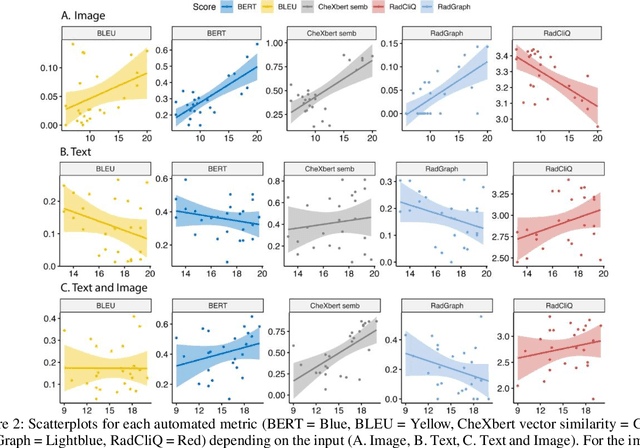
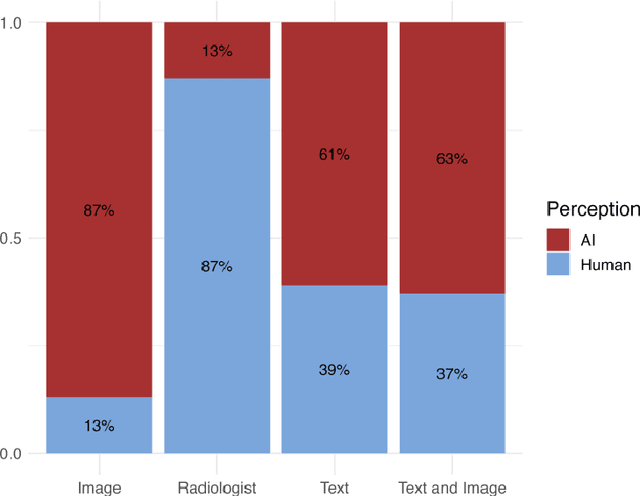
Abstract:The remarkable generative capabilities of multimodal foundation models are currently being explored for a variety of applications. Generating radiological impressions is a challenging task that could significantly reduce the workload of radiologists. In our study we explored and analyzed the generative abilities of GPT-4 for Chest X-ray impression generation. To generate and evaluate impressions of chest X-rays based on different input modalities (image, text, text and image), a blinded radiological report was written for 25-cases of the publicly available NIH-dataset. GPT-4 was given image, finding section or both sequentially to generate an input dependent impression. In a blind randomized reading, 4-radiologists rated the impressions and were asked to classify the impression origin (Human, AI), providing justification for their decision. Lastly text model evaluation metrics and their correlation with the radiological score (summation of the 4 dimensions) was assessed. According to the radiological score, the human-written impression was rated highest, although not significantly different to text-based impressions. The automated evaluation metrics showed moderate to substantial correlations to the radiological score for the image impressions, however individual scores were highly divergent among inputs, indicating insufficient representation of radiological quality. Detection of AI-generated impressions varied by input and was 61% for text-based impressions. Impressions classified as AI-generated had significantly worse radiological scores even when written by a radiologist, indicating potential bias. Our study revealed significant discrepancies between a radiological assessment and common automatic evaluation metrics depending on the model input. The detection of AI-generated findings is subject to bias that highly rated impressions are perceived as human-written.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge