Dror Ben-Zeev
Reading Between the Lines: Combining Pause Dynamics and Semantic Coherence for Automated Assessment of Thought Disorder
Jul 17, 2025Abstract:Formal thought disorder (FTD), a hallmark of schizophrenia spectrum disorders, manifests as incoherent speech and poses challenges for clinical assessment. Traditional clinical rating scales, though validated, are resource-intensive and lack scalability. Automated speech analysis with automatic speech recognition (ASR) allows for objective quantification of linguistic and temporal features of speech, offering scalable alternatives. The use of utterance timestamps in ASR captures pause dynamics, which are thought to reflect the cognitive processes underlying speech production. However, the utility of integrating these ASR-derived features for assessing FTD severity requires further evaluation. This study integrates pause features with semantic coherence metrics across three datasets: naturalistic self-recorded diaries (AVH, n = 140), structured picture descriptions (TOPSY, n = 72), and dream narratives (PsyCL, n = 43). We evaluated pause related features alongside established coherence measures, using support vector regression (SVR) to predict clinical FTD scores. Key findings demonstrate that pause features alone robustly predict the severity of FTD. Integrating pause features with semantic coherence metrics enhanced predictive performance compared to semantic-only models, with integration of independent models achieving correlations up to \r{ho} = 0.649 and AUC = 83.71% for severe cases detection (TOPSY, with best \r{ho} = 0.584 and AUC = 79.23% for semantic-only models). The performance gains from semantic and pause features integration held consistently across all contexts, though the nature of pause patterns was dataset-dependent. These findings suggest that frameworks combining temporal and semantic analyses provide a roadmap for refining the assessment of disorganized speech and advance automated speech analysis in psychosis.
Detecting PTSD in Clinical Interviews: A Comparative Analysis of NLP Methods and Large Language Models
Apr 01, 2025Abstract:Post-Traumatic Stress Disorder (PTSD) remains underdiagnosed in clinical settings, presenting opportunities for automated detection to identify patients. This study evaluates natural language processing approaches for detecting PTSD from clinical interview transcripts. We compared general and mental health-specific transformer models (BERT/RoBERTa), embedding-based methods (SentenceBERT/LLaMA), and large language model prompting strategies (zero-shot/few-shot/chain-of-thought) using the DAIC-WOZ dataset. Domain-specific models significantly outperformed general models (Mental-RoBERTa F1=0.643 vs. RoBERTa-base 0.485). LLaMA embeddings with neural networks achieved the highest performance (F1=0.700). Zero-shot prompting using DSM-5 criteria yielded competitive results without training data (F1=0.657). Performance varied significantly across symptom severity and comorbidity status, with higher accuracy for severe PTSD cases and patients with comorbid depression. Our findings highlight the potential of domain-adapted embeddings and LLMs for scalable screening while underscoring the need for improved detection of nuanced presentations and offering insights for developing clinically viable AI tools for PTSD assessment.
Bigger But Not Better: Small Neural Language Models Outperform Large Language Models in Detection of Thought Disorder
Mar 25, 2025Abstract:Disorganized thinking is a key diagnostic indicator of schizophrenia-spectrum disorders. Recently, clinical estimates of the severity of disorganized thinking have been shown to correlate with measures of how difficult speech transcripts would be for large language models (LLMs) to predict. However, LLMs' deployment challenges -- including privacy concerns, computational and financial costs, and lack of transparency of training data -- limit their clinical utility. We investigate whether smaller neural language models can serve as effective alternatives for detecting positive formal thought disorder, using the same sliding window based perplexity measurements that proved effective with larger models. Surprisingly, our results show that smaller models are more sensitive to linguistic differences associated with formal thought disorder than their larger counterparts. Detection capability declines beyond a certain model size and context length, challenging the common assumption of ``bigger is better'' for LLM-based applications. Our findings generalize across audio diaries and clinical interview speech samples from individuals with psychotic symptoms, suggesting a promising direction for developing efficient, cost-effective, and privacy-preserving screening tools that can be deployed in both clinical and naturalistic settings.
Patient-independent Schizophrenia Relapse Prediction Using Mobile Sensor based Daily Behavioral Rhythm Changes
Jun 25, 2021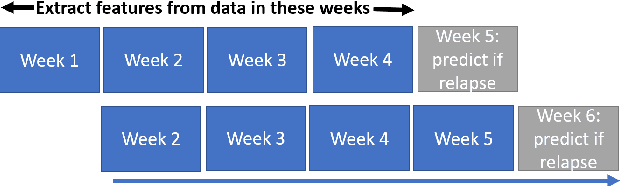
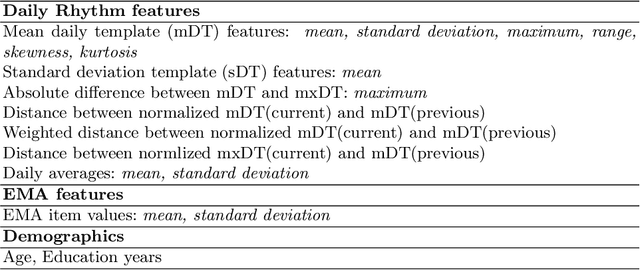
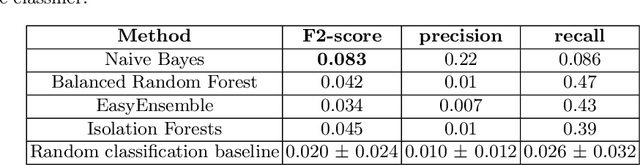
Abstract:A schizophrenia relapse has severe consequences for a patient's health, work, and sometimes even life safety. If an oncoming relapse can be predicted on time, for example by detecting early behavioral changes in patients, then interventions could be provided to prevent the relapse. In this work, we investigated a machine learning based schizophrenia relapse prediction model using mobile sensing data to characterize behavioral features. A patient-independent model providing sequential predictions, closely representing the clinical deployment scenario for relapse prediction, was evaluated. The model uses the mobile sensing data from the recent four weeks to predict an oncoming relapse in the next week. We used the behavioral rhythm features extracted from daily templates of mobile sensing data, self-reported symptoms collected via EMA (Ecological Momentary Assessment), and demographics to compare different classifiers for the relapse prediction. Naive Bayes based model gave the best results with an F2 score of 0.083 when evaluated in a dataset consisting of 63 schizophrenia patients, each monitored for up to a year. The obtained F2 score, though low, is better than the baseline performance of random classification (F2 score of 0.02 $\pm$ 0.024). Thus, mobile sensing has predictive value for detecting an oncoming relapse and needs further investigation to improve the current performance. Towards that end, further feature engineering and model personalization based on the behavioral idiosyncrasies of a patient could be helpful.
Routine Clustering of Mobile Sensor Data Facilitates Psychotic Relapse Prediction in Schizophrenia Patients
Jun 22, 2021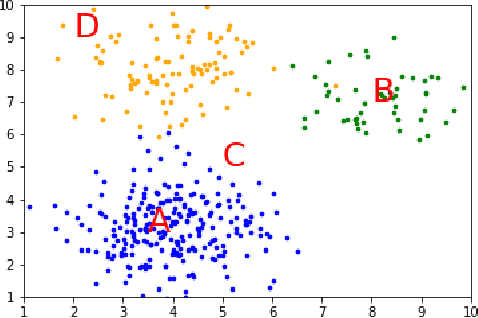
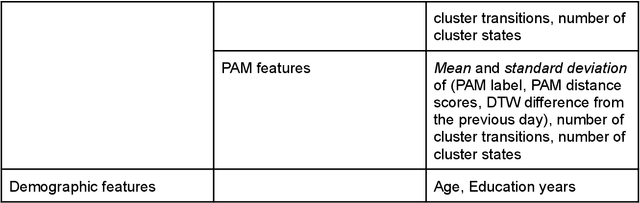
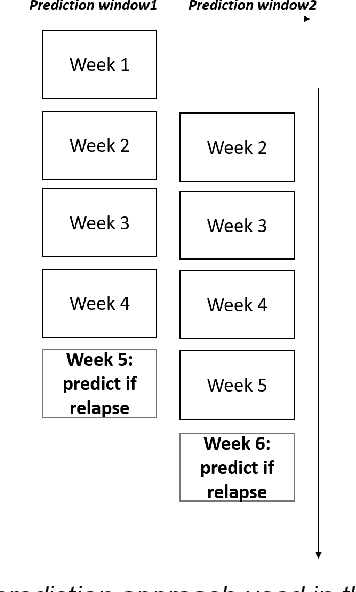

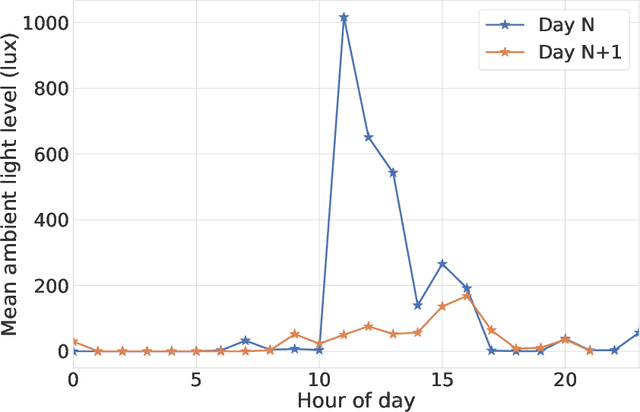
Abstract:We aim to develop clustering models to obtain behavioral representations from continuous multimodal mobile sensing data towards relapse prediction tasks. The identified clusters could represent different routine behavioral trends related to daily living of patients as well as atypical behavioral trends associated with impending relapse. We used the mobile sensing data obtained in the CrossCheck project for our analysis. Continuous data from six different mobile sensing-based modalities (e.g. ambient light, sound/conversation, acceleration etc.) obtained from a total of 63 schizophrenia patients, each monitored for up to a year, were used for the clustering models and relapse prediction evaluation. Two clustering models, Gaussian Mixture Model (GMM) and Partition Around Medoids (PAM), were used to obtain behavioral representations from the mobile sensing data. The features obtained from the clustering models were used to train and evaluate a personalized relapse prediction model using Balanced Random Forest. The personalization was done by identifying optimal features for a given patient based on a personalization subset consisting of other patients who are of similar age. The clusters identified using the GMM and PAM models were found to represent different behavioral patterns (such as clusters representing sedentary days, active but with low communications days, etc.). Significant changes near the relapse periods were seen in the obtained behavioral representation features from the clustering models. The clustering model based features, together with other features characterizing the mobile sensing data, resulted in an F2 score of 0.24 for the relapse prediction task in a leave-one-patient-out evaluation setting. This obtained F2 score is significantly higher than a random classification baseline with an average F2 score of 0.042.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge