A. Ian Wong
WorldMedQA-V: a multilingual, multimodal medical examination dataset for multimodal language models evaluation
Oct 16, 2024Abstract:Multimodal/vision language models (VLMs) are increasingly being deployed in healthcare settings worldwide, necessitating robust benchmarks to ensure their safety, efficacy, and fairness. Multiple-choice question and answer (QA) datasets derived from national medical examinations have long served as valuable evaluation tools, but existing datasets are largely text-only and available in a limited subset of languages and countries. To address these challenges, we present WorldMedQA-V, an updated multilingual, multimodal benchmarking dataset designed to evaluate VLMs in healthcare. WorldMedQA-V includes 568 labeled multiple-choice QAs paired with 568 medical images from four countries (Brazil, Israel, Japan, and Spain), covering original languages and validated English translations by native clinicians, respectively. Baseline performance for common open- and closed-source models are provided in the local language and English translations, and with and without images provided to the model. The WorldMedQA-V benchmark aims to better match AI systems to the diverse healthcare environments in which they are deployed, fostering more equitable, effective, and representative applications.
Evaluating the Impact of Pulse Oximetry Bias in Machine Learning under Counterfactual Thinking
Aug 08, 2024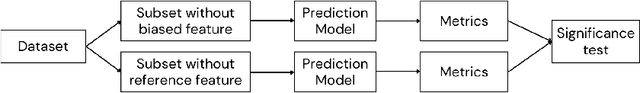
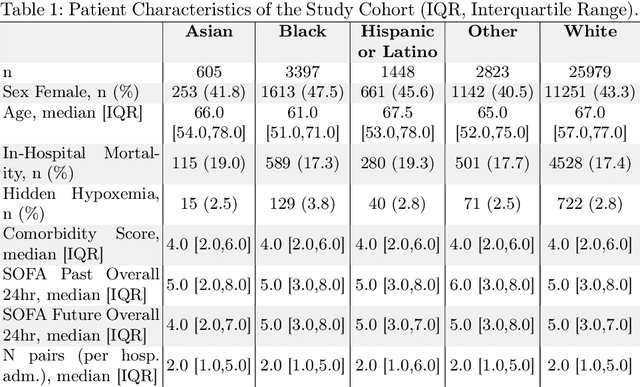
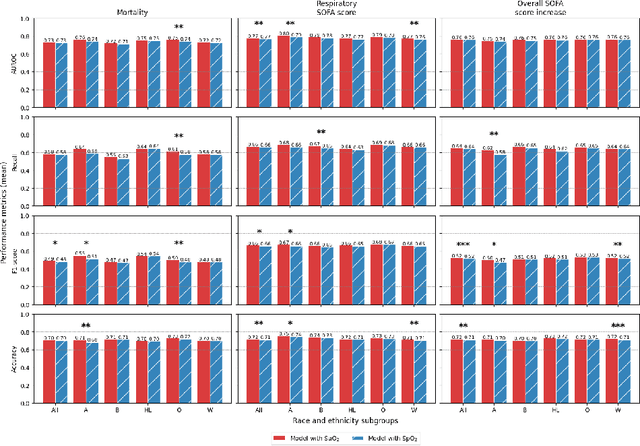

Abstract:Algorithmic bias in healthcare mirrors existing data biases. However, the factors driving unfairness are not always known. Medical devices capture significant amounts of data but are prone to errors; for instance, pulse oximeters overestimate the arterial oxygen saturation of darker-skinned individuals, leading to worse outcomes. The impact of this bias in machine learning (ML) models remains unclear. This study addresses the technical challenges of quantifying the impact of medical device bias in downstream ML. Our experiments compare a "perfect world", without pulse oximetry bias, using SaO2 (blood-gas), to the "actual world", with biased measurements, using SpO2 (pulse oximetry). Under this counterfactual design, two models are trained with identical data, features, and settings, except for the method of measuring oxygen saturation: models using SaO2 are a "control" and models using SpO2 a "treatment". The blood-gas oximetry linked dataset was a suitable test-bed, containing 163,396 nearly-simultaneous SpO2 - SaO2 paired measurements, aligned with a wide array of clinical features and outcomes. We studied three classification tasks: in-hospital mortality, respiratory SOFA score in the next 24 hours, and SOFA score increase by two points. Models using SaO2 instead of SpO2 generally showed better performance. Patients with overestimation of O2 by pulse oximetry of > 3% had significant decreases in mortality prediction recall, from 0.63 to 0.59, P < 0.001. This mirrors clinical processes where biased pulse oximetry readings provide clinicians with false reassurance of patients' oxygen levels. A similar degradation happened in ML models, with pulse oximetry biases leading to more false negatives in predicting adverse outcomes.
EHRmonize: A Framework for Medical Concept Abstraction from Electronic Health Records using Large Language Models
Jun 28, 2024



Abstract:Electronic health records (EHRs) contain vast amounts of complex data, but harmonizing and processing this information remains a challenging and costly task requiring significant clinical expertise. While large language models (LLMs) have shown promise in various healthcare applications, their potential for abstracting medical concepts from EHRs remains largely unexplored. We introduce EHRmonize, a framework leveraging LLMs to abstract medical concepts from EHR data. Our study uses medication data from two real-world EHR databases to evaluate five LLMs on two free-text extraction and six binary classification tasks across various prompting strategies. GPT-4o's with 10-shot prompting achieved the highest performance in all tasks, accompanied by Claude-3.5-Sonnet in a subset of tasks. GPT-4o achieved an accuracy of 97% in identifying generic route names, 82% for generic drug names, and 100% in performing binary classification of antibiotics. While EHRmonize significantly enhances efficiency, reducing annotation time by an estimated 60%, we emphasize that clinician oversight remains essential. Our framework, available as a Python package, offers a promising tool to assist clinicians in EHR data abstraction, potentially accelerating healthcare research and improving data harmonization processes.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge