Theresa Urban
1-3
Influence of Medical Foreign Bodies on Dark-Field Chest Radiographs: First experiences
Aug 20, 2024Abstract:Objectives: Evaluating the effects and artifacts introduced by medical foreign bodies in clinical dark-field chest radiographs and assessing their influence on the evaluation of pulmonary tissue, compared to conventional radiographs. Material & Methods: This retrospective study analyzed data from subjects enrolled in clinical trials conducted between 2018 and 2021, focusing on chronic obstructive pulmonary disease (COPD) and COVID-19 patients. All patients obtained a radiograph using an in-house developed clinical prototype for grating-based dark-field chest radiography. The prototype simultaneously delivers a conventional and dark-field radiograph. Two radiologists independently assessed the clinical studies to identify patients with foreign bodies. Subsequently, an analysis was conducted on the effects and artifacts attributed to distinct foreign bodies and their impact on the assessment of pulmonary tissue. Results: Overall, 30 subjects with foreign bodies were included in this study (mean age, 64 years +/- 11 [standard deviation]; 15 men). Foreign bodies composed of materials lacking microstructure exhibited a diminished dark-field signal or no discernible signal. Foreign bodies with a microstructure, in our investigations the cementation of the kyphoplasty, produce a positive dark-field signal. Since most foreign bodies lack microstructural features, dark-field imaging revealed fewer signals and artifacts by foreign bodies compared to conventional radiographs. Conclusion: Dark-field radiography enhances the assessment of pulmonary tissue with overlaying foreign bodies compared to conventional radiography. Reduced interfering signals result in fewer overlapping radiopaque artifacts within the investigated regions. This mitigates the impact on image quality and interpretability of the radiographs and the projection-related limitations of radiography compared to CT.
Optimizing Convolutional Neural Networks for Chronic Obstructive Pulmonary Disease Detection in Clinical Computed Tomography Imaging
Mar 13, 2023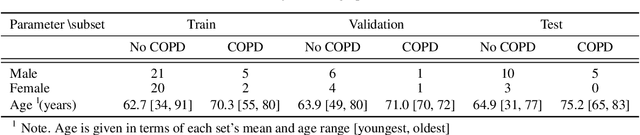
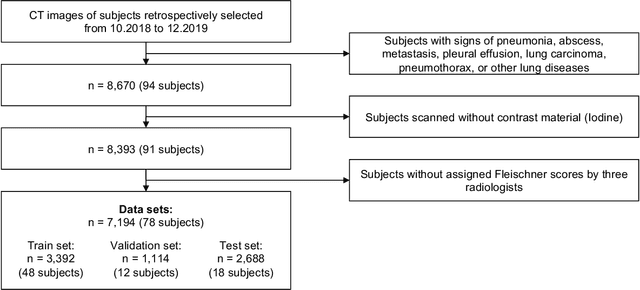
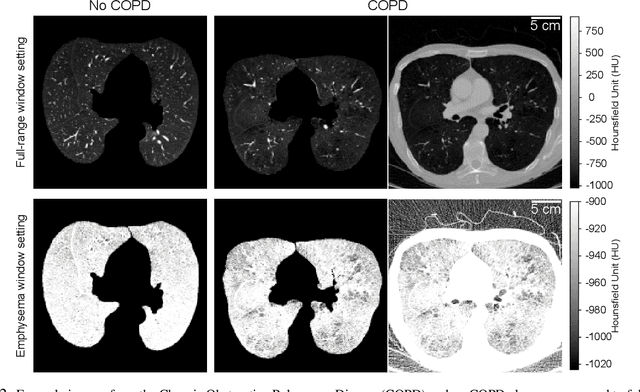
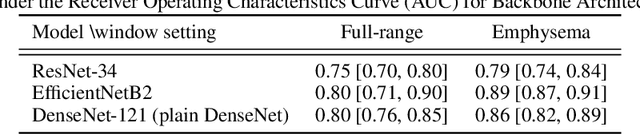
Abstract:Chronic Obstructive Pulmonary Disease (COPD) is a leading cause of death worldwide, yet early detection and treatment can prevent the progression of the disease. In contrast to the conventional method of detecting COPD with spirometry tests, X-ray Computed Tomography (CT) scans of the chest provide a measure of morphological changes in the lung. It has been shown that automated detection of COPD can be performed with deep learning models. However, the potential of incorporating optimal window setting selection, typically carried out by clinicians during examination of CT scans for COPD, is generally overlooked in deep learning approaches. We aim to optimize the binary classification of COPD with densely connected convolutional neural networks (DenseNets) through implementation of manual and automated Window-Setting Optimization (WSO) steps. Our dataset consisted of 78 CT scans from the Klinikum rechts der Isar research hospital. Repeated inference on the test set showed that without WSO, the plain DenseNet resulted in a mean slice-level AUC of 0.80$\pm$0.05. With input images manually adjusted to the emphysema window setting, the plain DenseNet model predicted COPD with a mean AUC of 0.86$\pm$0.04. By automating the WSO through addition of a customized layer to the DenseNet, an optimal window setting in the proximity of the emphysema window setting was learned and a mean AUC of 0.82$\pm$0.04 was achieved. Detection of COPD with DenseNet models was optimized by WSO of CT data to the emphysema window setting range, demonstrating the importance of implementing optimal window setting selection in the deep learning pipeline.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge