Jiyue Xie
Establishing Rigorous and Cost-effective Clinical Trials for Artificial Intelligence Models
Jul 11, 2024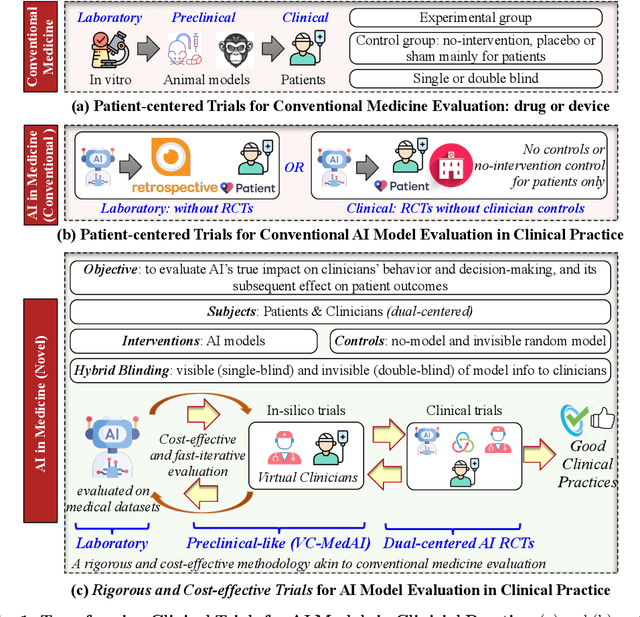
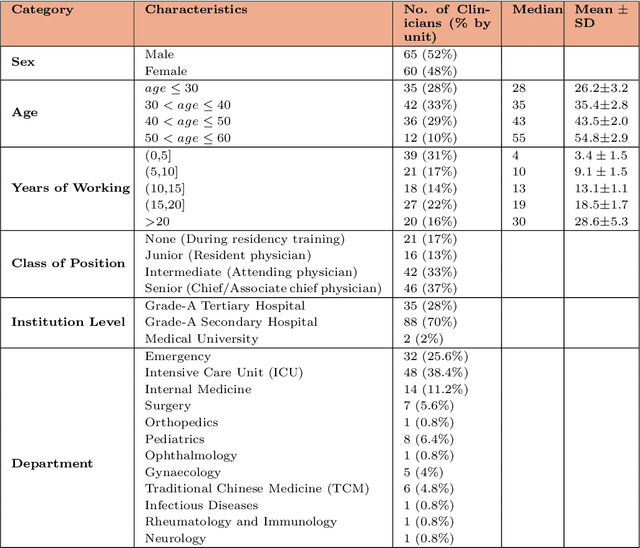
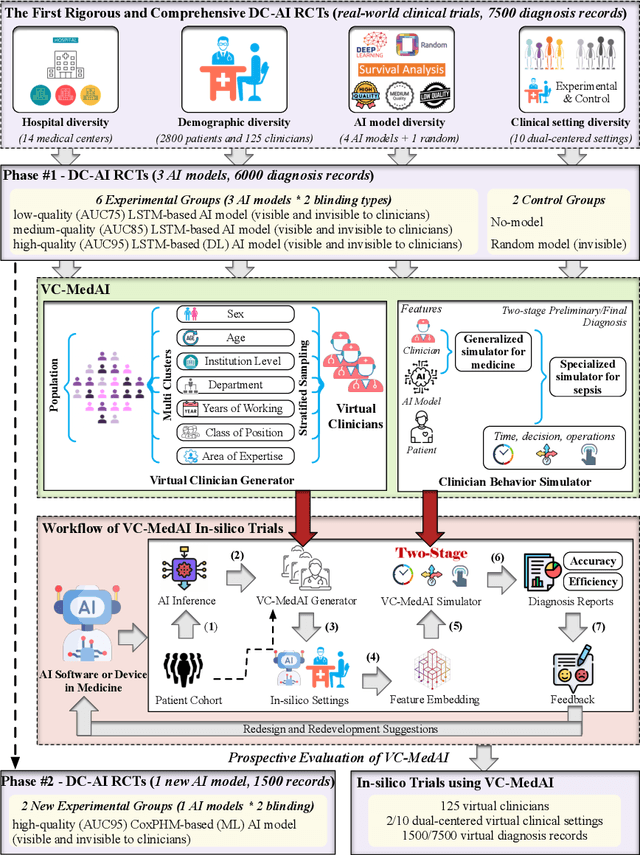
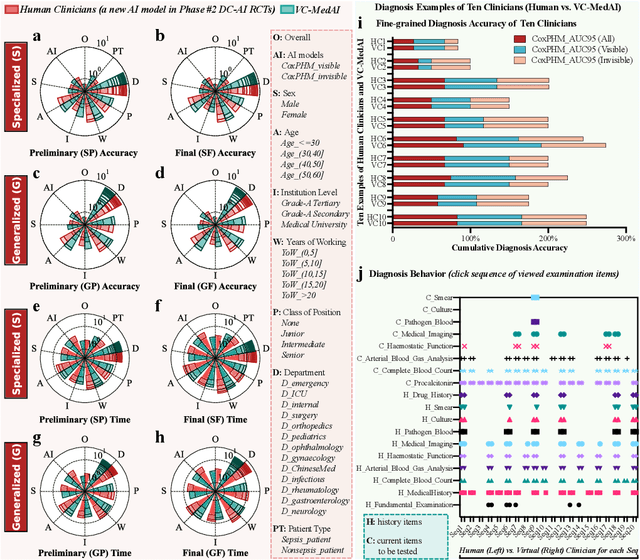
Abstract:A profound gap persists between artificial intelligence (AI) and clinical practice in medicine, primarily due to the lack of rigorous and cost-effective evaluation methodologies. State-of-the-art and state-of-the-practice AI model evaluations are limited to laboratory studies on medical datasets or direct clinical trials with no or solely patient-centered controls. Moreover, the crucial role of clinicians in collaborating with AI, pivotal for determining its impact on clinical practice, is often overlooked. For the first time, we emphasize the critical necessity for rigorous and cost-effective evaluation methodologies for AI models in clinical practice, featuring patient/clinician-centered (dual-centered) AI randomized controlled trials (DC-AI RCTs) and virtual clinician-based in-silico trials (VC-MedAI) as an effective proxy for DC-AI RCTs. Leveraging 7500 diagnosis records from two-phase inaugural DC-AI RCTs across 14 medical centers with 125 clinicians, our results demonstrate the necessity of DC-AI RCTs and the effectiveness of VC-MedAI. Notably, VC-MedAI performs comparably to human clinicians, replicating insights and conclusions from prospective DC-AI RCTs. We envision DC-AI RCTs and VC-MedAI as pivotal advancements, presenting innovative and transformative evaluation methodologies for AI models in clinical practice, offering a preclinical-like setting mirroring conventional medicine, and reshaping development paradigms in a cost-effective and fast-iterative manner. Chinese Clinical Trial Registration: ChiCTR2400086816.
OpenAPMax: Abnormal Patterns-based Model for Real-World Alzheimer's Disease Diagnosis
Jul 03, 2023



Abstract:Alzheimer's disease (AD) cannot be reversed, but early diagnosis will significantly benefit patients' medical treatment and care. In recent works, AD diagnosis has the primary assumption that all categories are known a prior -- a closed-set classification problem, which contrasts with the open-set recognition problem. This assumption hinders the application of the model in natural clinical settings. Although many open-set recognition technologies have been proposed in other fields, they are challenging to use for AD diagnosis directly since 1) AD is a degenerative disease of the nervous system with similar symptoms at each stage, and it is difficult to distinguish from its pre-state, and 2) diversified strategies for AD diagnosis are challenging to model uniformly. In this work, inspired by the concerns of clinicians during diagnosis, we propose an open-set recognition model, OpenAPMax, based on the anomaly pattern to address AD diagnosis in real-world settings. OpenAPMax first obtains the abnormal pattern of each patient relative to each known category through statistics or a literature search, clusters the patients' abnormal pattern, and finally, uses extreme value theory (EVT) to model the distance between each patient's abnormal pattern and the center of their category and modify the classification probability. We evaluate the performance of the proposed method with recent open-set recognition, where we obtain state-of-the-art results.
OpenClinicalAI: An Open and Dynamic Model for Alzheimer's Disease Diagnosis
Jul 03, 2023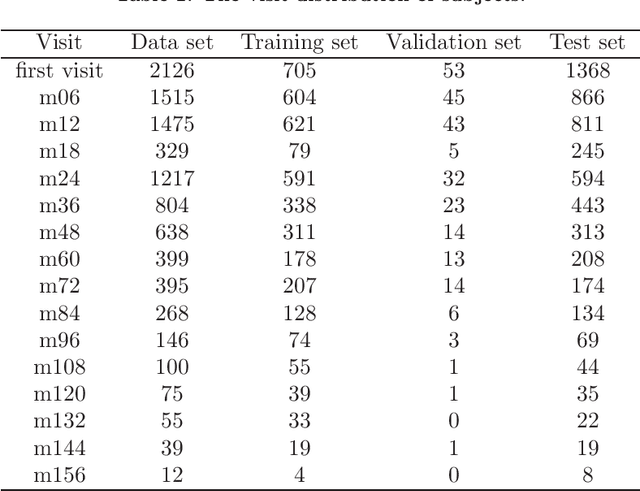
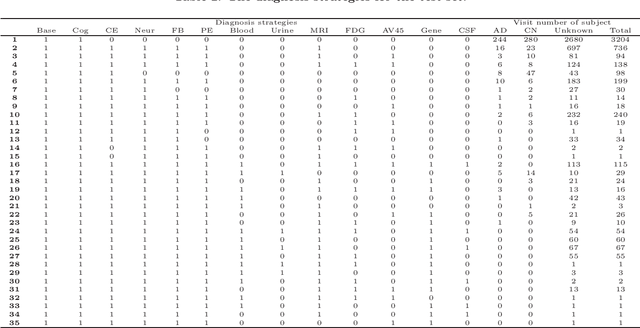
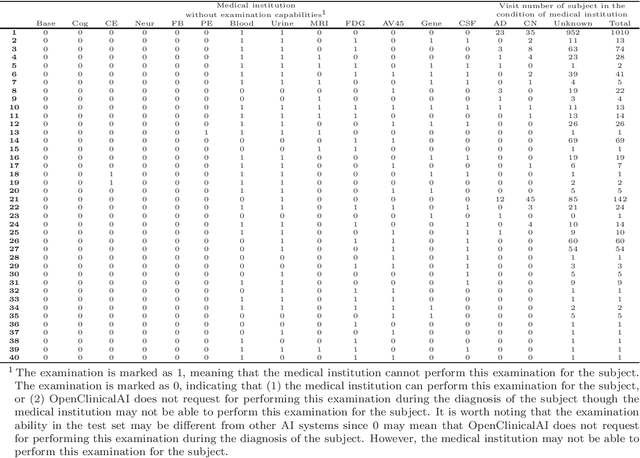
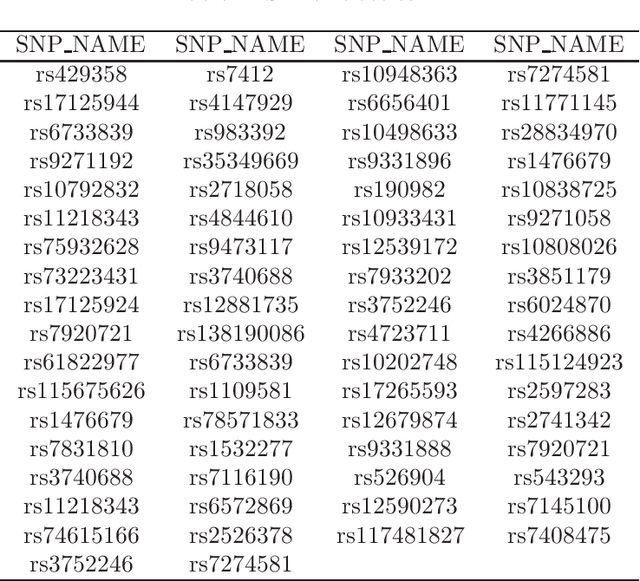
Abstract:Although Alzheimer's disease (AD) cannot be reversed or cured, timely diagnosis can significantly reduce the burden of treatment and care. Current research on AD diagnosis models usually regards the diagnosis task as a typical classification task with two primary assumptions: 1) All target categories are known a priori; 2) The diagnostic strategy for each patient is consistent, that is, the number and type of model input data for each patient are the same. However, real-world clinical settings are open, with complexity and uncertainty in terms of both subjects and the resources of the medical institutions. This means that diagnostic models may encounter unseen disease categories and need to dynamically develop diagnostic strategies based on the subject's specific circumstances and available medical resources. Thus, the AD diagnosis task is tangled and coupled with the diagnosis strategy formulation. To promote the application of diagnostic systems in real-world clinical settings, we propose OpenClinicalAI for direct AD diagnosis in complex and uncertain clinical settings. This is the first powerful end-to-end model to dynamically formulate diagnostic strategies and provide diagnostic results based on the subject's conditions and available medical resources. OpenClinicalAI combines reciprocally coupled deep multiaction reinforcement learning (DMARL) for diagnostic strategy formulation and multicenter meta-learning (MCML) for open-set recognition. The experimental results show that OpenClinicalAI achieves better performance and fewer clinical examinations than the state-of-the-art model. Our method provides an opportunity to embed the AD diagnostic system into the current health care system to cooperate with clinicians to improve current health care.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge