Mahdi Saadatmand
Deep learning and traditional-based CAD schemes for the pulmonary embolism diagnosis: A survey
Dec 03, 2023Abstract:Nowadays, pulmonary Computed Tomography Angiography (CTA) is the main tool for detecting Pulmonary Embolism (PE). However, manual interpretation of CTA volume requires a radiologist, which is time-consuming and error-prone due to the specific conditions of lung tissue, large volume of data, lack of experience, and eye fatigue. Therefore, Computer-Aided Design (CAD) systems are used as a second opinion for the diagnosis of PE. The purpose of this article is to review, evaluate, and compare the performance of deep learning and traditional-based CAD system for diagnosis PE and to help physicians and researchers in this field. In this study, all articles available in databases such as IEEE, ScienceDirect, Wiley, Springer, Nature, and Wolters Kluwer in the field of PE diagnosis were examined using traditional and deep learning methods. From 2002 to 2023, 23 papers were studied to extract the articles with the considered limitations. Each paper presents an automatic PE detection system that we evaluate using criteria such as sensitivity, False Positives (FP), and the number of datasets. This research work includes recent studies, state-of-the-art research works, and a more comprehensive overview compared to previously published review articles in this research area.
Computer Aided Detection for Pulmonary Embolism Challenge (CAD-PE)
Mar 30, 2020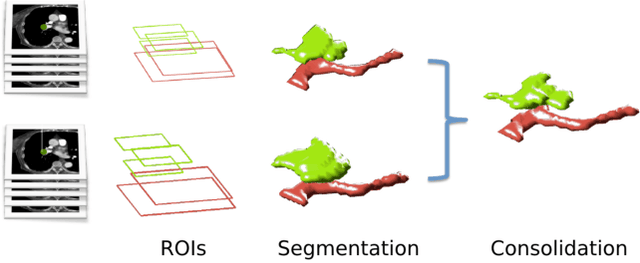
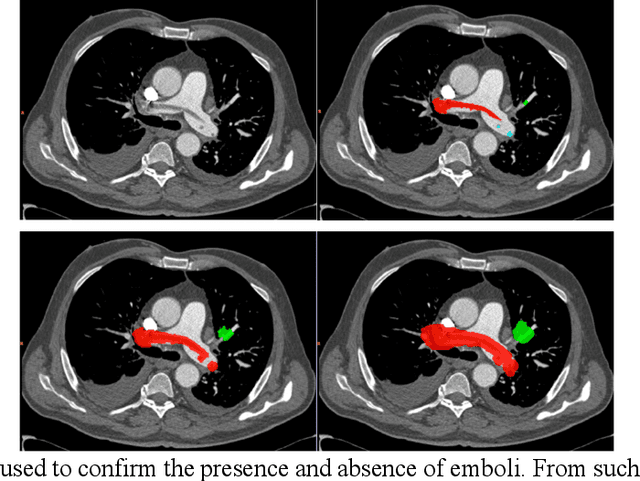
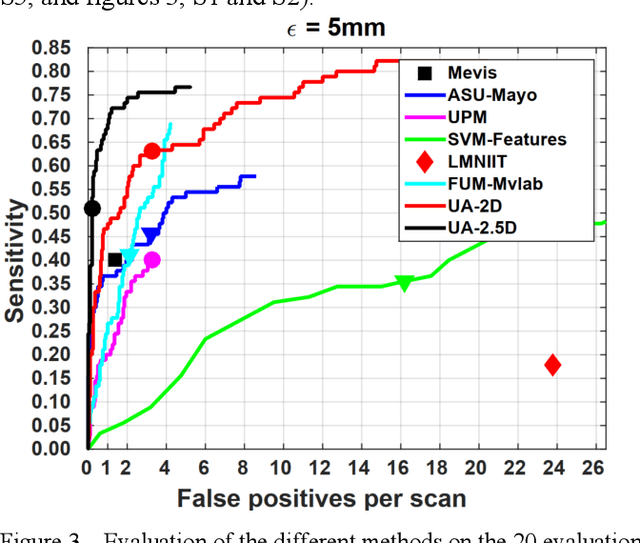
Abstract:Rationale: Computer aided detection (CAD) algorithms for Pulmonary Embolism (PE) algorithms have been shown to increase radiologists' sensitivity with a small increase in specificity. However, CAD for PE has not been adopted into clinical practice, likely because of the high number of false positives current CAD software produces. Objective: To generate a database of annotated computed tomography pulmonary angiographies, use it to compare the sensitivity and false positive rate of current algorithms and to develop new methods that improve such metrics. Methods: 91 Computed tomography pulmonary angiography scans were annotated by at least one radiologist by segmenting all pulmonary emboli visible on the study. 20 annotated CTPAs were open to the public in the form of a medical image analysis challenge. 20 more were kept for evaluation purposes. 51 were made available post-challenge. 8 submissions, 6 of them novel, were evaluated on the 20 evaluation CTPAs. Performance was measured as per embolus sensitivity vs. false positives per scan curve. Results: The best algorithms achieved a per-embolus sensitivity of 75% at 2 false positives per scan (fps) or of 70% at 1 fps, outperforming the state of the art. Deep learning approaches outperformed traditional machine learning ones, and their performance improved with the number of training cases. Significance: Through this work and challenge we have improved the state-of-the art of computer aided detection algorithms for pulmonary embolism. An open database and an evaluation benchmark for such algorithms have been generated, easing the development of further improvements. Implications on clinical practice will need further research.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge