Tanner J. Zachem
Department of Neurosurgery, Duke University School of Medicine, Durham, NC, USA, Department of Mechanical Engineering and Materials Science, Duke University, Durham, NC, USA
Tendon-Actuated Concentric Tube Endonasal Robot (TACTER)
Apr 28, 2025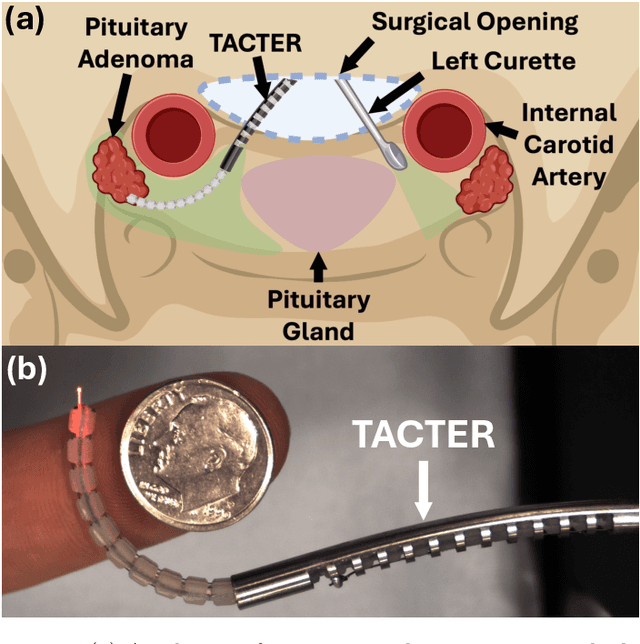
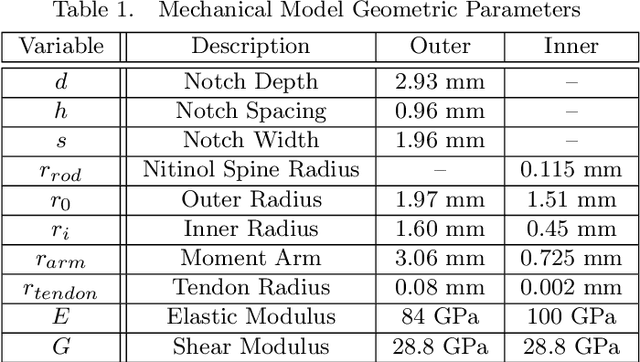
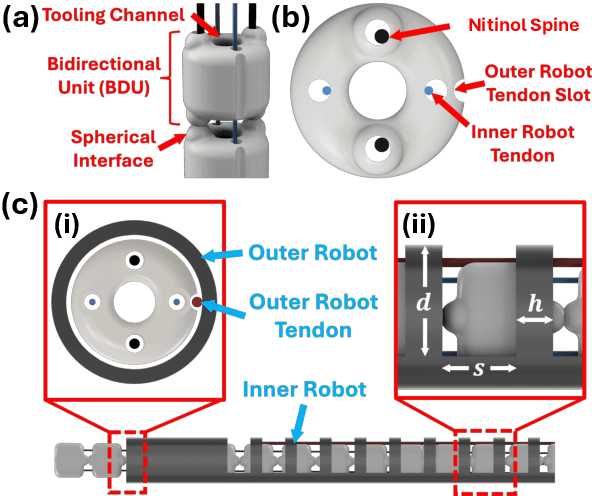
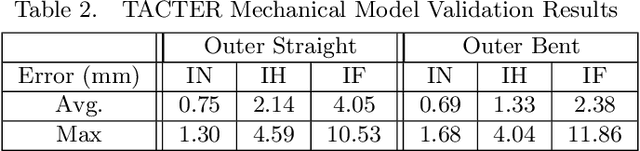
Abstract:Endoscopic endonasal approaches (EEA) have become more prevalent for minimally invasive skull base and sinus surgeries. However, rigid scopes and tools significantly decrease the surgeon's ability to operate in tight anatomical spaces and avoid critical structures such as the internal carotid artery and cranial nerves. This paper proposes a novel tendon-actuated concentric tube endonasal robot (TACTER) design in which two tendon-actuated robots are concentric to each other, resulting in an outer and inner robot that can bend independently. The outer robot is a unidirectionally asymmetric notch (UAN) nickel-titanium robot, and the inner robot is a 3D-printed bidirectional robot, with a nickel-titanium bending member. In addition, the inner robot can translate axially within the outer robot, allowing the tool to traverse through structures while bending, thereby executing follow-the-leader motion. A Cosserat-rod based mechanical model is proposed that uses tendon tension of both tendon-actuated robots and the relative translation between the robots as inputs and predicts the TACTER tip position for varying input parameters. The model is validated with experiments, and a human cadaver experiment is presented to demonstrate maneuverability from the nostril to the sphenoid sinus. This work presents the first tendon-actuated concentric tube (TACT) dexterous robotic tool capable of performing follow-the-leader motion within natural nasal orifices to cover workspaces typically required for a successful EEA.
Towards the Development of a Tendon-Actuated Galvanometer for Endoscopic Surgical Laser Scanning
Jun 05, 2024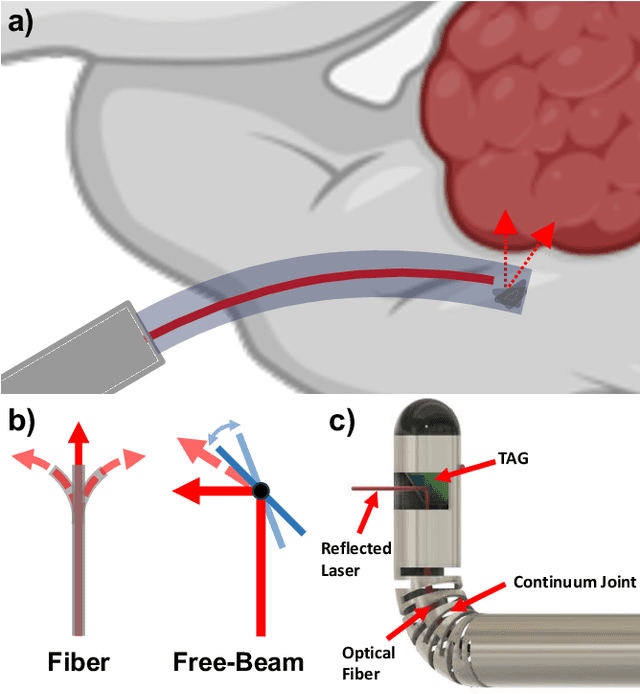
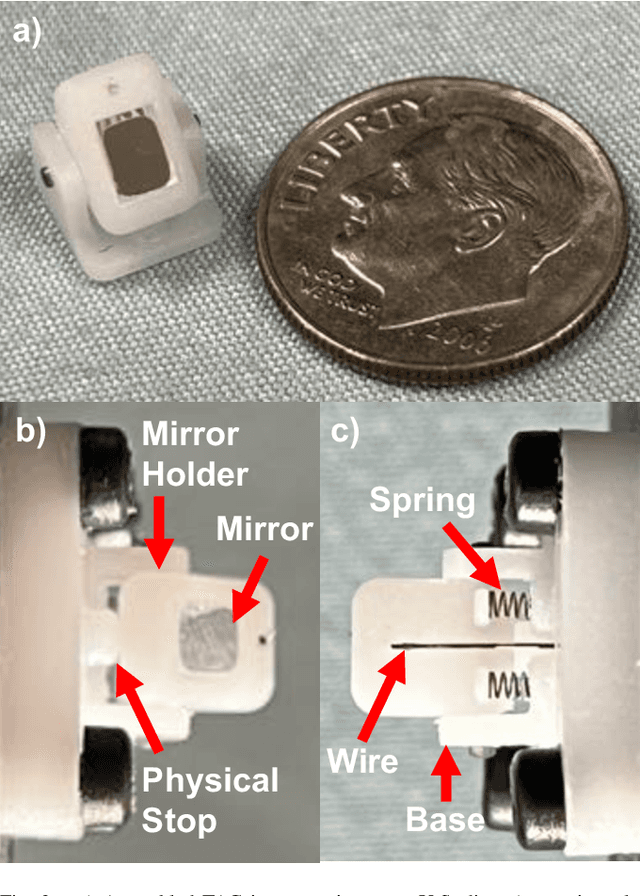
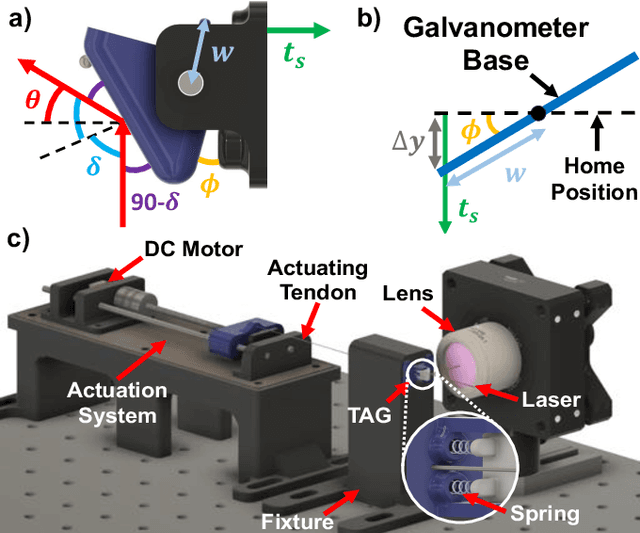
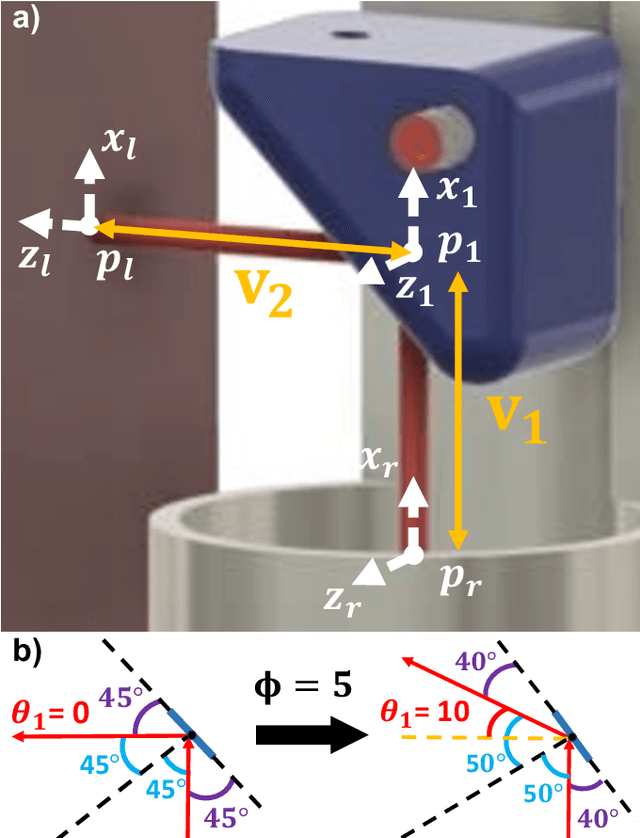
Abstract:There is a need for precision pathological sensing, imaging, and tissue manipulation in neurosurgical procedures, such as brain tumor resection. Precise tumor margin identification and resection can prevent further growth and protect critical structures. Surgical lasers with small laser diameters and steering capabilities can allow for new minimally invasive procedures by traversing through complex anatomy, then providing energy to sense, visualize, and affect tissue. In this paper, we present the design of a small-scale tendon-actuated galvanometer (TAG) that can serve as an end-effector tool for a steerable surgical laser. The galvanometer sensor design, fabrication, and kinematic modeling are presented and derived. It can accurately rotate up to 30.14 degrees (or a laser reflection angle of 60.28 degrees). A kinematic mapping of input tendon stroke to output galvanometer angle change and a forward-kinematics model relating the end of the continuum joint to the laser end-point are derived and validated.
Computer Vision for Increased Operative Efficiency via Identification of Instruments in the Neurosurgical Operating Room: A Proof-of-Concept Study
Dec 03, 2023


Abstract:Objectives Computer vision (CV) is a field of artificial intelligence that enables machines to interpret and understand images and videos. CV has the potential to be of assistance in the operating room (OR) to track surgical instruments. We built a CV algorithm for identifying surgical instruments in the neurosurgical operating room as a potential solution for surgical instrument tracking and management to decrease surgical waste and opening of unnecessary tools. Methods We collected 1660 images of 27 commonly used neurosurgical instruments. Images were labeled using the VGG Image Annotator and split into 80% training and 20% testing sets in order to train a U-Net Convolutional Neural Network using 5-fold cross validation. Results Our U-Net achieved a tool identification accuracy of 80-100% when distinguishing 25 classes of instruments, with 19/25 classes having accuracy over 90%. The model performance was not adequate for sub classifying Adson, Gerald, and Debakey forceps, which had accuracies of 60-80%. Conclusions We demonstrated the viability of using machine learning to accurately identify surgical instruments. Instrument identification could help optimize surgical tray packing, decrease tool usage and waste, decrease incidence of instrument misplacement events, and assist in timing of routine instrument maintenance. More training data will be needed to increase accuracy across all surgical instruments that would appear in a neurosurgical operating room. Such technology has the potential to be used as a method to be used for proving what tools are truly needed in each type of operation allowing surgeons across the world to do more with less.
Incident Angle Study for Designing an Endoscopic Tool for Intraoperative Brain Tumor Detection
Nov 07, 2023


Abstract:In neurosurgical procedures maximizing the resection of tumor tissue while avoiding healthy tissue is of paramount importance and a difficult task due to many factors, such as surrounding eloquent brain. Swiftly identifying tumor tissue for removal could increase surgical outcomes. The TumorID is a laser-induced fluorescence spectroscopy device that utilizes endogenous fluorophores such as NADH and FAD to detect tumor regions. With the goal of creating an endoscopic tool for intraoperative tumor detection in mind, a study of the TumorID was conducted to assess how the angle of incidence (AoI) affects the collected spectral response of the scanned tumor. For this study, flat and convex NADH/FAD gellan gum phantoms were scanned at various AoI (a range of 36 degrees) to observe the spectral behavior. Results showed that spectral signature did not change significantly across flat and convex phantoms, and the Area under Curve (AUC) values calculated for each spectrum had a standard deviation of 0.02 and 0.01 for flat and convex phantoms, respectively. Therefore, the study showed that AoI will affect the intensity of the spectral response, but the peaks representative of the endogenous fluorophores are still observable and similar. Future work includes conducting an AoI study with a longer working-distance lens, then incorporating said lens to design an endoscopic, intraoperative tumor detection device for minimally invasive surgery, with first applications in endonasal endoscopic approaches for pituitary tumors.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge