Gloria Hyunjung Kwak
Longitudinal Progression Prediction of Alzheimer's Disease with Tabular Foundation Model
Aug 25, 2025Abstract:Alzheimer's disease is a progressive neurodegenerative disorder that remains challenging to predict due to its multifactorial etiology and the complexity of multimodal clinical data. Accurate forecasting of clinically relevant biomarkers, including diagnostic and quantitative measures, is essential for effective monitoring of disease progression. This work introduces L2C-TabPFN, a method that integrates a longitudinal-to-cross-sectional (L2C) transformation with a pre-trained Tabular Foundation Model (TabPFN) to predict Alzheimer's disease outcomes using the TADPOLE dataset. L2C-TabPFN converts sequential patient records into fixed-length feature vectors, enabling robust prediction of diagnosis, cognitive scores, and ventricular volume. Experimental results demonstrate that, while L2C-TabPFN achieves competitive performance on diagnostic and cognitive outcomes, it provides state-of-the-art results in ventricular volume prediction. This key imaging biomarker reflects neurodegeneration and progression in Alzheimer's disease. These findings highlight the potential of tabular foundational models for advancing longitudinal prediction of clinically relevant imaging markers in Alzheimer's disease.
Learning ECG Representations via Poly-Window Contrastive Learning
Aug 21, 2025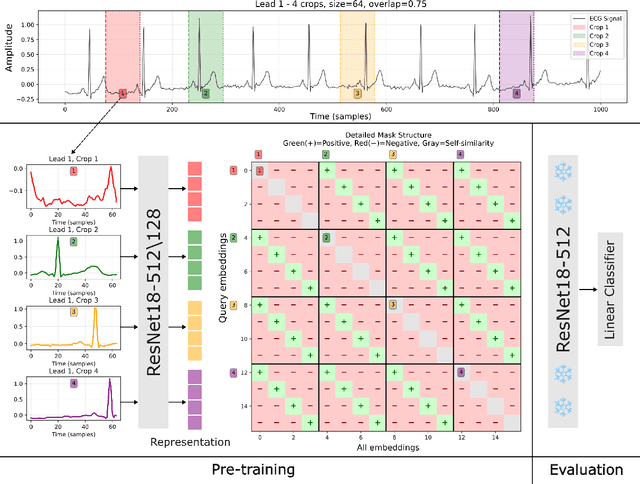
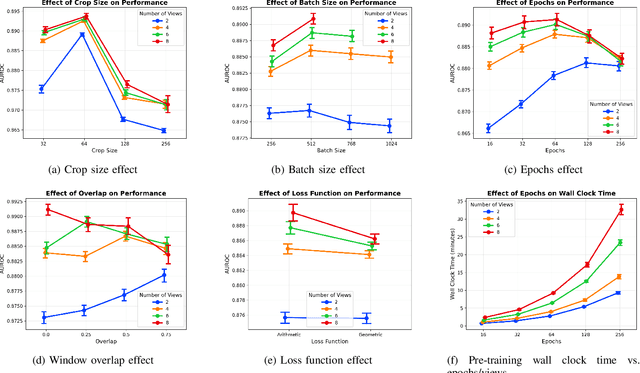
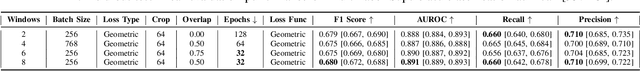

Abstract:Electrocardiogram (ECG) analysis is foundational for cardiovascular disease diagnosis, yet the performance of deep learning models is often constrained by limited access to annotated data. Self-supervised contrastive learning has emerged as a powerful approach for learning robust ECG representations from unlabeled signals. However, most existing methods generate only pairwise augmented views and fail to leverage the rich temporal structure of ECG recordings. In this work, we present a poly-window contrastive learning framework. We extract multiple temporal windows from each ECG instance to construct positive pairs and maximize their agreement via statistics. Inspired by the principle of slow feature analysis, our approach explicitly encourages the model to learn temporally invariant and physiologically meaningful features that persist across time. We validate our approach through extensive experiments and ablation studies on the PTB-XL dataset. Our results demonstrate that poly-window contrastive learning consistently outperforms conventional two-view methods in multi-label superclass classification, achieving higher AUROC (0.891 vs. 0.888) and F1 scores (0.680 vs. 0.679) while requiring up to four times fewer pre-training epochs (32 vs. 128) and 14.8% in total wall clock pre-training time reduction. Despite processing multiple windows per sample, we achieve a significant reduction in the number of training epochs and total computation time, making our method practical for training foundational models. Through extensive ablations, we identify optimal design choices and demonstrate robustness across various hyperparameters. These findings establish poly-window contrastive learning as a highly efficient and scalable paradigm for automated ECG analysis and provide a promising general framework for self-supervised representation learning in biomedical time-series data.
Evaluating the Impact of Social Determinants on Health Prediction
May 22, 2023
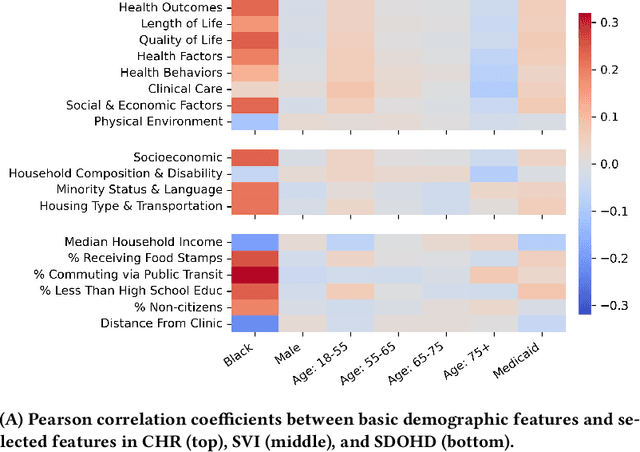


Abstract:Social determinants of health (SDOH) -- the conditions in which people live, grow, and age -- play a crucial role in a person's health and well-being. There is a large, compelling body of evidence in population health studies showing that a wide range of SDOH is strongly correlated with health outcomes. Yet, a majority of the risk prediction models based on electronic health records (EHR) do not incorporate a comprehensive set of SDOH features as they are often noisy or simply unavailable. Our work links a publicly available EHR database, MIMIC-IV, to well-documented SDOH features. We investigate the impact of such features on common EHR prediction tasks across different patient populations. We find that community-level SDOH features do not improve model performance for a general patient population, but can improve data-limited model fairness for specific subpopulations. We also demonstrate that SDOH features are vital for conducting thorough audits of algorithmic biases beyond protective attributes. We hope the new integrated EHR-SDOH database will enable studies on the relationship between community health and individual outcomes and provide new benchmarks to study algorithmic biases beyond race, gender, and age.
Predicting Hyperkalemia in the ICU and Evaluation of Generalizability and Interpretability
Jan 27, 2021



Abstract:Hyperkalemia is a potentially life-threatening condition that can lead to fatal arrhythmias. Early identification of high risk patients can inform clinical care to mitigate the risk. While hyperkalemia is often a complication of acute kidney injury (AKI), it also occurs in the absence of AKI. We developed predictive models to identify intensive care unit (ICU) patients at risk of developing hyperkalemia by using the Medical Information Mart for Intensive Care (MIMIC) and the eICU Collaborative Research Database (eICU-CRD). Our methodology focused on building multiple models, optimizing for interpretability through model selection, and simulating various clinical scenarios. In order to determine if our models perform accurately on patients with and without AKI, we evaluated the following clinical cases: (i) predicting hyperkalemia after AKI within 14 days of ICU admission, (ii) predicting hyperkalemia within 14 days of ICU admission regardless of AKI status, and compared different lead times for (i) and (ii). Both clinical scenarios were modeled using logistic regression (LR), random forest (RF), and XGBoost. Using observations from the first day in the ICU, our models were able to predict hyperkalemia with an AUC of (i) 0.79, 0.81, 0.81 and (ii) 0.81, 0.85, 0.85 for LR, RF, and XGBoost respectively. We found that 4 out of the top 5 features were consistent across the models. AKI stage was significant in the models that included all patients with or without AKI, but not in the models which only included patients with AKI. This suggests that while AKI is important for hyperkalemia, the specific stage of AKI may not be as important. Our findings require further investigation and confirmation.
* 6 pages, 3 figures, 3 tables
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge