Benjamin Ondruschka
A Mobile Robotic Approach to Autonomous Surface Scanning in Legal Medicine
Feb 20, 2025Abstract:Purpose: Comprehensive legal medicine documentation includes both an internal but also an external examination of the corpse. Typically, this documentation is conducted manually during conventional autopsy. A systematic digital documentation would be desirable, especially for the external examination of wounds, which is becoming more relevant for legal medicine analysis. For this purpose, RGB surface scanning has been introduced. While a manual full surface scan using a handheld camera is timeconsuming and operator dependent, floor or ceiling mounted robotic systems require substantial space and a dedicated room. Hence, we consider whether a mobile robotic system can be used for external documentation. Methods: We develop a mobile robotic system that enables full-body RGB-D surface scanning. Our work includes a detailed configuration space analysis to identify the environmental parameters that need to be considered to successfully perform a surface scan. We validate our findings through an experimental study in the lab and demonstrate the system's application in a legal medicine environment. Results: Our configuration space analysis shows that a good trade-off between coverage and time is reached with three robot base positions, leading to a coverage of 94.96 %. Experiments validate the effectiveness of the system in accurately capturing body surface geometry with an average surface coverage of 96.90 +- 3.16 % and 92.45 +- 1.43 % for a body phantom and actual corpses, respectively. Conclusion: This work demonstrates the potential of a mobile robotic system to automate RGB-D surface scanning in legal medicine, complementing the use of post-mortem CT scans for inner documentation. Our results indicate that the proposed system can contribute to more efficient and autonomous legal medicine documentation, reducing the need for manual intervention.
Collaborative Robotic Biopsy with Trajectory Guidance and Needle Tip Force Feedback
Jun 12, 2023Abstract:The diagnostic value of biopsies is highly dependent on the placement of needles. Robotic trajectory guidance has been shown to improve needle positioning, but feedback for real-time navigation is limited. Haptic display of needle tip forces can provide rich feedback for needle navigation by enabling localization of tissue structures along the insertion path. We present a collaborative robotic biopsy system that combines trajectory guidance with kinesthetic feedback to assist the physician in needle placement. The robot aligns the needle while the insertion is performed in collaboration with a medical expert who controls the needle position on site. We present a needle design that senses forces at the needle tip based on optical coherence tomography and machine learning for real-time data processing. Our robotic setup allows operators to sense deep tissue interfaces independent of frictional forces to improve needle placement relative to a desired target structure. We first evaluate needle tip force sensing in ex-vivo tissue in a phantom study. We characterize the tip forces during insertions with constant velocity and demonstrate the ability to detect tissue interfaces in a collaborative user study. Participants are able to detect 91% of ex-vivo tissue interfaces based on needle tip force feedback alone. Finally, we demonstrate that even smaller, deep target structures can be accurately sampled by performing post-mortem in situ biopsies of the pancreas.
Robotic Tissue Sampling for Safe Post-mortem Biopsy in Infectious Corpses
Jan 28, 2022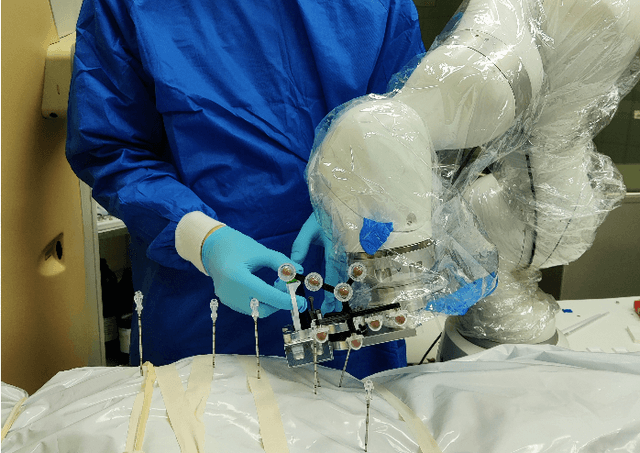
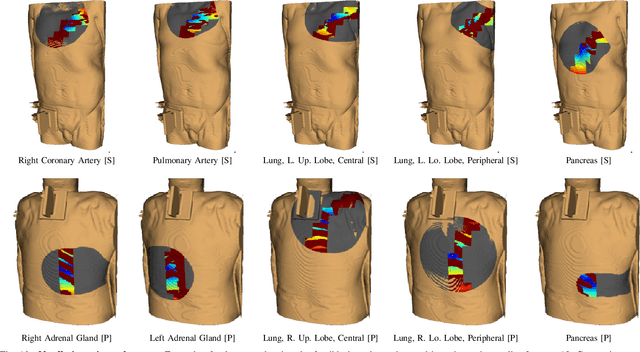
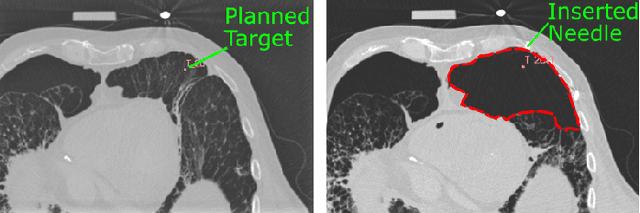
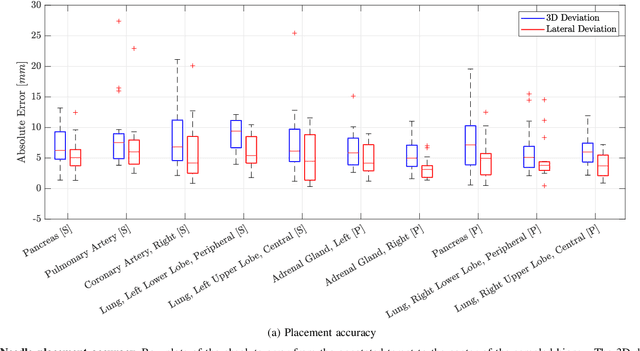
Abstract:In pathology and legal medicine, the histopathological and microbiological analysis of tissue samples from infected deceased is a valuable information for developing treatment strategies during a pandemic such as COVID-19. However, a conventional autopsy carries the risk of disease transmission and may be rejected by relatives. We propose minimally invasive biopsy with robot assistance under CT guidance to minimize the risk of disease transmission during tissue sampling and to improve accuracy. A flexible robotic system for biopsy sampling is presented, which is applied to human corpses placed inside protective body bags. An automatic planning and decision system estimates optimal insertion point. Heat maps projected onto the segmented skin visualize the distance and angle of insertions and estimate the minimum cost of a puncture while avoiding bone collisions. Further, we test multiple insertion paths concerning feasibility and collisions. A custom end effector is designed for inserting needles and extracting tissue samples under robotic guidance. Our robotic post-mortem biopsy (RPMB) system is evaluated in a study during the COVID-19 pandemic on 20 corpses and 10 tissue targets, 5 of them being infected with SARS-CoV-2. The mean planning time including robot path planning is (5.72+-1.67) s. Mean needle placement accuracy is (7.19+-4.22) mm.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge