Amisha Dave
Rethinking Retrieval-Augmented Generation for Medicine: A Large-Scale, Systematic Expert Evaluation and Practical Insights
Nov 10, 2025Abstract:Large language models (LLMs) are transforming the landscape of medicine, yet two fundamental challenges persist: keeping up with rapidly evolving medical knowledge and providing verifiable, evidence-grounded reasoning. Retrieval-augmented generation (RAG) has been widely adopted to address these limitations by supplementing model outputs with retrieved evidence. However, whether RAG reliably achieves these goals remains unclear. Here, we present the most comprehensive expert evaluation of RAG in medicine to date. Eighteen medical experts contributed a total of 80,502 annotations, assessing 800 model outputs generated by GPT-4o and Llama-3.1-8B across 200 real-world patient and USMLE-style queries. We systematically decomposed the RAG pipeline into three components: (i) evidence retrieval (relevance of retrieved passages), (ii) evidence selection (accuracy of evidence usage), and (iii) response generation (factuality and completeness of outputs). Contrary to expectation, standard RAG often degraded performance: only 22% of top-16 passages were relevant, evidence selection remained weak (precision 41-43%, recall 27-49%), and factuality and completeness dropped by up to 6% and 5%, respectively, compared with non-RAG variants. Retrieval and evidence selection remain key failure points for the model, contributing to the overall performance drop. We further show that simple yet effective strategies, including evidence filtering and query reformulation, substantially mitigate these issues, improving performance on MedMCQA and MedXpertQA by up to 12% and 8.2%, respectively. These findings call for re-examining RAG's role in medicine and highlight the importance of stage-aware evaluation and deliberate system design for reliable medical LLM applications.
Enhancing Large Language Models with Domain-specific Retrieval Augment Generation: A Case Study on Long-form Consumer Health Question Answering in Ophthalmology
Sep 20, 2024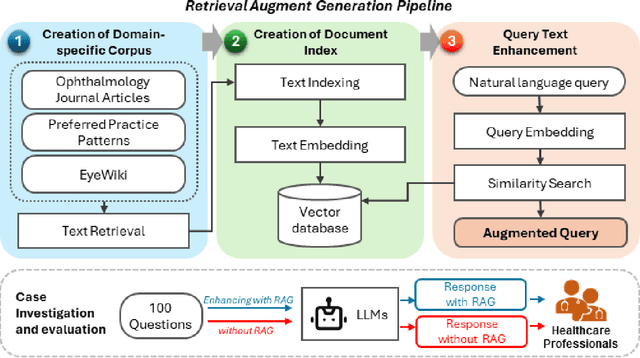
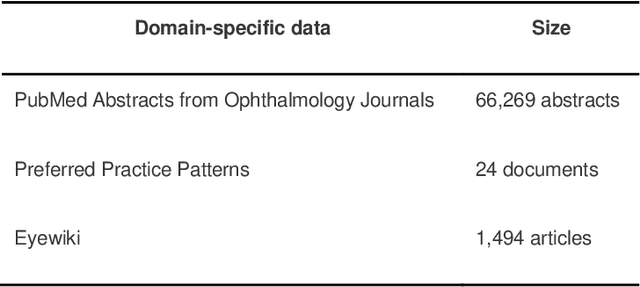
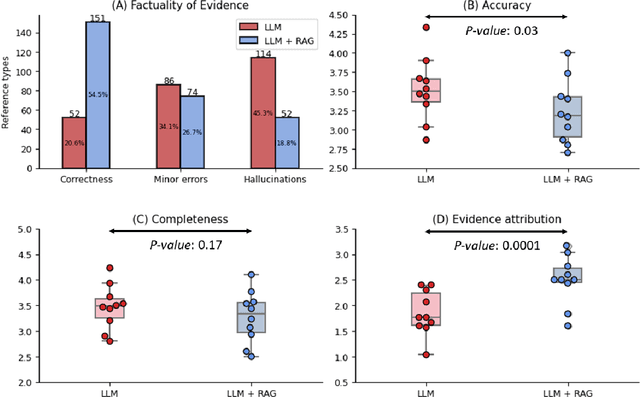

Abstract:Despite the potential of Large Language Models (LLMs) in medicine, they may generate responses lacking supporting evidence or based on hallucinated evidence. While Retrieval Augment Generation (RAG) is popular to address this issue, few studies implemented and evaluated RAG in downstream domain-specific applications. We developed a RAG pipeline with 70,000 ophthalmology-specific documents that retrieve relevant documents to augment LLMs during inference time. In a case study on long-form consumer health questions, we systematically evaluated the responses including over 500 references of LLMs with and without RAG on 100 questions with 10 healthcare professionals. The evaluation focuses on factuality of evidence, selection and ranking of evidence, attribution of evidence, and answer accuracy and completeness. LLMs without RAG provided 252 references in total. Of which, 45.3% hallucinated, 34.1% consisted of minor errors, and 20.6% were correct. In contrast, LLMs with RAG significantly improved accuracy (54.5% being correct) and reduced error rates (18.8% with minor hallucinations and 26.7% with errors). 62.5% of the top 10 documents retrieved by RAG were selected as the top references in the LLM response, with an average ranking of 4.9. The use of RAG also improved evidence attribution (increasing from 1.85 to 2.49 on a 5-point scale, P<0.001), albeit with slight decreases in accuracy (from 3.52 to 3.23, P=0.03) and completeness (from 3.47 to 3.27, P=0.17). The results demonstrate that LLMs frequently exhibited hallucinated and erroneous evidence in the responses, raising concerns for downstream applications in the medical domain. RAG substantially reduced the proportion of such evidence but encountered challenges.
MedCalc-Bench: Evaluating Large Language Models for Medical Calculations
Jun 17, 2024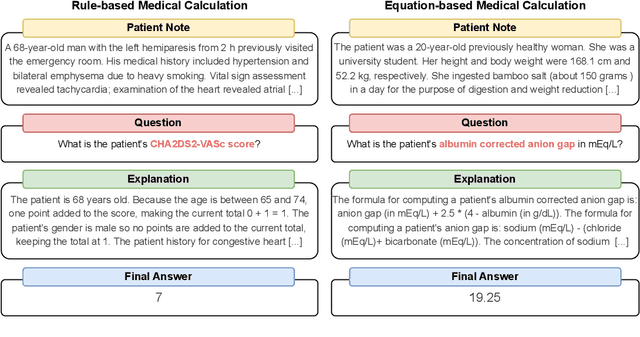
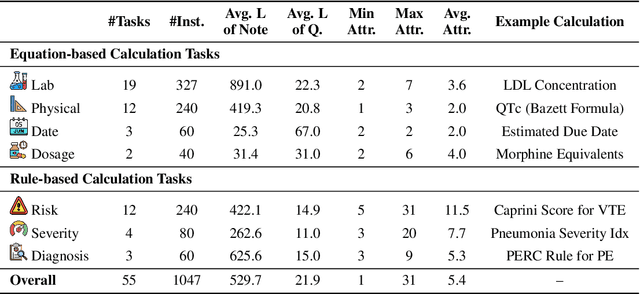
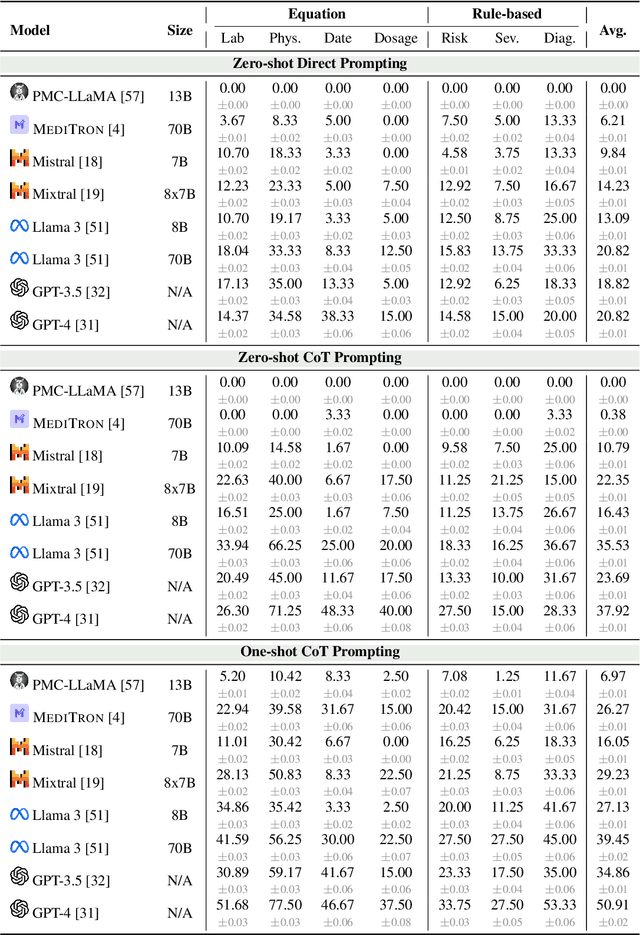
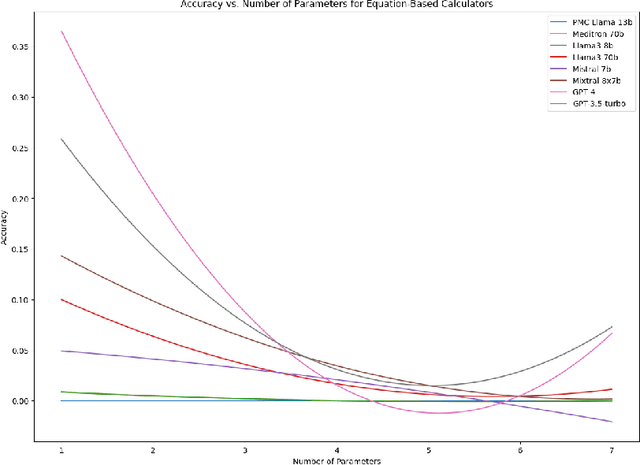
Abstract:As opposed to evaluating computation and logic-based reasoning, current bench2 marks for evaluating large language models (LLMs) in medicine are primarily focused on question-answering involving domain knowledge and descriptive rea4 soning. While such qualitative capabilities are vital to medical diagnosis, in real5 world scenarios, doctors frequently use clinical calculators that follow quantitative equations and rule-based reasoning paradigms for evidence-based decision support. To this end, we propose MedCalc-Bench, a first-of-its-kind dataset focused on evaluating the medical calculation capability of LLMs. MedCalc-Bench contains an evaluation set of over 1000 manually reviewed instances from 55 different medical calculation tasks. Each instance in MedCalc-Bench consists of a patient note, a question requesting to compute a specific medical value, a ground truth answer, and a step-by-step explanation showing how the answer is obtained. While our evaluation results show the potential of LLMs in this area, none of them are effective enough for clinical settings. Common issues include extracting the incorrect entities, not using the correct equation or rules for a calculation task, or incorrectly performing the arithmetic for the computation. We hope our study highlights the quantitative knowledge and reasoning gaps in LLMs within medical settings, encouraging future improvements of LLMs for various clinical calculation tasks.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge