Dong Joo Rhee
Automated WBRT Treatment Planning via Deep Learning Auto-Contouring and Customizable Landmark-Based Field Aperture Design
May 24, 2022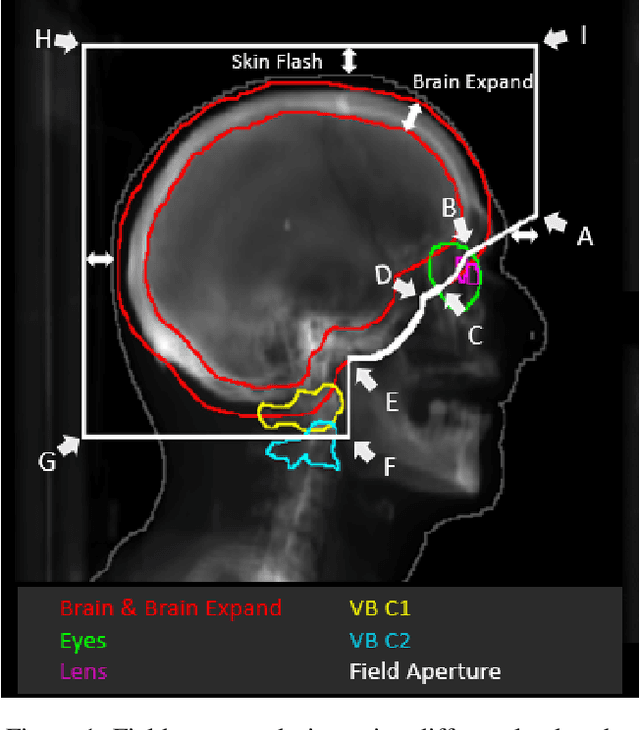


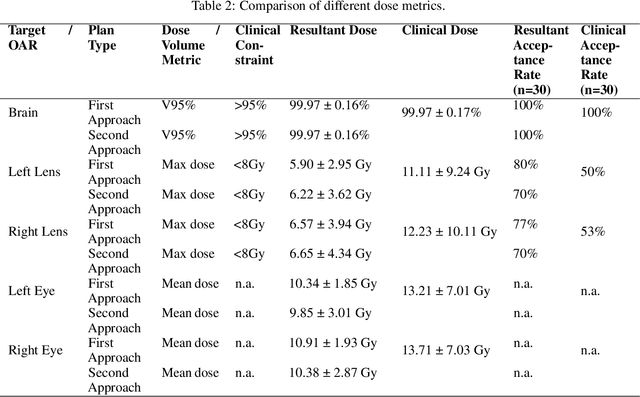
Abstract:In this work, we developed and evaluated a novel pipeline consisting of two landmark-based field aperture generation approaches for WBRT treatment planning; they are fully automated and customizable. The automation pipeline is beneficial for both clinicians and patients, where we can reduce clinician workload and reduce treatment planning time. The customizability of the field aperture design addresses different clinical requirements and allows the personalized design to become feasible. The performance results regarding quantitative and qualitative evaluations demonstrated that our plans were comparable with the original clinical plans. This technique has been deployed as part of a fully automated treatment planning tool for whole-brain cancer and could be translated to other treatment sites in the future.
Automation of Radiation Treatment Planning for Rectal Cancer
Apr 26, 2022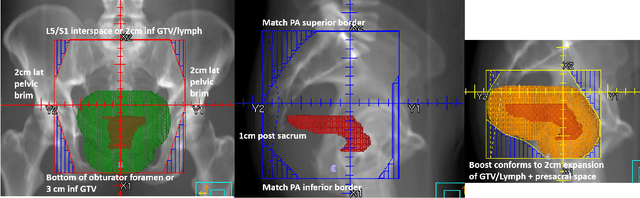
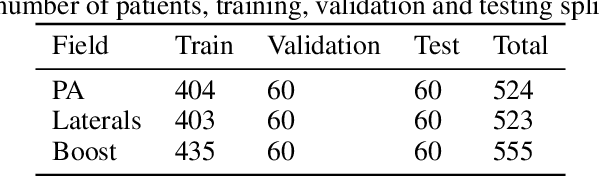
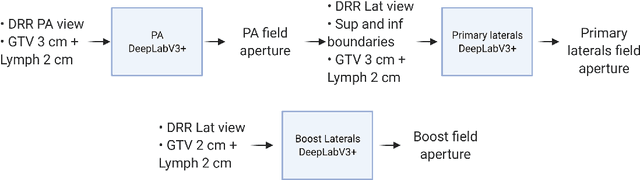
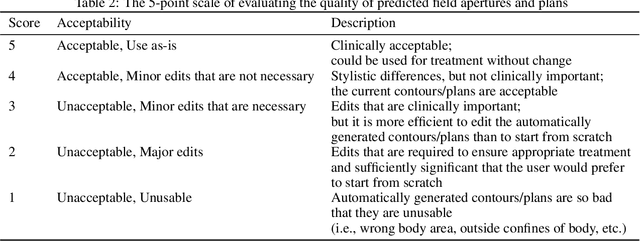
Abstract:To develop an automated workflow for rectal cancer three-dimensional conformal radiotherapy treatment planning that combines deep-learning(DL) aperture predictions and forward-planning algorithms. We designed an algorithm to automate the clinical workflow for planning with field-in-field. DL models were trained, validated, and tested on 555 patients to automatically generate aperture shapes for primary and boost fields. Network inputs were digitally reconstructed radiography, gross tumor volume(GTV), and nodal GTV. A physician scored each aperture for 20 patients on a 5-point scale(>3 acceptable). A planning algorithm was then developed to create a homogeneous dose using a combination of wedges and subfields. The algorithm iteratively identifies a hotspot volume, creates a subfield, and optimizes beam weight all without user intervention. The algorithm was tested on 20 patients using clinical apertures with different settings, and the resulting plans(4 plans/patient) were scored by a physician. The end-to-end workflow was tested and scored by a physician on 39 patients using DL-generated apertures and planning algorithms. The predicted apertures had Dice scores of 0.95, 0.94, and 0.90 for posterior-anterior, laterals, and boost fields, respectively. 100%, 95%, and 87.5% of the posterior-anterior, laterals, and boost apertures were scored as clinically acceptable, respectively. Wedged and non-wedged plans were clinically acceptable for 85% and 50% of patients, respectively. The final plans hotspot dose percentage was reduced from 121%($\pm$ 14%) to 109%($\pm$ 5%) of prescription dose. The integrated end-to-end workflow of automatically generated apertures and optimized field-in-field planning gave clinically acceptable plans for 38/39(97%) of patients. We have successfully automated the clinical workflow for generating radiotherapy plans for rectal cancer for our institution.
OpenKBP-Opt: An international and reproducible evaluation of 76 knowledge-based planning pipelines
Feb 16, 2022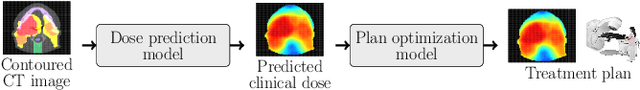
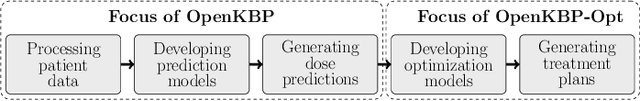
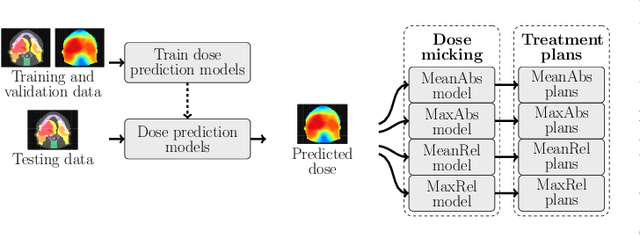
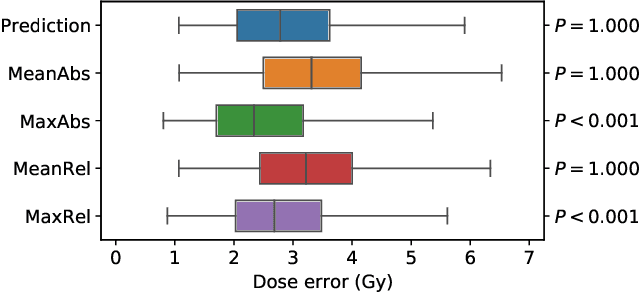
Abstract:We establish an open framework for developing plan optimization models for knowledge-based planning (KBP) in radiotherapy. Our framework includes reference plans for 100 patients with head-and-neck cancer and high-quality dose predictions from 19 KBP models that were developed by different research groups during the OpenKBP Grand Challenge. The dose predictions were input to four optimization models to form 76 unique KBP pipelines that generated 7600 plans. The predictions and plans were compared to the reference plans via: dose score, which is the average mean absolute voxel-by-voxel difference in dose a model achieved; the deviation in dose-volume histogram (DVH) criterion; and the frequency of clinical planning criteria satisfaction. We also performed a theoretical investigation to justify our dose mimicking models. The range in rank order correlation of the dose score between predictions and their KBP pipelines was 0.50 to 0.62, which indicates that the quality of the predictions is generally positively correlated with the quality of the plans. Additionally, compared to the input predictions, the KBP-generated plans performed significantly better (P<0.05; one-sided Wilcoxon test) on 18 of 23 DVH criteria. Similarly, each optimization model generated plans that satisfied a higher percentage of criteria than the reference plans. Lastly, our theoretical investigation demonstrated that the dose mimicking models generated plans that are also optimal for a conventional planning model. This was the largest international effort to date for evaluating the combination of KBP prediction and optimization models. In the interest of reproducibility, our data and code is freely available at https://github.com/ababier/open-kbp-opt.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge