Paul Varghese
A tutorial on fairness in machine learning in healthcare
Jun 15, 2024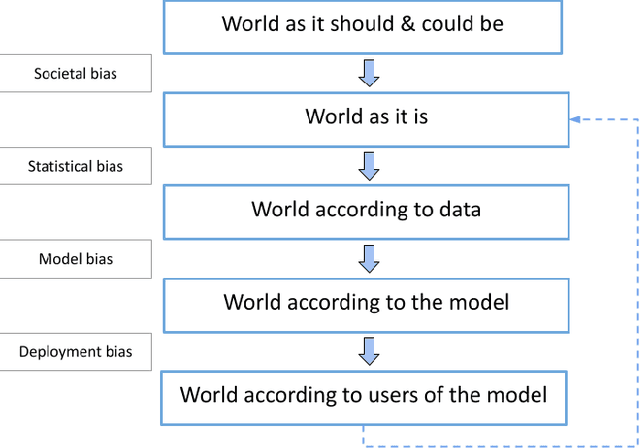
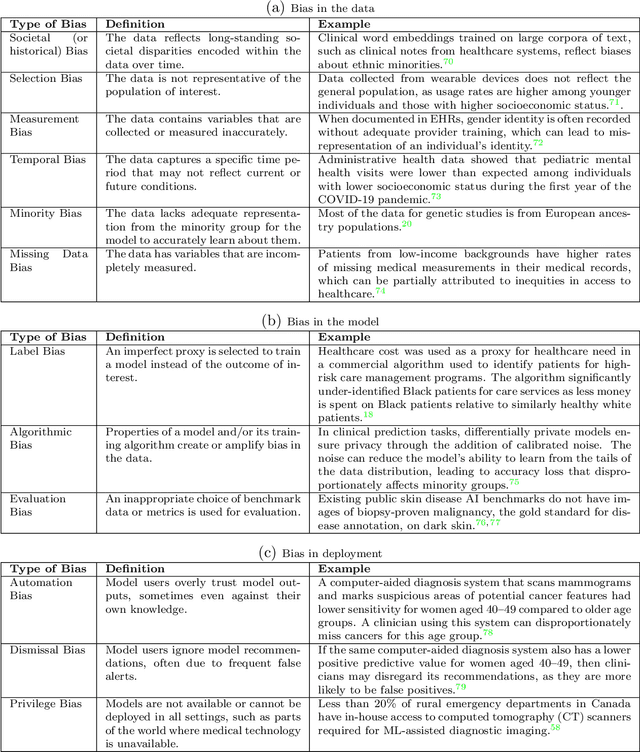
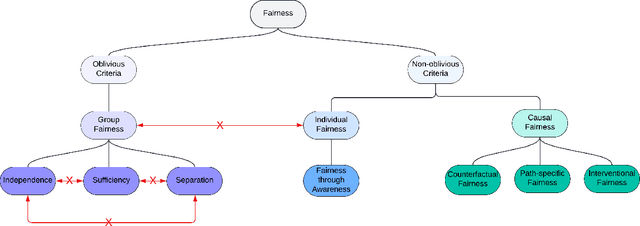
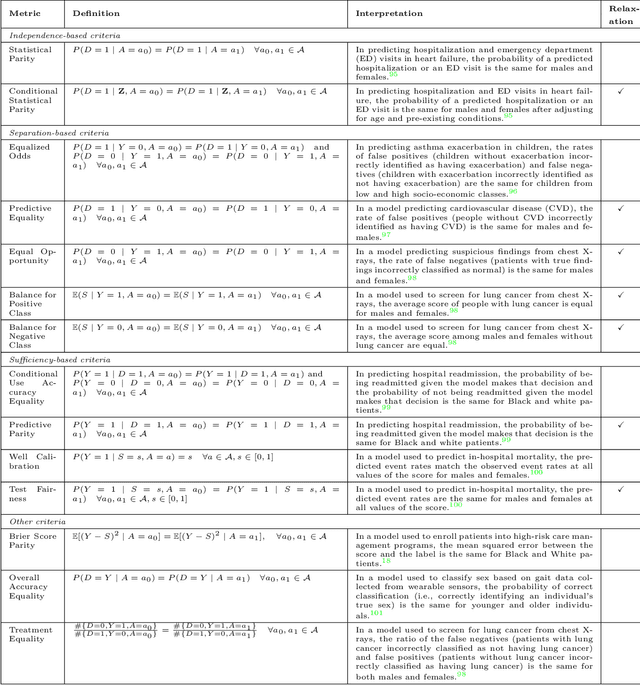
Abstract:$\textbf{OBJECTIVE}$: Ensuring that machine learning (ML) algorithms are safe and effective within all patient groups, and do not disadvantage particular patients, is essential to clinical decision making and preventing the reinforcement of existing healthcare inequities. The objective of this tutorial is to introduce the medical informatics community to the common notions of fairness within ML, focusing on clinical applications and implementation in practice. $\textbf{TARGET AUDIENCE}$: As gaps in fairness arise in a variety of healthcare applications, this tutorial is designed to provide an understanding of fairness, without assuming prior knowledge, to researchers and clinicians who make use of modern clinical data. $\textbf{SCOPE}$: We describe the fundamental concepts and methods used to define fairness in ML, including an overview of why models in healthcare may be unfair, a summary and comparison of the metrics used to quantify fairness, and a discussion of some ongoing research. We illustrate some of the fairness methods introduced through a case study of mortality prediction in a publicly available electronic health record dataset. Finally, we provide a user-friendly R package for comprehensive group fairness evaluation, enabling researchers and clinicians to assess fairness in their own ML work.
Uncertainty-Aware PPG-2-ECG for Enhanced Cardiovascular Diagnosis using Diffusion Models
May 19, 2024Abstract:Analyzing the cardiovascular system condition via Electrocardiography (ECG) is a common and highly effective approach, and it has been practiced and perfected over many decades. ECG sensing is non-invasive and relatively easy to acquire, and yet it is still cumbersome for holter monitoring tests that may span over hours and even days. A possible alternative in this context is Photoplethysmography (PPG): An optically-based signal that measures blood volume fluctuations, as typically sensed by conventional ``wearable devices''. While PPG presents clear advantages in acquisition, convenience, and cost-effectiveness, ECG provides more comprehensive information, allowing for a more precise detection of heart conditions. This implies that a conversion from PPG to ECG, as recently discussed in the literature, inherently involves an unavoidable level of uncertainty. In this paper we introduce a novel methodology for addressing the PPG-2-ECG conversion, and offer an enhanced classification of cardiovascular conditions using the given PPG, all while taking into account the uncertainties arising from the conversion process. We provide a mathematical justification for our proposed computational approach, and present empirical studies demonstrating its superior performance compared to state-of-the-art baseline methods.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge