Tom Pollard
EHRCon: Dataset for Checking Consistency between Unstructured Notes and Structured Tables in Electronic Health Records
Jun 24, 2024



Abstract:Electronic Health Records (EHRs) are integral for storing comprehensive patient medical records, combining structured data (e.g., medications) with detailed clinical notes (e.g., physician notes). These elements are essential for straightforward data retrieval and provide deep, contextual insights into patient care. However, they often suffer from discrepancies due to unintuitive EHR system designs and human errors, posing serious risks to patient safety. To address this, we developed EHRCon, a new dataset and task specifically designed to ensure data consistency between structured tables and unstructured notes in EHRs. EHRCon was crafted in collaboration with healthcare professionals using the MIMIC-III EHR dataset, and includes manual annotations of 3,943 entities across 105 clinical notes checked against database entries for consistency. EHRCon has two versions, one using the original MIMIC-III schema, and another using the OMOP CDM schema, in order to increase its applicability and generalizability. Furthermore, leveraging the capabilities of large language models, we introduce CheckEHR, a novel framework for verifying the consistency between clinical notes and database tables. CheckEHR utilizes an eight-stage process and shows promising results in both few-shot and zero-shot settings. The code is available at https://github.com/dustn1259/EHRCon.
Evaluating the Impact of Social Determinants on Health Prediction
May 22, 2023
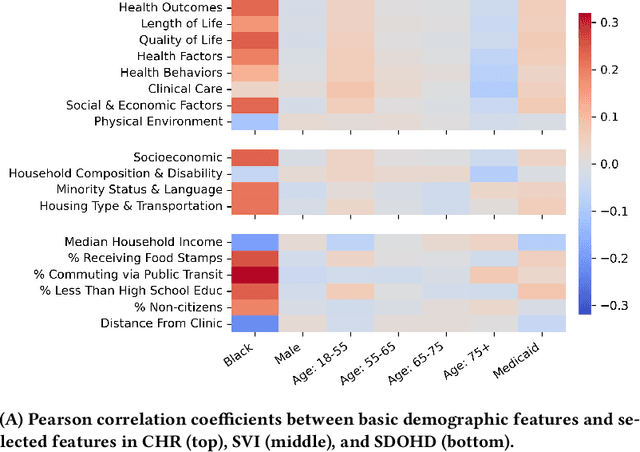


Abstract:Social determinants of health (SDOH) -- the conditions in which people live, grow, and age -- play a crucial role in a person's health and well-being. There is a large, compelling body of evidence in population health studies showing that a wide range of SDOH is strongly correlated with health outcomes. Yet, a majority of the risk prediction models based on electronic health records (EHR) do not incorporate a comprehensive set of SDOH features as they are often noisy or simply unavailable. Our work links a publicly available EHR database, MIMIC-IV, to well-documented SDOH features. We investigate the impact of such features on common EHR prediction tasks across different patient populations. We find that community-level SDOH features do not improve model performance for a general patient population, but can improve data-limited model fairness for specific subpopulations. We also demonstrate that SDOH features are vital for conducting thorough audits of algorithmic biases beyond protective attributes. We hope the new integrated EHR-SDOH database will enable studies on the relationship between community health and individual outcomes and provide new benchmarks to study algorithmic biases beyond race, gender, and age.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge