Mohammadreza Chavoshi
Feature Quality and Adaptability of Medical Foundation Models: A Comparative Evaluation for Radiographic Classification and Segmentation
Nov 12, 2025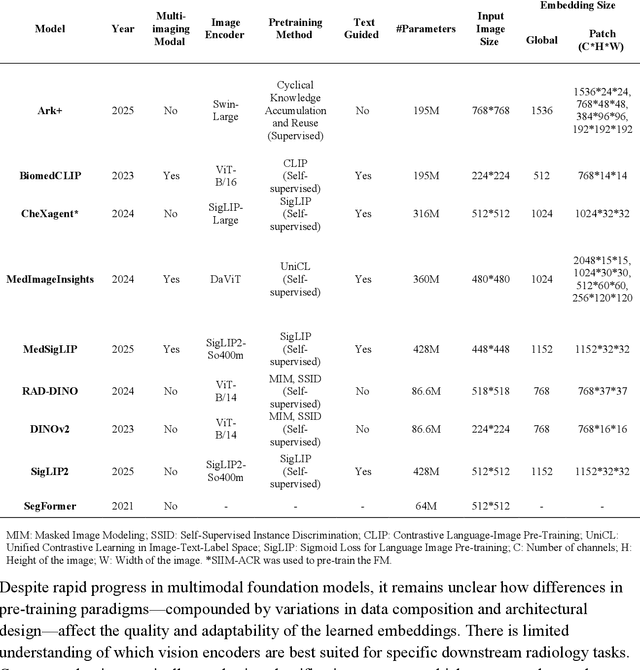
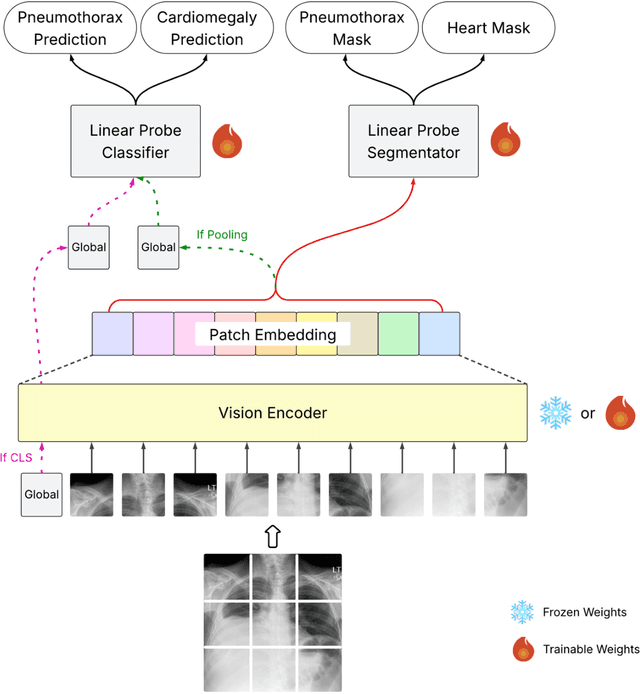
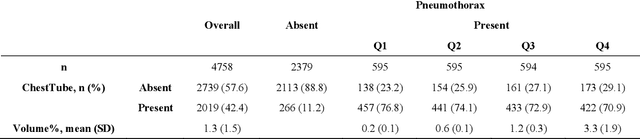
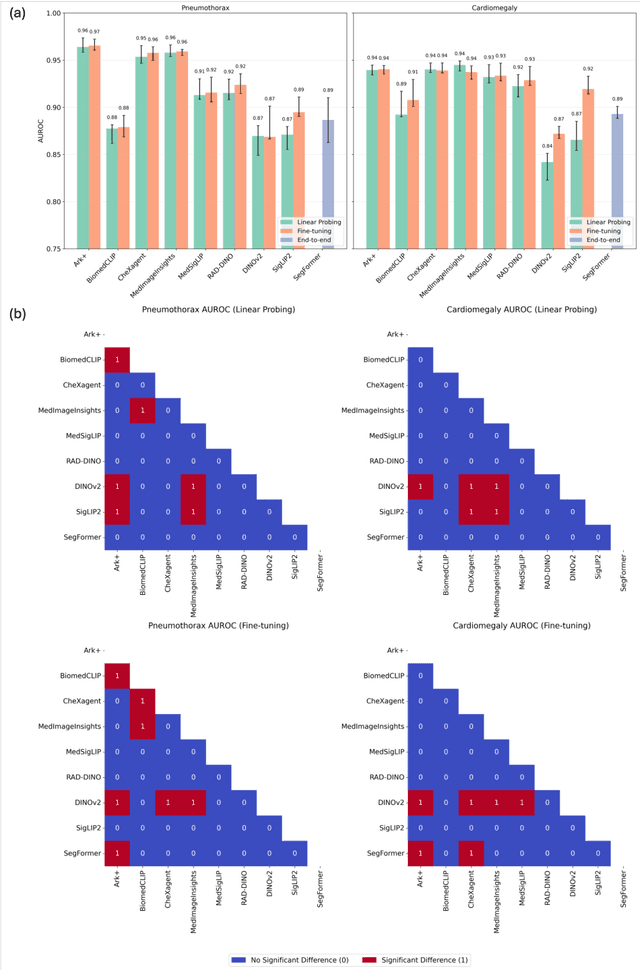
Abstract:Foundation models (FMs) promise to generalize medical imaging, but their effectiveness varies. It remains unclear how pre-training domain (medical vs. general), paradigm (e.g., text-guided), and architecture influence embedding quality, hindering the selection of optimal encoders for specific radiology tasks. To address this, we evaluate vision encoders from eight medical and general-domain FMs for chest X-ray analysis. We benchmark classification (pneumothorax, cardiomegaly) and segmentation (pneumothorax, cardiac boundary) using linear probing and fine-tuning. Our results show that domain-specific pre-training provides a significant advantage; medical FMs consistently outperformed general-domain models in linear probing, establishing superior initial feature quality. However, feature utility is highly task-dependent. Pre-trained embeddings were strong for global classification and segmenting salient anatomy (e.g., heart). In contrast, for segmenting complex, subtle pathologies (e.g., pneumothorax), all FMs performed poorly without significant fine-tuning, revealing a critical gap in localizing subtle disease. Subgroup analysis showed FMs use confounding shortcuts (e.g., chest tubes for pneumothorax) for classification, a strategy that fails for precise segmentation. We also found that expensive text-image alignment is not a prerequisite; image-only (RAD-DINO) and label-supervised (Ark+) FMs were among top performers. Notably, a supervised, end-to-end baseline remained highly competitive, matching or exceeding the best FMs on segmentation tasks. These findings show that while medical pre-training is beneficial, architectural choices (e.g., multi-scale) are critical, and pre-trained features are not universally effective, especially for complex localization tasks where supervised models remain a strong alternative.
Evaluating Vision Language Models (VLMs) for Radiology: A Comprehensive Analysis
Apr 22, 2025



Abstract:Foundation models, trained on vast amounts of data using self-supervised techniques, have emerged as a promising frontier for advancing artificial intelligence (AI) applications in medicine. This study evaluates three different vision-language foundation models (RAD-DINO, CheXagent, and BiomedCLIP) on their ability to capture fine-grained imaging features for radiology tasks. The models were assessed across classification, segmentation, and regression tasks for pneumothorax and cardiomegaly on chest radiographs. Self-supervised RAD-DINO consistently excelled in segmentation tasks, while text-supervised CheXagent demonstrated superior classification performance. BiomedCLIP showed inconsistent performance across tasks. A custom segmentation model that integrates global and local features substantially improved performance for all foundation models, particularly for challenging pneumothorax segmentation. The findings highlight that pre-training methodology significantly influences model performance on specific downstream tasks. For fine-grained segmentation tasks, models trained without text supervision performed better, while text-supervised models offered advantages in classification and interpretability. These insights provide guidance for selecting foundation models based on specific clinical applications in radiology.
Novel AI-Based Quantification of Breast Arterial Calcification to Predict Cardiovascular Risk
Mar 17, 2025Abstract:Women are underdiagnosed and undertreated for cardiovascular disease. Automatic quantification of breast arterial calcification on screening mammography can identify women at risk for cardiovascular disease and enable earlier treatment and management of disease. In this retrospective study of 116,135 women from two healthcare systems, a transformer-based neural network quantified BAC severity (no BAC, mild, moderate, and severe) on screening mammograms. Outcomes included major adverse cardiovascular events (MACE) and all-cause mortality. BAC severity was independently associated with MACE after adjusting for cardiovascular risk factors, with increasing hazard ratios from mild (HR 1.18-1.22), moderate (HR 1.38-1.47), to severe BAC (HR 2.03-2.22) across datasets (all p<0.001). This association remained significant across all age groups, with even mild BAC indicating increased risk in women under 50. BAC remained an independent predictor when analyzed alongside ASCVD risk scores, showing significant associations with myocardial infarction, stroke, heart failure, and mortality (all p<0.005). Automated BAC quantification enables opportunistic cardiovascular risk assessment during routine mammography without additional radiation or cost. This approach provides value beyond traditional risk factors, particularly in younger women, offering potential for early CVD risk stratification in the millions of women undergoing annual mammography.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge