Janos Hajagos
A Methodological Framework for the Comparative Evaluation of Multiple Imputation Methods: Multiple Imputation of Race, Ethnicity and Body Mass Index in the U.S. National COVID Cohort Collaborative
Jun 13, 2022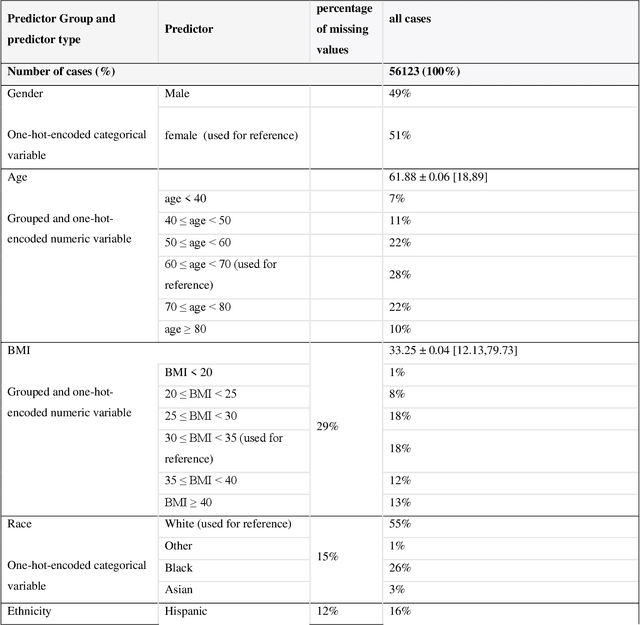
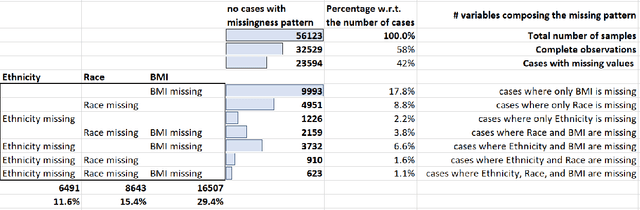
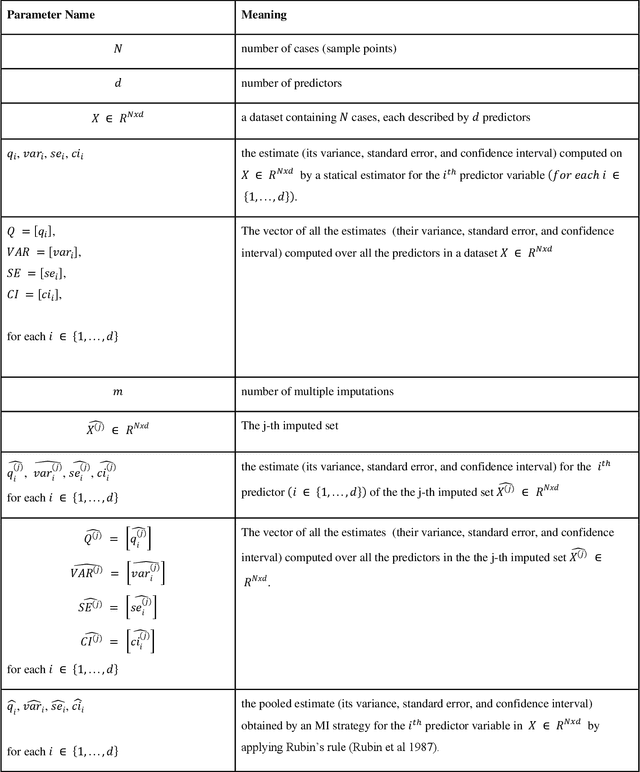
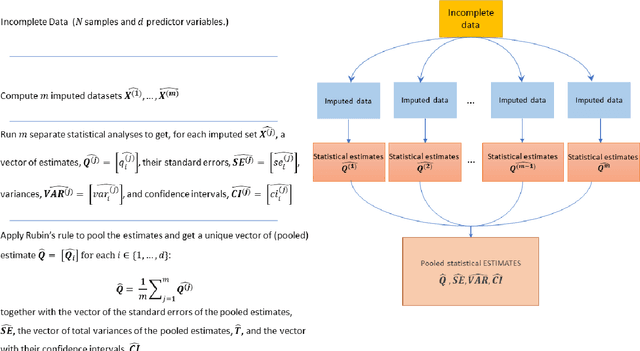
Abstract:While electronic health records are a rich data source for biomedical research, these systems are not implemented uniformly across healthcare settings and significant data may be missing due to healthcare fragmentation and lack of interoperability between siloed electronic health records. Considering that the deletion of cases with missing data may introduce severe bias in the subsequent analysis, several authors prefer applying a multiple imputation strategy to recover the missing information. Unfortunately, although several literature works have documented promising results by using any of the different multiple imputation algorithms that are now freely available for research, there is no consensus on which MI algorithm works best. Beside the choice of the MI strategy, the choice of the imputation algorithm and its application settings are also both crucial and challenging. In this paper, inspired by the seminal works of Rubin and van Buuren, we propose a methodological framework that may be applied to evaluate and compare several multiple imputation techniques, with the aim to choose the most valid for computing inferences in a clinical research work. Our framework has been applied to validate, and extend on a larger cohort, the results we presented in a previous literature study, where we evaluated the influence of crucial patients' descriptors and COVID-19 severity in patients with type 2 diabetes mellitus whose data is provided by the National COVID Cohort Collaborative Enclave.
Disease phenotyping using deep learning: A diabetes case study
Nov 28, 2018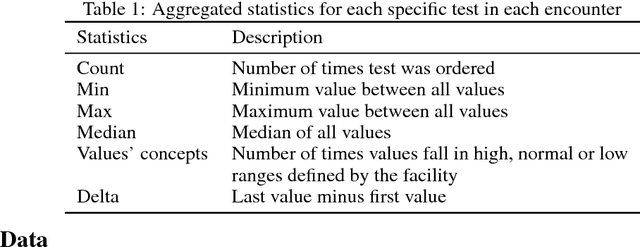
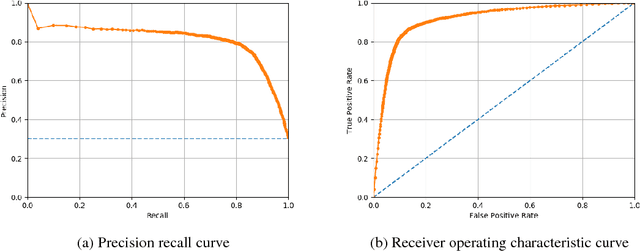
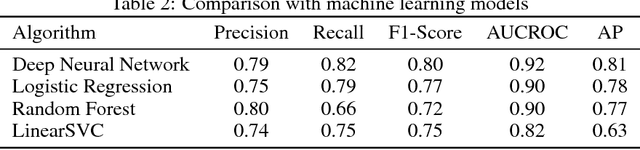
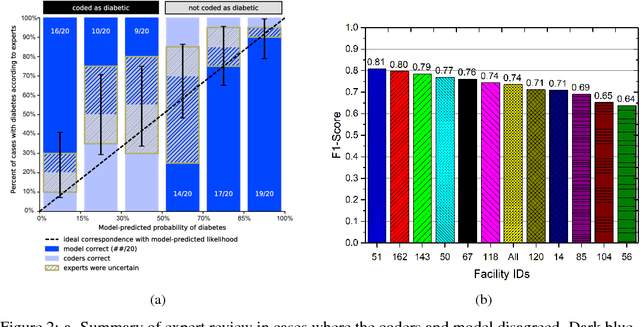
Abstract:Characterization of a patient clinical phenotype is central to biomedical informatics. ICD codes, assigned to inpatient encounters by coders, is important for population health and cohort discovery when clinical information is limited. While ICD codes are assigned to patients by professionals trained and certified in coding there is substantial variability in coding. We present a methodology that uses deep learning methods to model coder decision making and that predicts ICD codes. Our approach predicts codes based on demographics, lab results, and medications, as well as codes from previous encounters. We are able to predict existing codes with high accuracy for all three of the test cases we investigated: diabetes, acute renal failure, and chronic kidney disease. We employed a panel of clinicians, in a blinded manner, to assess ground truth and compared the predictions of coders, model and clinicians. When disparities between the model prediction and coder assigned codes were reviewed, our model outperformed coder assigned ICD codes.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge