Yuria Utsumi
Closing the Gap in High-Risk Pregnancy Care Using Machine Learning and Human-AI Collaboration
May 26, 2023



Abstract:Health insurers often use algorithms to identify members who would benefit from care and condition management programs, which provide personalized, high-touch clinical support. Timely, accurate, and seamless integration between algorithmic identification and clinical intervention depends on effective collaboration between the system designers and nurse care managers. We focus on a high-risk pregnancy (HRP) program designed to reduce the likelihood of adverse prenatal, perinatal, and postnatal events and describe how we overcome three challenges of HRP programs as articulated by nurse care managers; (1) early detection of pregnancy, (2) accurate identification of impactable high-risk members, and (3) provision of explainable indicators to supplement predictions. We propose a novel algorithm for pregnancy identification that identifies pregnancies 57 days earlier than previous code-based models in a retrospective study. We then build a model to predict impactable pregnancy complications that achieves an AUROC of 0.760. Models for pregnancy identification and complications are then integrated into a proposed user interface. In a set of user studies, we collected quantitative and qualitative feedback from nurses on the utility of the predictions combined with clinical information driving the predictions on triaging members for the HRP program.
Meta-Weighted Gaussian Process Experts for Personalized Forecasting of AD Cognitive Changes
Apr 19, 2019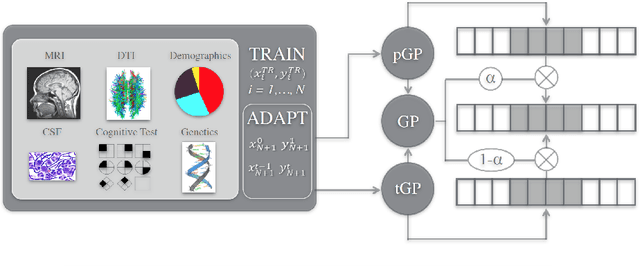
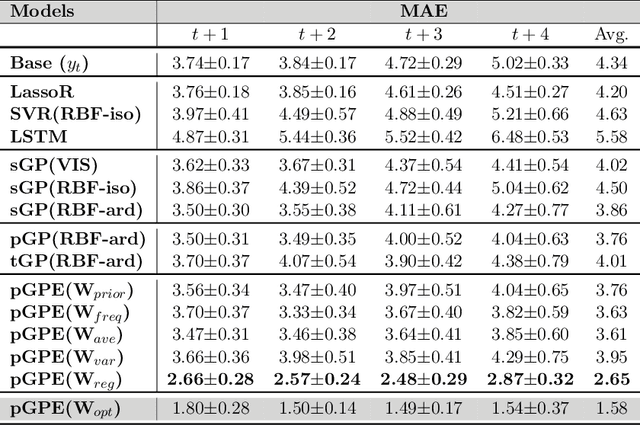
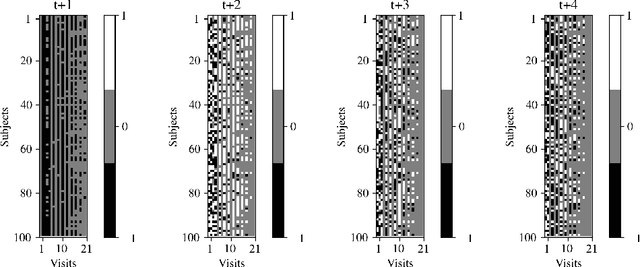
Abstract:We introduce a novel personalized Gaussian Process Experts (pGPE) model for predicting per-subject ADAS-Cog13 cognitive scores -- a significant predictor of Alzheimer's Disease (AD) in the cognitive domain -- over the future 6, 12, 18, and 24 months. We start by training a population-level model using multi-modal data from previously seen subjects using a base Gaussian Process (GP) regression. Then, we personalize this model by adapting the base GP sequentially over time to a new (target) subject using domain adaptive GPs, and also by training subject-specific GP. While we show that these models achieve improved performance when selectively applied to the forecasting task (one performs better than the other on different subjects/visits), the average performance per model is suboptimal. To this end, we used the notion of meta learning in the proposed pGPE to design a regression-based weighting of these expert models, where the expert weights are optimized for each subject and his/her future visit. The results on a cohort of subjects from the ADNI dataset show that this newly introduced personalized weighting of the expert models leads to large improvements in accurately forecasting future ADAS-Cog13 scores and their fine-grained changes associated with the AD progression. This approach has potential to help identify at-risk patients early and improve the construction of clinical trials for AD.
Personalized Gaussian Processes for Forecasting of Alzheimer's Disease Assessment Scale-Cognition Sub-Scale (ADAS-Cog13)
May 04, 2018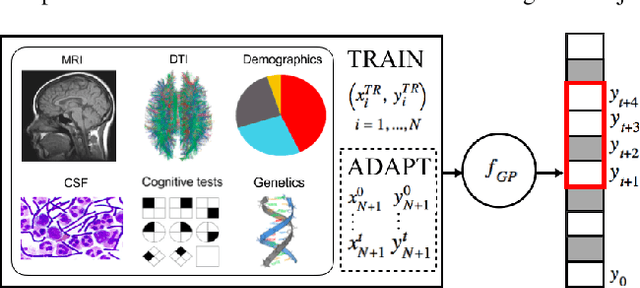
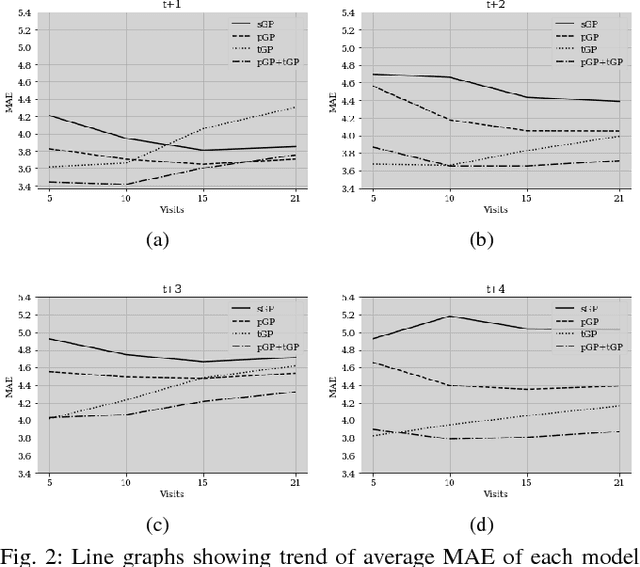

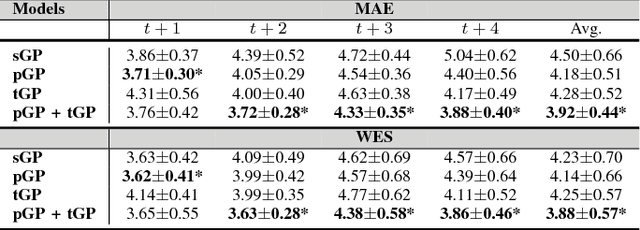
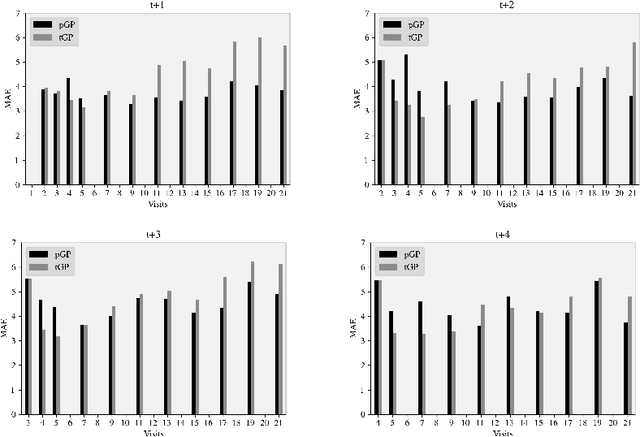
Abstract:In this paper, we introduce the use of a personalized Gaussian Process model (pGP) to predict per-patient changes in ADAS-Cog13 -- a significant predictor of Alzheimer's Disease (AD) in the cognitive domain -- using data from each patient's previous visits, and testing on future (held-out) data. We start by learning a population-level model using multi-modal data from previously seen patients using a base Gaussian Process (GP) regression. The personalized GP (pGP) is formed by adapting the base GP sequentially over time to a new (target) patient using domain adaptive GPs. We extend this personalized approach to predict the values of ADAS-Cog13 over the future 6, 12, 18, and 24 months. We compare this approach to a GP model trained only on past data of the target patients (tGP), as well as to a new approach that combines pGP with tGP. We find that the new approach, combining pGP with tGP, leads to large improvements in accurately forecasting future ADAS-Cog13 scores.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge