Razeyeh Bagherinasab
Automated Body Composition Analysis Using DAFS Express on 2D MRI Slices at L3 Vertebral Level
Sep 11, 2024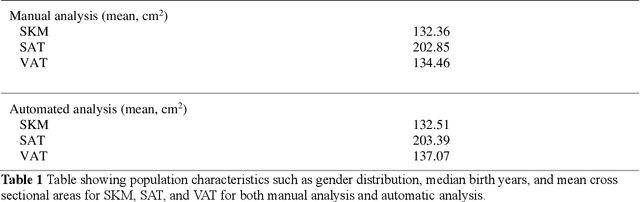
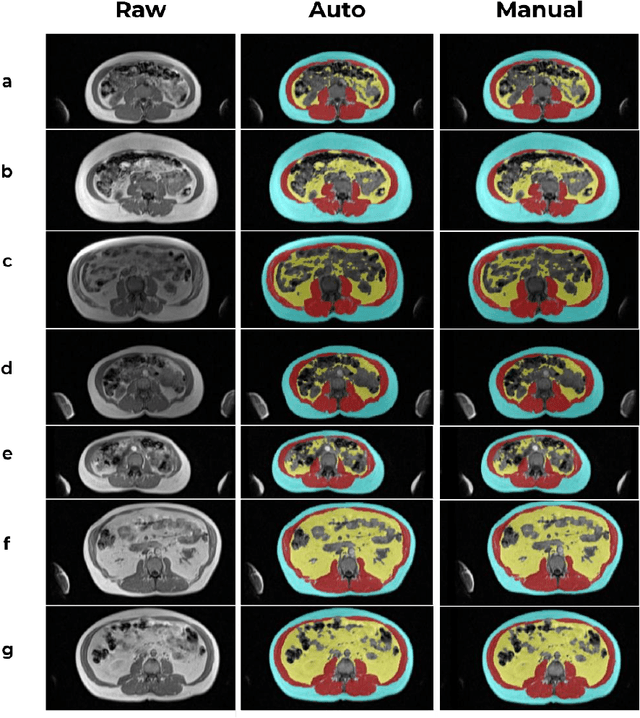
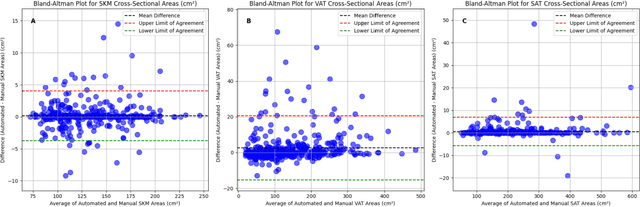
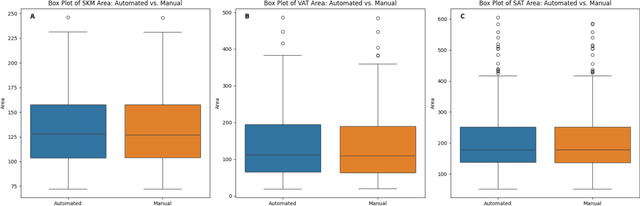
Abstract:Body composition analysis is vital in assessing health conditions such as obesity, sarcopenia, and metabolic syndromes. MRI provides detailed images of skeletal muscle (SKM), visceral adipose tissue (VAT), and subcutaneous adipose tissue (SAT), but their manual segmentation is labor-intensive and limits clinical applicability. This study validates an automated tool for MRI-based 2D body composition analysis- (Data Analysis Facilitation Suite (DAFS) Express), comparing its automated measurements with expert manual segmentations using UK Biobank data. A cohort of 399 participants from the UK Biobank dataset was selected, yielding 423 single L3 slices for analysis. DAFS Express performed automated segmentations of SKM, VAT, and SAT, which were then manually corrected by expert raters for validation. Evaluation metrics included Jaccard coefficients, Dice scores, Intraclass Correlation Coefficients (ICCs), and Bland-Altman Plots to assess segmentation agreement and reliability. High agreements were observed between automated and manual segmentations with mean Jaccard scores: SKM 99.03%, VAT 95.25%, and SAT 99.57%; and mean Dice scores: SKM 99.51%, VAT 97.41%, and SAT 99.78%. Cross-sectional area comparisons showed consistent measurements with automated methods closely matching manual measurements for SKM and SAT, and slightly higher values for VAT (SKM: Auto 132.51 cm^2, Manual 132.36 cm^2; VAT: Auto 137.07 cm^2, Manual 134.46 cm^2; SAT: Auto 203.39 cm^2, Manual 202.85 cm^2). ICCs confirmed strong reliability (SKM: 0.998, VAT: 0.994, SAT: 0.994). Bland-Altman plots revealed minimal biases, and boxplots illustrated distribution similarities across SKM, VAT, and SAT areas. On average DAFS Express took 18 seconds per DICOM. This underscores its potential to streamline image analysis processes in research and clinical settings, enhancing diagnostic accuracy and efficiency.
Transcervical Ultrasound Image Guidance System for Transoral Robotic Surgery
Nov 29, 2022Abstract:Purpose: Trans-oral robotic surgery (TORS) using the da Vinci surgical robot is a new minimally-invasive surgery method to treat oropharyngeal tumors, but it is a challenging operation. Augmented reality (AR) based on intra-operative ultrasound (US) has the potential to enhance the visualization of the anatomy and cancerous tumors to provide additional tools for decision-making in surgery. Methods: We propose and carry out preliminary evaluations of a US-guided AR system for TORS, with the transducer placed on the neck for a transcervical view. Firstly, we perform a novel MRI-transcervical 3D US registration study. Secondly, we develop a US-robot calibration method with an optical tracker and an AR system to display the anatomy mesh model in the real-time endoscope images inside the surgeon console. Results: Our AR system reaches a mean projection error of 26.81 and 27.85 pixels for the projection from the US to stereo cameras in a water bath experiment. The average target registration error for MRI to 3D US is 8.90 mm for the 3D US transducer and 5.85 mm for freehand 3D US, and the average distance between the vessel centerlines is 2.32 mm. Conclusion: We demonstrate the first proof-of-concept transcervical US-guided AR system for TORS and the feasibility of trans-cervical 3D US-MRI registration. Our results show that trans-cervical 3D US is a promising technique for TORS image guidance.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge