Peter H. Charlton
Obstructive Sleep Apnea Characterization: A Multimodal Cross-Recurrence-Based Approach for Investigating Atrial Fibrillation
Apr 30, 2025Abstract:Obstructive sleep apnea (OSA) is believed to contribute significantly to atrial fibrillation (AF) development in certain patients. Recent studies indicate a rising risk of AF with increasing OSA severity. However, the commonly used apnea-hypopnea index in clinical practice may not adequately account for the potential cardiovascular risks associated with OSA. (1) Objective: to propose and explore a novel method for assessing OSA severity considering potential connection to cardiac arrhythmias. (2) Method: the approach utilizes cross-recurrence features to characterize OSA and AF by considering the relationships among oxygen desaturation, pulse arrival time, and heart-beat intervals. Multinomial logistic regression models were trained to predict four levels of OSA severity and four groups related to heart rhythm issues. The rank biserial correlation coefficient, rrb, was used to estimate effect size for statistical analysis. The investigation was conducted using the MESA database, which includes polysomnography data from 2055 subjects. (3) Results: a derived cross-recurrence-based index showed a significant association with a higher OSA severity (p < 0.01) and the presence of AF (p < 0.01). Additionally, the proposed index had a significantly larger effect, rrb, than the conventional apnea-hypopnea index in differentiating increasingly severe heart rhythm issue groups: 0.14 > 0.06, 0.33 > 0.10, and 0.41 > 0.07. (4) Significance: the proposed method holds relevance as a supplementary diagnostic tool for assessing the authentic state of sleep apnea in clinical practice.
Towards deployment-centric multimodal AI beyond vision and language
Apr 04, 2025Abstract:Multimodal artificial intelligence (AI) integrates diverse types of data via machine learning to improve understanding, prediction, and decision-making across disciplines such as healthcare, science, and engineering. However, most multimodal AI advances focus on models for vision and language data, while their deployability remains a key challenge. We advocate a deployment-centric workflow that incorporates deployment constraints early to reduce the likelihood of undeployable solutions, complementing data-centric and model-centric approaches. We also emphasise deeper integration across multiple levels of multimodality and multidisciplinary collaboration to significantly broaden the research scope beyond vision and language. To facilitate this approach, we identify common multimodal-AI-specific challenges shared across disciplines and examine three real-world use cases: pandemic response, self-driving car design, and climate change adaptation, drawing expertise from healthcare, social science, engineering, science, sustainability, and finance. By fostering multidisciplinary dialogue and open research practices, our community can accelerate deployment-centric development for broad societal impact.
Machine-learning for photoplethysmography analysis: Benchmarking feature, image, and signal-based approaches
Feb 27, 2025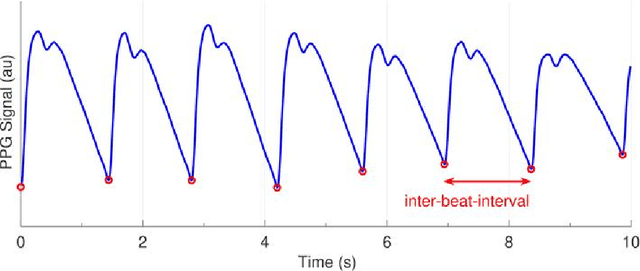
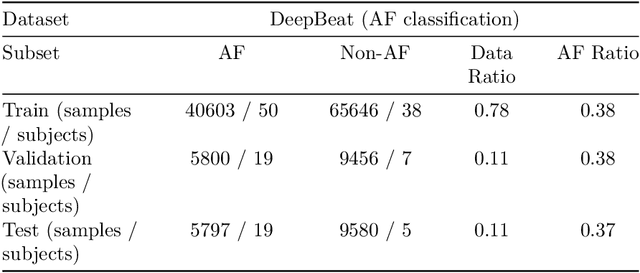
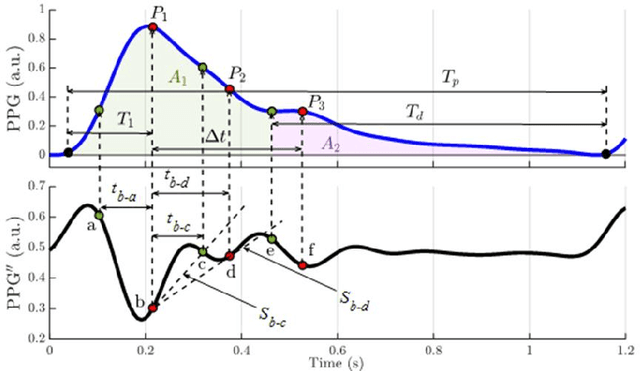
Abstract:Photoplethysmography (PPG) is a widely used non-invasive physiological sensing technique, suitable for various clinical applications. Such clinical applications are increasingly supported by machine learning methods, raising the question of the most appropriate input representation and model choice. Comprehensive comparisons, in particular across different input representations, are scarce. We address this gap in the research landscape by a comprehensive benchmarking study covering three kinds of input representations, interpretable features, image representations and raw waveforms, across prototypical regression and classification use cases: blood pressure and atrial fibrillation prediction. In both cases, the best results are achieved by deep neural networks operating on raw time series as input representations. Within this model class, best results are achieved by modern convolutional neural networks (CNNs). but depending on the task setup, shallow CNNs are often also very competitive. We envision that these results will be insightful for researchers to guide their choice on machine learning tasks for PPG data, even beyond the use cases presented in this work.
Generalizable deep learning for photoplethysmography-based blood pressure estimation -- A Benchmarking Study
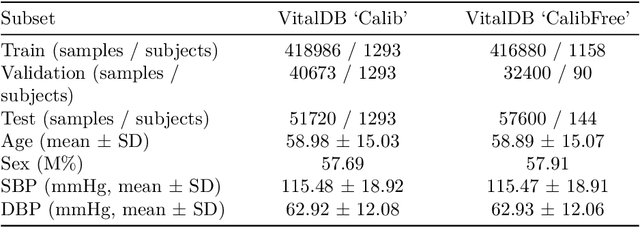
Feb 26, 2025Abstract:Photoplethysmography (PPG)-based blood pressure (BP) estimation represents a promising alternative to cuff-based BP measurements. Recently, an increasing number of deep learning models have been proposed to infer BP from the raw PPG waveform. However, these models have been predominantly evaluated on in-distribution test sets, which immediately raises the question of the generalizability of these models to external datasets. To investigate this question, we trained five deep learning models on the recently released PulseDB dataset, provided in-distribution benchmarking results on this dataset, and then assessed out-of-distribution performance on several external datasets. The best model (XResNet1d101) achieved in-distribution MAEs of 9.4 and 6.0 mmHg for systolic and diastolic BP respectively on PulseDB (with subject-specific calibration), and 14.0 and 8.5 mmHg respectively without calibration. Equivalent MAEs on external test datasets without calibration ranged from 15.0 to 25.1 mmHg (SBP) and 7.0 to 10.4 mmHg (DBP). Our results indicate that the performance is strongly influenced by the differences in BP distributions between datasets. We investigated a simple way of improving performance through sample-based domain adaptation and put forward recommendations for training models with good generalization properties. With this work, we hope to educate more researchers for the importance and challenges of out-of-distribution generalization.
SleepPPG-Net: a deep learning algorithm for robust sleep staging from continuous photoplethysmography
Feb 18, 2022



Abstract:Introduction: Sleep staging is an essential component in the diagnosis of sleep disorders and management of sleep health. It is traditionally measured in a clinical setting and requires a labor-intensive labeling process. We hypothesize that it is possible to perform robust 4-class sleep staging using the raw photoplethysmography (PPG) time series and modern advances in deep learning (DL). Methods: We used two publicly available sleep databases that included raw PPG recordings, totalling 2,374 patients and 23,055 hours. We developed SleepPPG-Net, a DL model for 4-class sleep staging from the raw PPG time series. SleepPPG-Net was trained end-to-end and consists of a residual convolutional network for automatic feature extraction and a temporal convolutional network to capture long-range contextual information. We benchmarked the performance of SleepPPG-Net against models based on the best-reported state-of-the-art (SOTA) algorithms. Results: When benchmarked on a held-out test set, SleepPPG-Net obtained a median Cohen's Kappa ($\kappa$) score of 0.75 against 0.69 for the best SOTA approach. SleepPPG-Net showed good generalization performance to an external database, obtaining a $\kappa$ score of 0.74 after transfer learning. Perspective: Overall, SleepPPG-Net provides new SOTA performance. In addition, performance is high enough to open the path to the development of wearables that meet the requirements for usage in clinical applications such as the diagnosis and monitoring of obstructive sleep apnea.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge