Ying Sha
Beyond Words: Enhancing Desire, Emotion, and Sentiment Recognition with Non-Verbal Cues
Sep 19, 2025

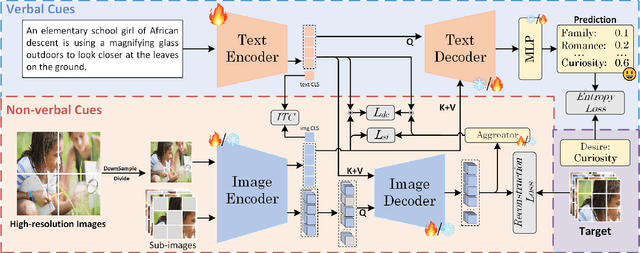
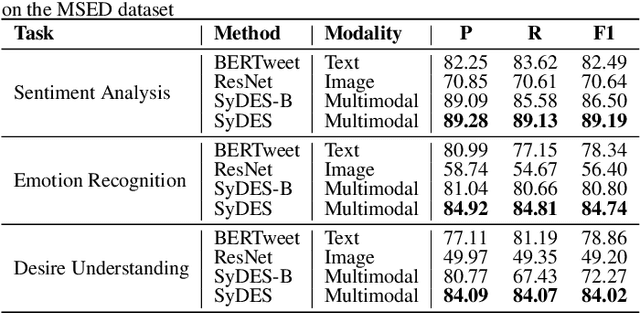
Abstract:Desire, as an intention that drives human behavior, is closely related to both emotion and sentiment. Multimodal learning has advanced sentiment and emotion recognition, but multimodal approaches specially targeting human desire understanding remain underexplored. And existing methods in sentiment analysis predominantly emphasize verbal cues and overlook images as complementary non-verbal cues. To address these gaps, we propose a Symmetrical Bidirectional Multimodal Learning Framework for Desire, Emotion, and Sentiment Recognition, which enforces mutual guidance between text and image modalities to effectively capture intention-related representations in the image. Specifically, low-resolution images are used to obtain global visual representations for cross-modal alignment, while high resolution images are partitioned into sub-images and modeled with masked image modeling to enhance the ability to capture fine-grained local features. A text-guided image decoder and an image-guided text decoder are introduced to facilitate deep cross-modal interaction at both local and global representations of image information. Additionally, to balance perceptual gains with computation cost, a mixed-scale image strategy is adopted, where high-resolution images are cropped into sub-images for masked modeling. The proposed approach is evaluated on MSED, a multimodal dataset that includes a desire understanding benchmark, as well as emotion and sentiment recognition. Experimental results indicate consistent improvements over other state-of-the-art methods, validating the effectiveness of our proposed method. Specifically, our method outperforms existing approaches, achieving F1-score improvements of 1.1% in desire understanding, 0.6% in emotion recognition, and 0.9% in sentiment analysis. Our code is available at: https://github.com/especiallyW/SyDES.
Keyword-Oriented Multimodal Modeling for Euphemism Identification
Mar 27, 2025Abstract:Euphemism identification deciphers the true meaning of euphemisms, such as linking "weed" (euphemism) to "marijuana" (target keyword) in illicit texts, aiding content moderation and combating underground markets. While existing methods are primarily text-based, the rise of social media highlights the need for multimodal analysis, incorporating text, images, and audio. However, the lack of multimodal datasets for euphemisms limits further research. To address this, we regard euphemisms and their corresponding target keywords as keywords and first introduce a keyword-oriented multimodal corpus of euphemisms (KOM-Euph), involving three datasets (Drug, Weapon, and Sexuality), including text, images, and speech. We further propose a keyword-oriented multimodal euphemism identification method (KOM-EI), which uses cross-modal feature alignment and dynamic fusion modules to explicitly utilize the visual and audio features of the keywords for efficient euphemism identification. Extensive experiments demonstrate that KOM-EI outperforms state-of-the-art models and large language models, and show the importance of our multimodal datasets.
RCLMuFN: Relational Context Learning and Multiplex Fusion Network for Multimodal Sarcasm Detection
Dec 17, 2024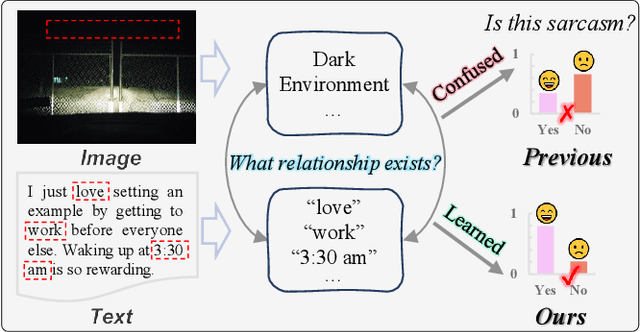
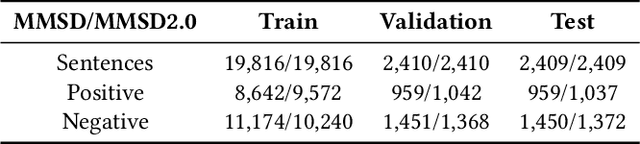
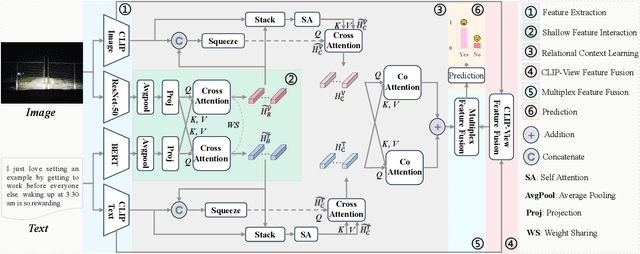

Abstract:Sarcasm typically conveys emotions of contempt or criticism by expressing a meaning that is contrary to the speaker's true intent. Accurate detection of sarcasm aids in identifying and filtering undesirable information on the Internet, thereby reducing malicious defamation and rumor-mongering. Nonetheless, the task of automatic sarcasm detection remains highly challenging for machines, as it critically depends on intricate factors such as relational context. Most existing multimodal sarcasm detection methods focus on introducing graph structures to establish entity relationships between text and images while neglecting to learn the relational context between text and images, which is crucial evidence for understanding the meaning of sarcasm. In addition, the meaning of sarcasm changes with the evolution of different contexts, but existing methods may not be accurate in modeling such dynamic changes, limiting the generalization ability of the models. To address the above issues, we propose a relational context learning and multiplex fusion network (RCLMuFN) for multimodal sarcasm detection. Firstly, we employ four feature extractors to comprehensively extract features from raw text and images, aiming to excavate potential features that may have been previously overlooked. Secondly, we utilize the relational context learning module to learn the contextual information of text and images and capture the dynamic properties through shallow and deep interactions. Finally, we employ a multiplex feature fusion module to enhance the generalization of the model by penetratingly integrating multimodal features derived from various interaction contexts. Extensive experiments on two multimodal sarcasm detection datasets show that our proposed method achieves state-of-the-art performance.
Explainable Artificial Intelligence Methods in Combating Pandemics: A Systematic Review
Dec 25, 2021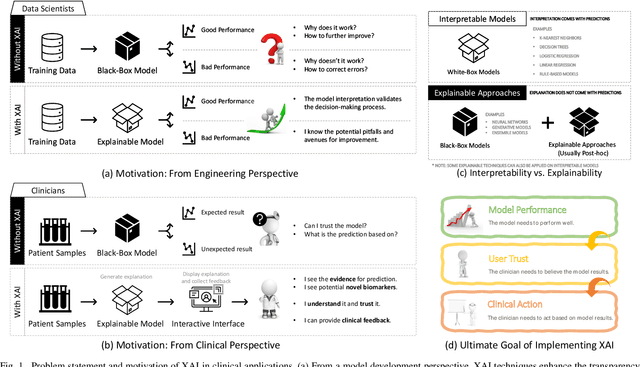
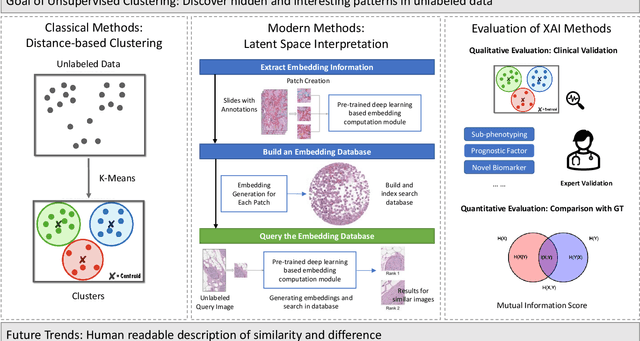
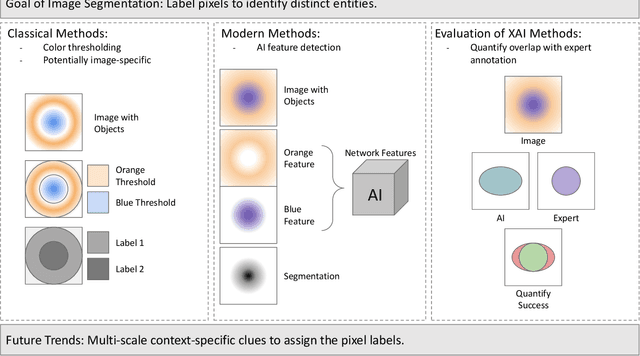
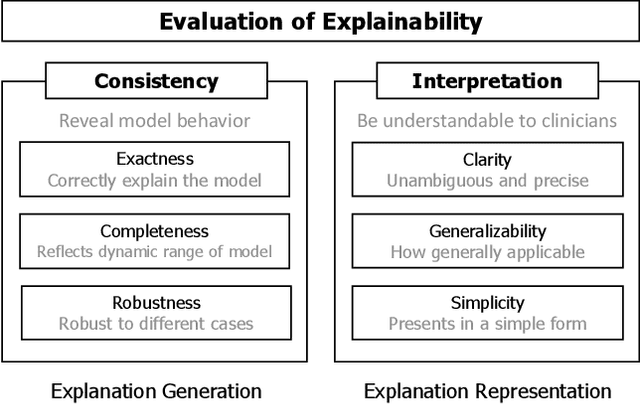
Abstract:Despite the myriad peer-reviewed papers demonstrating novel Artificial Intelligence (AI)-based solutions to COVID-19 challenges during the pandemic, few have made significant clinical impact. The impact of artificial intelligence during the COVID-19 pandemic was greatly limited by lack of model transparency. This systematic review examines the use of Explainable Artificial Intelligence (XAI) during the pandemic and how its use could overcome barriers to real-world success. We find that successful use of XAI can improve model performance, instill trust in the end-user, and provide the value needed to affect user decision-making. We introduce the reader to common XAI techniques, their utility, and specific examples of their application. Evaluation of XAI results is also discussed as an important step to maximize the value of AI-based clinical decision support systems. We illustrate the classical, modern, and potential future trends of XAI to elucidate the evolution of novel XAI techniques. Finally, we provide a checklist of suggestions during the experimental design process supported by recent publications. Common challenges during the implementation of AI solutions are also addressed with specific examples of potential solutions. We hope this review may serve as a guide to improve the clinical impact of future AI-based solutions.
Public Health Informatics: Proposing Causal Sequence of Death Using Neural Machine Translation
Sep 22, 2020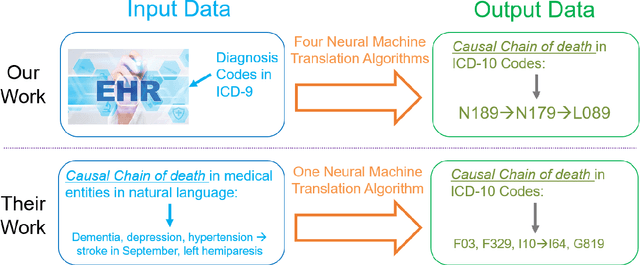
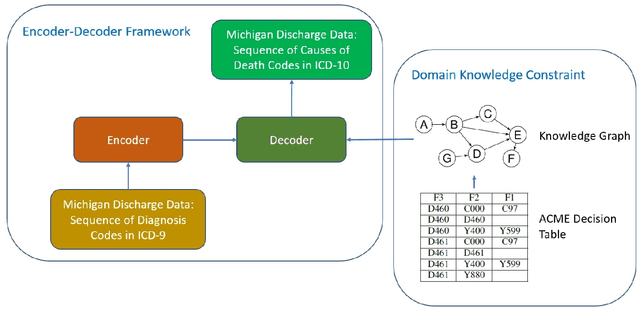
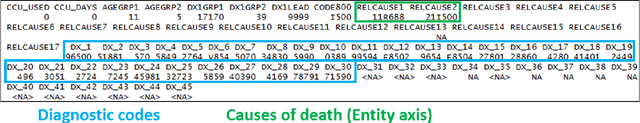
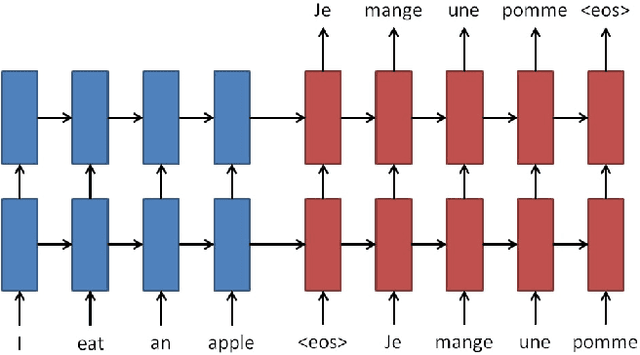
Abstract:Each year there are nearly 57 million deaths around the world, with over 2.7 million in the United States. Timely, accurate and complete death reporting is critical in public health, as institutions and government agencies rely on death reports to analyze vital statistics and to formulate responses to communicable diseases. Inaccurate death reporting may result in potential misdirection of public health policies. Determining the causes of death is, nevertheless, challenging even for experienced physicians. To facilitate physicians in accurately reporting causes of death, we present an advanced AI approach to determine a chronically ordered sequence of clinical conditions that lead to death, based on decedent's last hospital admission discharge record. The sequence of clinical codes on the death report is named as causal chain of death, coded in the tenth revision of International Statistical Classification of Diseases (ICD-10); the priority-ordered clinical conditions on the discharge record are coded in ICD-9. We identify three challenges in proposing the causal chain of death: two versions of coding system in clinical codes, medical domain knowledge conflict, and data interoperability. To overcome the first challenge in this sequence-to-sequence problem, we apply neural machine translation models to generate target sequence. We evaluate the quality of generated sequences with the BLEU (BiLingual Evaluation Understudy) score and achieve 16.44 out of 100. To address the second challenge, we incorporate expert-verified medical domain knowledge as constraint in generating output sequence to exclude infeasible causal chains. Lastly, we demonstrate the usability of our work in a Fast Healthcare Interoperability Resources (FHIR) interface to address the third challenge.
DeepDeath: Learning to Predict the Underlying Cause of Death with Big Data
May 06, 2017
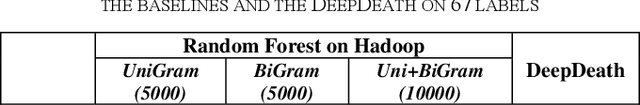
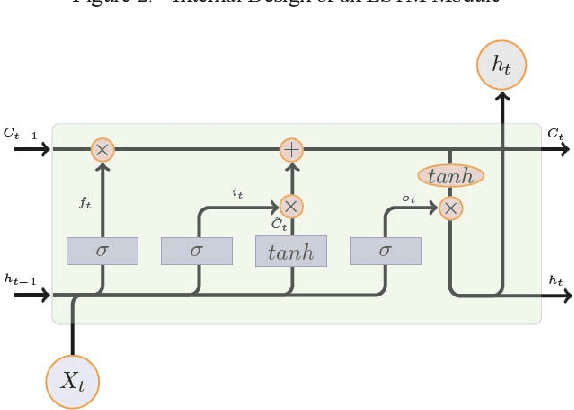
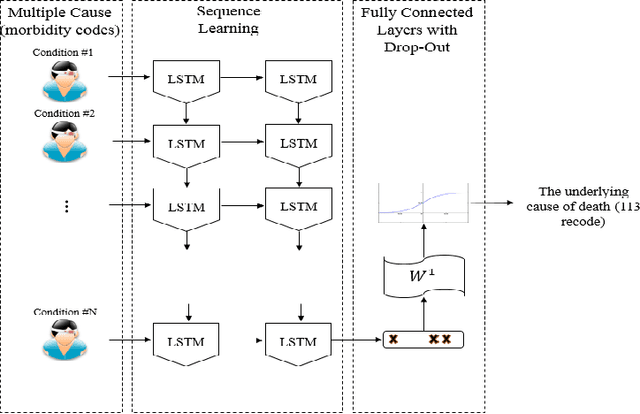
Abstract:Multiple cause-of-death data provides a valuable source of information that can be used to enhance health standards by predicting health related trajectories in societies with large populations. These data are often available in large quantities across U.S. states and require Big Data techniques to uncover complex hidden patterns. We design two different classes of models suitable for large-scale analysis of mortality data, a Hadoop-based ensemble of random forests trained over N-grams, and the DeepDeath, a deep classifier based on the recurrent neural network (RNN). We apply both classes to the mortality data provided by the National Center for Health Statistics and show that while both perform significantly better than the random classifier, the deep model that utilizes long short-term memory networks (LSTMs), surpasses the N-gram based models and is capable of learning the temporal aspect of the data without a need for building ad-hoc, expert-driven features.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge