Toan D Nguyen
Revamping AI Models in Dermatology: Overcoming Critical Challenges for Enhanced Skin Lesion Diagnosis
Nov 02, 2023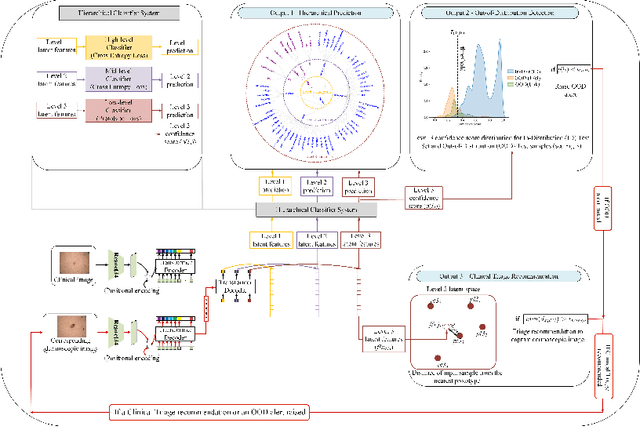
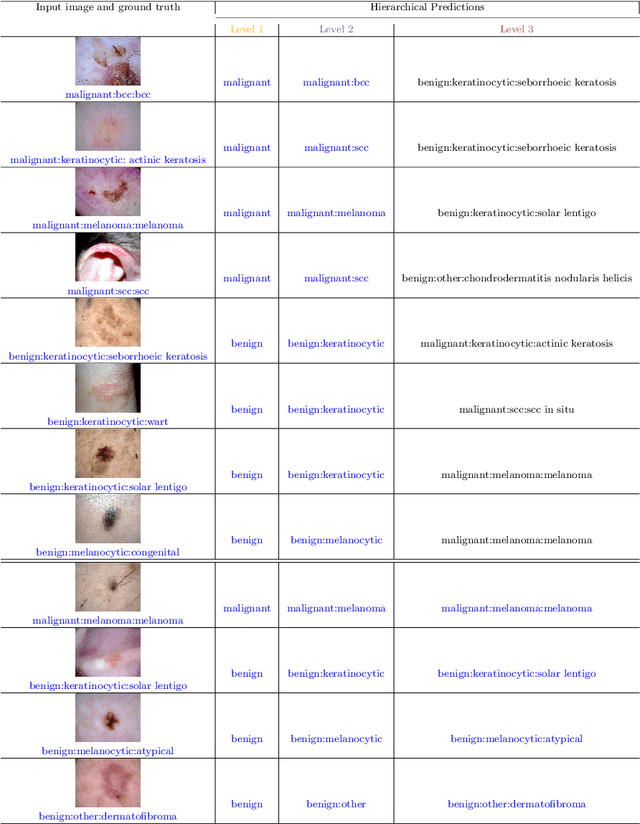
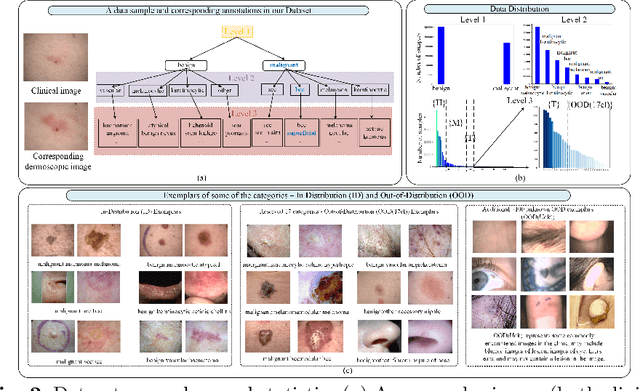
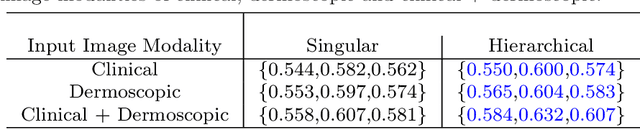
Abstract:The surge in developing deep learning models for diagnosing skin lesions through image analysis is notable, yet their clinical black faces challenges. Current dermatology AI models have limitations: limited number of possible diagnostic outputs, lack of real-world testing on uncommon skin lesions, inability to detect out-of-distribution images, and over-reliance on dermoscopic images. To address these, we present an All-In-One \textbf{H}ierarchical-\textbf{O}ut of Distribution-\textbf{C}linical Triage (HOT) model. For a clinical image, our model generates three outputs: a hierarchical prediction, an alert for out-of-distribution images, and a recommendation for dermoscopy if clinical image alone is insufficient for diagnosis. When the recommendation is pursued, it integrates both clinical and dermoscopic images to deliver final diagnosis. Extensive experiments on a representative cutaneous lesion dataset demonstrate the effectiveness and synergy of each component within our framework. Our versatile model provides valuable decision support for lesion diagnosis and sets a promising precedent for medical AI applications.
Early Melanoma Diagnosis with Sequential Dermoscopic Images
Oct 12, 2021
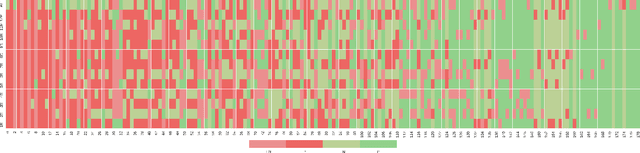
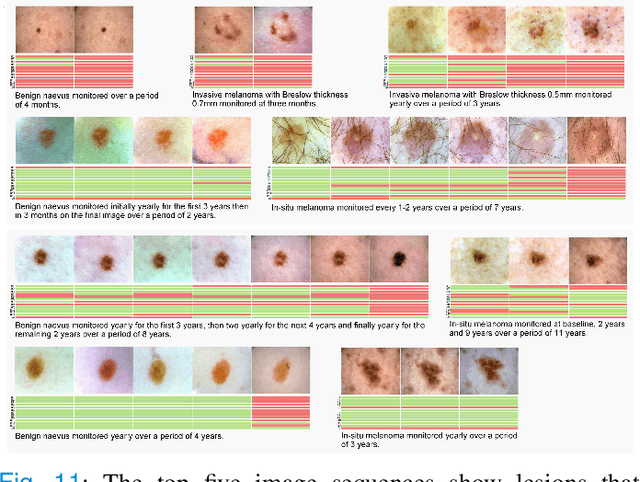
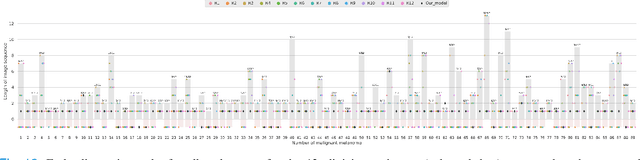
Abstract:Dermatologists often diagnose or rule out early melanoma by evaluating the follow-up dermoscopic images of skin lesions. However, existing algorithms for early melanoma diagnosis are developed using single time-point images of lesions. Ignoring the temporal, morphological changes of lesions can lead to misdiagnosis in borderline cases. In this study, we propose a framework for automated early melanoma diagnosis using sequential dermoscopic images. To this end, we construct our method in three steps. First, we align sequential dermoscopic images of skin lesions using estimated Euclidean transformations, extract the lesion growth region by computing image differences among the consecutive images, and then propose a spatio-temporal network to capture the dermoscopic changes from aligned lesion images and the corresponding difference images. Finally, we develop an early diagnosis module to compute probability scores of malignancy for lesion images over time. We collected 179 serial dermoscopic imaging data from 122 patients to verify our method. Extensive experiments show that the proposed model outperforms other commonly used sequence models. We also compared the diagnostic results of our model with those of seven experienced dermatologists and five registrars. Our model achieved higher diagnostic accuracy than clinicians (63.69% vs. 54.33%, respectively) and provided an earlier diagnosis of melanoma (60.7% vs. 32.7% of melanoma correctly diagnosed on the first follow-up images). These results demonstrate that our model can be used to identify melanocytic lesions that are at high-risk of malignant transformation earlier in the disease process and thereby redefine what is possible in the early detection of melanoma.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge