Jennifer A. Pacheco
Natural language processing to identify lupus nephritis phenotype in electronic health records
Dec 20, 2021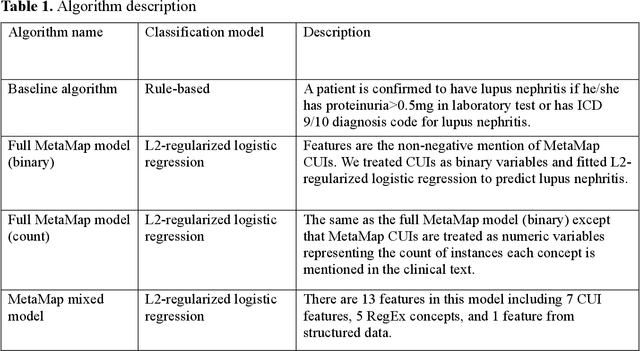
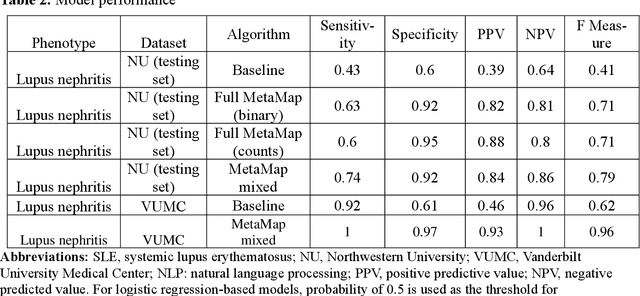
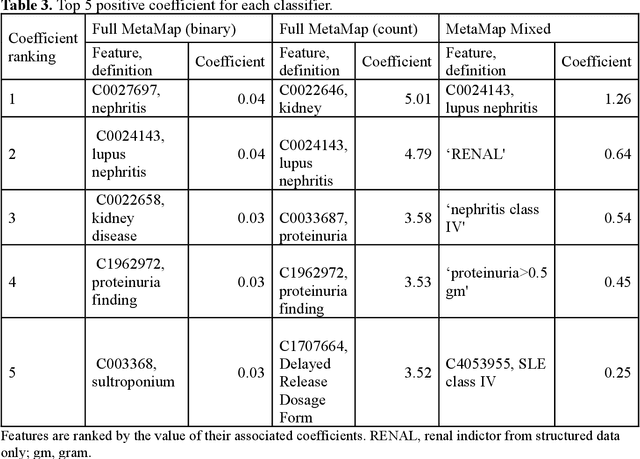
Abstract:Systemic lupus erythematosus (SLE) is a rare autoimmune disorder characterized by an unpredictable course of flares and remission with diverse manifestations. Lupus nephritis, one of the major disease manifestations of SLE for organ damage and mortality, is a key component of lupus classification criteria. Accurately identifying lupus nephritis in electronic health records (EHRs) would therefore benefit large cohort observational studies and clinical trials where characterization of the patient population is critical for recruitment, study design, and analysis. Lupus nephritis can be recognized through procedure codes and structured data, such as laboratory tests. However, other critical information documenting lupus nephritis, such as histologic reports from kidney biopsies and prior medical history narratives, require sophisticated text processing to mine information from pathology reports and clinical notes. In this study, we developed algorithms to identify lupus nephritis with and without natural language processing (NLP) using EHR data. We developed four algorithms: a rule-based algorithm using only structured data (baseline algorithm) and three algorithms using different NLP models. The three NLP models are based on regularized logistic regression and use different sets of features including positive mention of concept unique identifiers (CUIs), number of appearances of CUIs, and a mixture of three components respectively. The baseline algorithm and the best performed NLP algorithm were external validated on a dataset from Vanderbilt University Medical Center (VUMC). Our best performing NLP model incorporating features from both structured data, regular expression concepts, and mapped CUIs improved F measure in both the NMEDW (0.41 vs 0.79) and VUMC (0.62 vs 0.96) datasets compared to the baseline lupus nephritis algorithm.
Identification of Predictive Sub-Phenotypes of Acute Kidney Injury using Structured and Unstructured Electronic Health Record Data with Memory Networks
Apr 10, 2019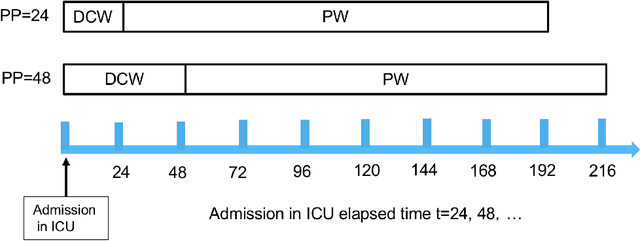
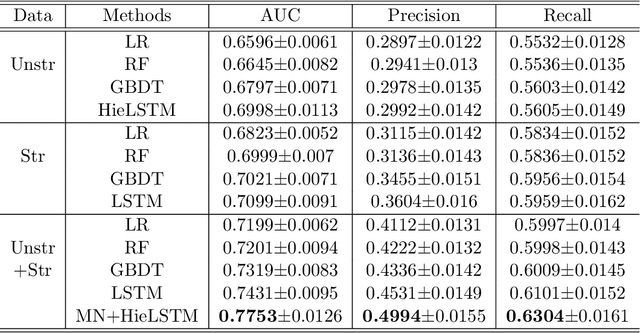
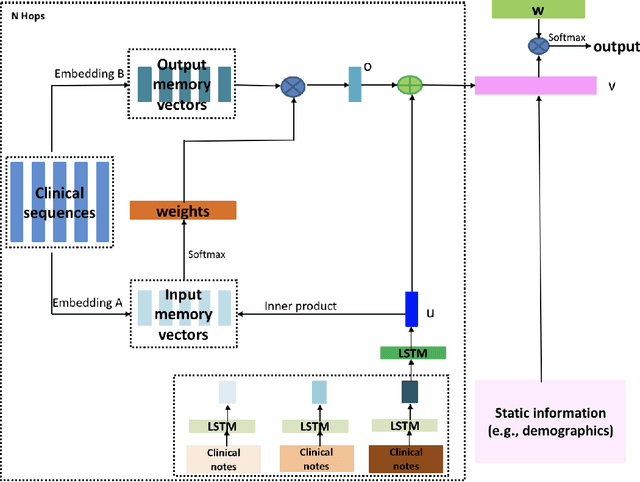
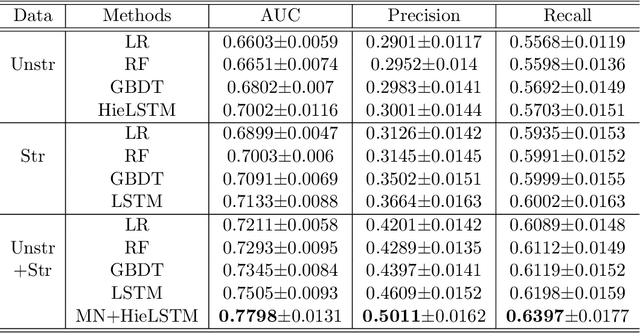
Abstract:Acute Kidney Injury (AKI) is a common clinical syndrome characterized by the rapid loss of kidney excretory function, which aggravates the clinical severity of other diseases in a large number of hospitalized patients. Accurate early prediction of AKI can enable in-time interventions and treatments. However, AKI is highly heterogeneous, thus identification of AKI sub-phenotypes can lead to an improved understanding of the disease pathophysiology and development of more targeted clinical interventions. This study used a memory network-based deep learning approach to discover predictive AKI sub-phenotypes using structured and unstructured electronic health record (EHR) data of patients before AKI diagnosis. We leveraged a real world critical care EHR corpus including 37,486 ICU stays. Our approach identified three distinct sub-phenotypes: sub-phenotype I is with an average age of 63.03$ \pm 17.25 $ years, and is characterized by mild loss of kidney excretory function (Serum Creatinne (SCr) $1.55\pm 0.34$ mg/dL, estimated Glomerular Filtration Rate Test (eGFR) $107.65\pm 54.98$ mL/min/1.73$m^2$). These patients are more likely to develop stage I AKI. Sub-phenotype II is with average age 66.81$ \pm 10.43 $ years, and was characterized by severe loss of kidney excretory function (SCr $1.96\pm 0.49$ mg/dL, eGFR $82.19\pm 55.92$ mL/min/1.73$m^2$). These patients are more likely to develop stage III AKI. Sub-phenotype III is with average age 65.07$ \pm 11.32 $ years, and was characterized moderate loss of kidney excretory function and thus more likely to develop stage II AKI (SCr $1.69\pm 0.32$ mg/dL, eGFR $93.97\pm 56.53$ mL/min/1.73$m^2$). Both SCr and eGFR are significantly different across the three sub-phenotypes with statistical testing plus postdoc analysis, and the conclusion still holds after age adjustment.
Evaluating the Portability of an NLP System for Processing Echocardiograms: A Retrospective, Multi-site Observational Study
Apr 02, 2019

Abstract:While natural language processing (NLP) of unstructured clinical narratives holds the potential for patient care and clinical research, portability of NLP approaches across multiple sites remains a major challenge. This study investigated the portability of an NLP system developed initially at the Department of Veterans Affairs (VA) to extract 27 key cardiac concepts from free-text or semi-structured echocardiograms from three academic medical centers: Weill Cornell Medicine, Mayo Clinic and Northwestern Medicine. While the NLP system showed high precision and recall measurements for four target concepts (aortic valve regurgitation, left atrium size at end systole, mitral valve regurgitation, tricuspid valve regurgitation) across all sites, we found moderate or poor results for the remaining concepts and the NLP system performance varied between individual sites.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge