David Scheinker
Learning Explainable Treatment Policies with Clinician-Informed Representations: A Practical Approach
Nov 26, 2024



Abstract:Digital health interventions (DHIs) and remote patient monitoring (RPM) have shown great potential in improving chronic disease management through personalized care. However, barriers like limited efficacy and workload concerns hinder adoption of existing DHIs; while limited sample sizes and lack of interpretability limit the effectiveness and adoption of purely black-box algorithmic DHIs. In this paper, we address these challenges by developing a pipeline for learning explainable treatment policies for RPM-enabled DHIs. We apply our approach in the real-world setting of RPM using a DHI to improve glycemic control of youth with type 1 diabetes. Our main contribution is to reveal the importance of clinical domain knowledge in developing state and action representations for effective, efficient, and interpretable targeting policies. We observe that policies learned from clinician-informed representations are significantly more efficacious and efficient than policies learned from black-box representations. This work emphasizes the importance of collaboration between ML researchers and clinicians for developing effective DHIs in the real world.
The Design and Implementation of a Broadly Applicable Algorithm for Optimizing Intra-Day Surgical Scheduling
Mar 14, 2022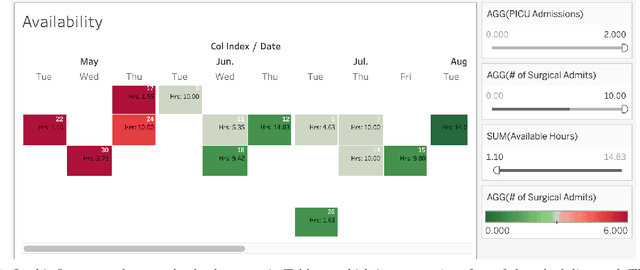
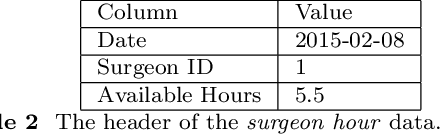
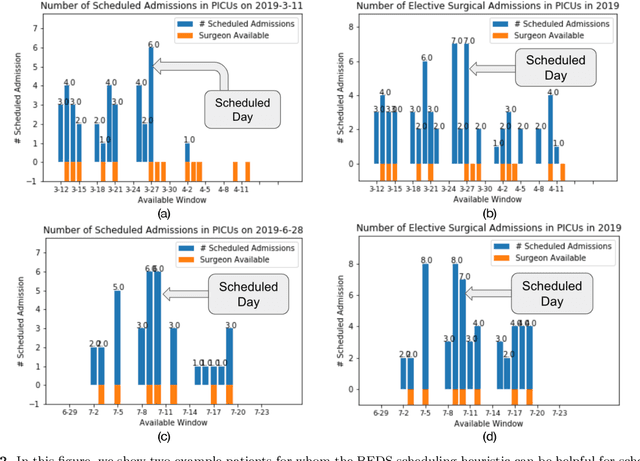
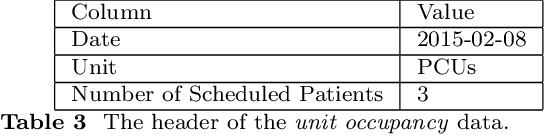
Abstract:Surgical scheduling optimization is an active area of research. However, few algorithms to optimize surgical scheduling are implemented and see sustained use. An algorithm is more likely to be implemented, if it allows for surgeon autonomy, i.e., requires only limited scheduling centralization, and functions in the limited technical infrastructure of widely used electronic medical records (EMRs). In order for an algorithm to see sustained use, it must be compatible with changes to hospital capacity, patient volumes, and scheduling practices. To meet these objectives, we developed the BEDS (better elective day of surgery) algorithm, a greedy heuristic for smoothing unit-specific surgical admissions across days. We implemented BEDS in the EMR of a large pediatric academic medical center. The use of BEDS was associated with a reduction in the variability in the number of admissions. BEDS is freely available as a dashboard in Tableau, a commercial software used by numerous hospitals. BEDS is readily implementable with the limited tools available to most hospitals, does not require reductions to surgeon autonomy or centralized scheduling, and is compatible with changes to hospital capacity or patient volumes. We present a general algorithmic framework from which BEDS is derived based on a particular choice of objectives and constraints. We argue that algorithms generated by this framework retain many of the desirable characteristics of BEDS while being compatible with a wide range of objectives and constraints.
Surgical Scheduling via Optimization and Machine Learning with Long-Tailed Data
Feb 13, 2022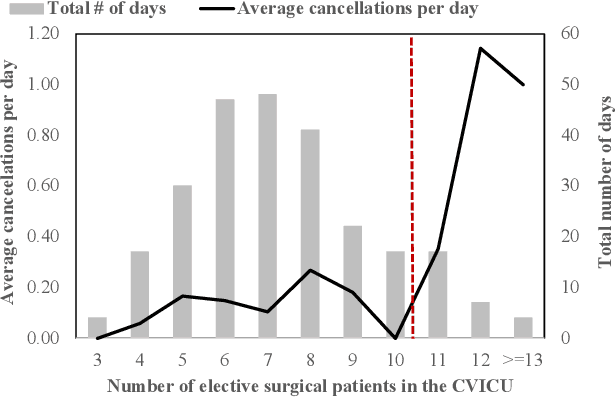
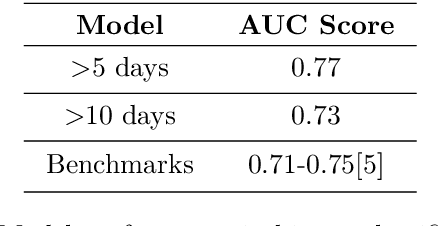
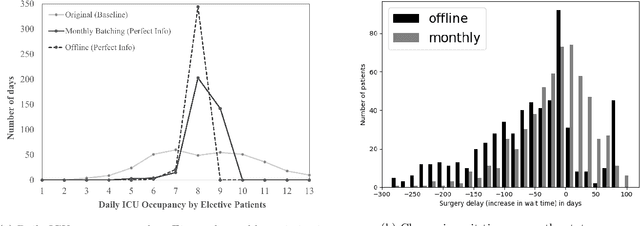
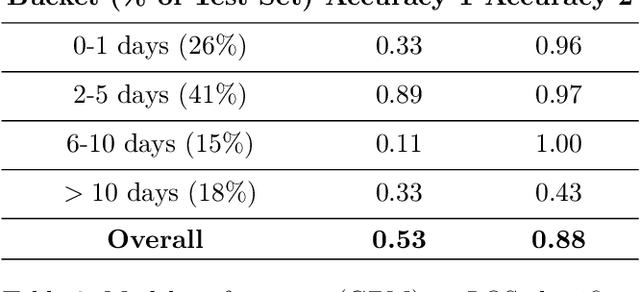
Abstract:Using data from cardiovascular surgery patients with long and highly variable post-surgical lengths of stay (LOS), we develop a model to reduce recovery unit congestion. We estimate LOS using a variety of machine learning models, schedule procedures with a variety of online optimization models, and estimate performance with simulation. The machine learning models achieved only modest LOS prediction accuracy, despite access to a very rich set of patient characteristics. Compared to the current paper-based system used in the hospital, most optimization models failed to reduce congestion without increasing wait times for surgery. A conservative stochastic optimization with sufficient sampling to capture the long tail of the LOS distribution outperformed the current manual process. These results highlight the perils of using oversimplified distributional models of patient length of stay for scheduling procedures and the importance of using stochastic optimization well-suited to dealing with long-tailed behavior.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge