Deborah Blacker
Massachusetts General Hospital, Boston, MA
An Agentic AI Workflow for Detecting Cognitive Concerns in Real-world Data
Feb 03, 2025Abstract:Early identification of cognitive concerns is critical but often hindered by subtle symptom presentation. This study developed and validated a fully automated, multi-agent AI workflow using LLaMA 3 8B to identify cognitive concerns in 3,338 clinical notes from Mass General Brigham. The agentic workflow, leveraging task-specific agents that dynamically collaborate to extract meaningful insights from clinical notes, was compared to an expert-driven benchmark. Both workflows achieved high classification performance, with F1-scores of 0.90 and 0.91, respectively. The agentic workflow demonstrated improved specificity (1.00) and achieved prompt refinement in fewer iterations. Although both workflows showed reduced performance on validation data, the agentic workflow maintained perfect specificity. These findings highlight the potential of fully automated multi-agent AI workflows to achieve expert-level accuracy with greater efficiency, offering a scalable and cost-effective solution for detecting cognitive concerns in clinical settings.
Using Deep Learning to Identify Patients with Cognitive Impairment in Electronic Health Records
Nov 13, 2021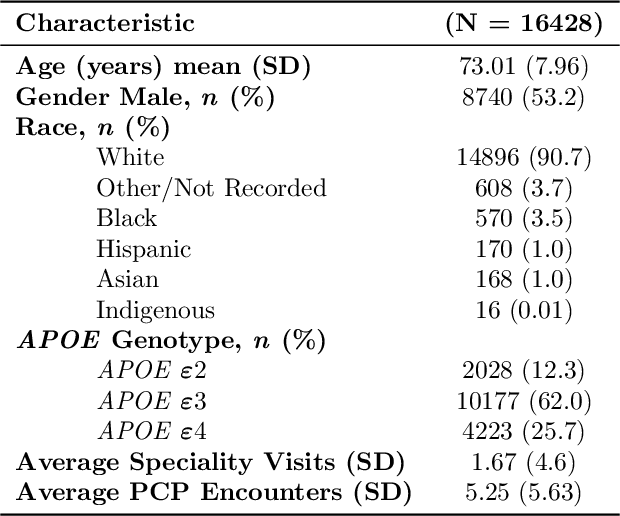
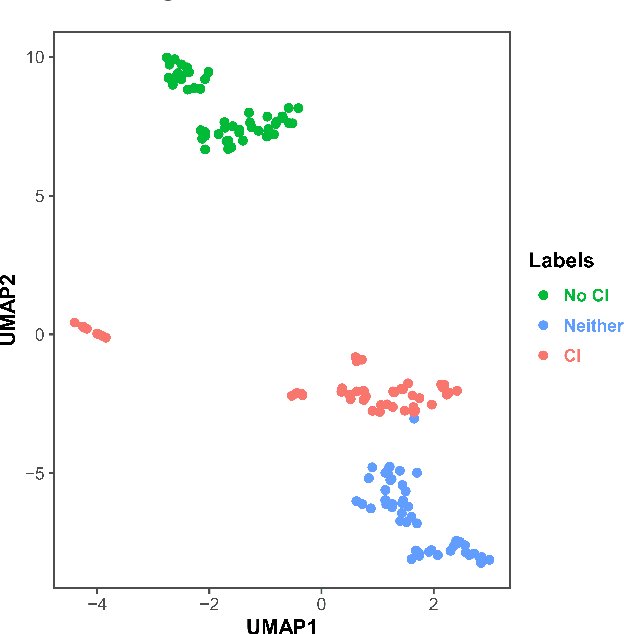
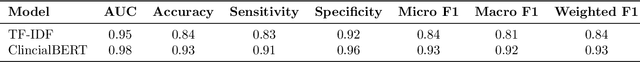
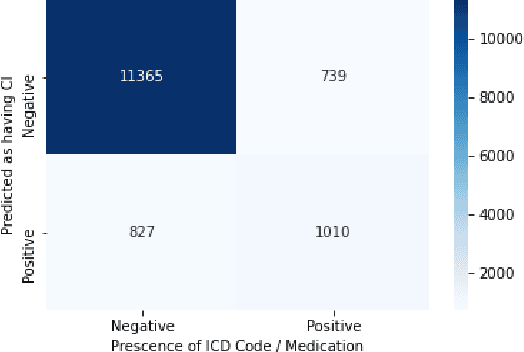
Abstract:Dementia is a neurodegenerative disorder that causes cognitive decline and affects more than 50 million people worldwide. Dementia is under-diagnosed by healthcare professionals - only one in four people who suffer from dementia are diagnosed. Even when a diagnosis is made, it may not be entered as a structured International Classification of Diseases (ICD) diagnosis code in a patient's charts. Information relevant to cognitive impairment (CI) is often found within electronic health records (EHR), but manual review of clinician notes by experts is both time consuming and often prone to errors. Automated mining of these notes presents an opportunity to label patients with cognitive impairment in EHR data. We developed natural language processing (NLP) tools to identify patients with cognitive impairment and demonstrate that linguistic context enhances performance for the cognitive impairment classification task. We fine-tuned our attention based deep learning model, which can learn from complex language structures, and substantially improved accuracy (0.93) relative to a baseline NLP model (0.84). Further, we show that deep learning NLP can successfully identify dementia patients without dementia-related ICD codes or medications.
Natural Language Processing to Detect Cognitive Concerns in Electronic Health Records Using Deep Learning
Nov 12, 2020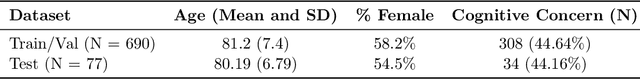
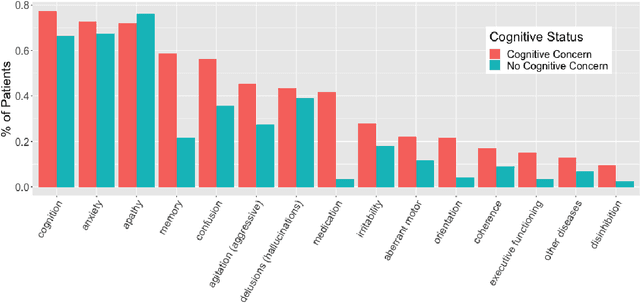
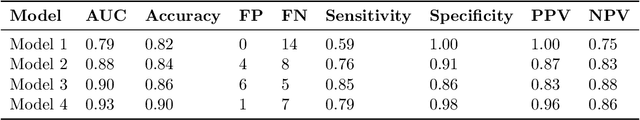
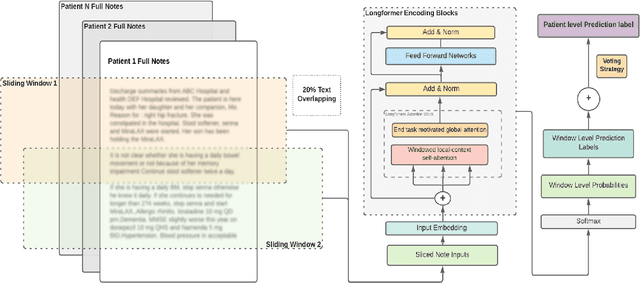
Abstract:Dementia is under-recognized in the community, under-diagnosed by healthcare professionals, and under-coded in claims data. Information on cognitive dysfunction, however, is often found in unstructured clinician notes within medical records but manual review by experts is time consuming and often prone to errors. Automated mining of these notes presents a potential opportunity to label patients with cognitive concerns who could benefit from an evaluation or be referred to specialist care. In order to identify patients with cognitive concerns in electronic medical records, we applied natural language processing (NLP) algorithms and compared model performance to a baseline model that used structured diagnosis codes and medication data only. An attention-based deep learning model outperformed the baseline model and other simpler models.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge