Barbaros Selnur Erdal
Integration and Implementation Strategies for AI Algorithm Deployment with Smart Routing Rules and Workflow Management
Nov 21, 2023

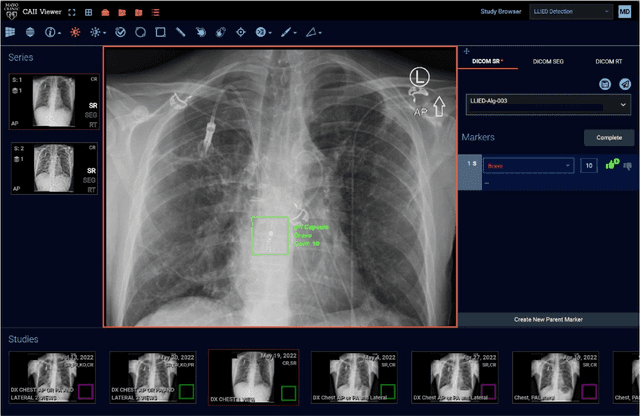

Abstract:This paper reviews the challenges hindering the widespread adoption of artificial intelligence (AI) solutions in the healthcare industry, focusing on computer vision applications for medical imaging, and how interoperability and enterprise-grade scalability can be used to address these challenges. The complex nature of healthcare workflows, intricacies in managing large and secure medical imaging data, and the absence of standardized frameworks for AI development pose significant barriers and require a new paradigm to address them. The role of interoperability is examined in this paper as a crucial factor in connecting disparate applications within healthcare workflows. Standards such as DICOM, Health Level 7 (HL7), and Integrating the Healthcare Enterprise (IHE) are highlighted as foundational for common imaging workflows. A specific focus is placed on the role of DICOM gateways, with Smart Routing Rules and Workflow Management leading transformational efforts in this area. To drive enterprise scalability, new tools are needed. Project MONAI, established in 2019, is introduced as an initiative aiming to redefine the development of medical AI applications. The MONAI Deploy App SDK, a component of Project MONAI, is identified as a key tool in simplifying the packaging and deployment process, enabling repeatable, scalable, and standardized deployment patterns for AI applications. The abstract underscores the potential impact of successful AI adoption in healthcare, offering physicians both life-saving and time-saving insights and driving efficiencies in radiology department workflows. The collaborative efforts between academia and industry, are emphasized as essential for advancing the adoption of healthcare AI solutions.
Current State of Community-Driven Radiological AI Deployment in Medical Imaging
Dec 29, 2022



Abstract:Artificial Intelligence (AI) has become commonplace to solve routine everyday tasks. Because of the exponential growth in medical imaging data volume and complexity, the workload on radiologists is steadily increasing. We project that the gap between the number of imaging exams and the number of expert radiologist readers required to cover this increase will continue to expand, consequently introducing a demand for AI-based tools that improve the efficiency with which radiologists can comfortably interpret these exams. AI has been shown to improve efficiency in medical-image generation, processing, and interpretation, and a variety of such AI models have been developed across research labs worldwide. However, very few of these, if any, find their way into routine clinical use, a discrepancy that reflects the divide between AI research and successful AI translation. To address the barrier to clinical deployment, we have formed MONAI Consortium, an open-source community which is building standards for AI deployment in healthcare institutions, and developing tools and infrastructure to facilitate their implementation. This report represents several years of weekly discussions and hands-on problem solving experience by groups of industry experts and clinicians in the MONAI Consortium. We identify barriers between AI-model development in research labs and subsequent clinical deployment and propose solutions. Our report provides guidance on processes which take an imaging AI model from development to clinical implementation in a healthcare institution. We discuss various AI integration points in a clinical Radiology workflow. We also present a taxonomy of Radiology AI use-cases. Through this report, we intend to educate the stakeholders in healthcare and AI (AI researchers, radiologists, imaging informaticists, and regulators) about cross-disciplinary challenges and possible solutions.
A multi-reconstruction study of breast density estimation using Deep Learning
Feb 17, 2022



Abstract:Breast density estimation is one of the key tasks in recognizing individuals predisposed to breast cancer. It is often challenging because of low contrast and fluctuations in mammograms' fatty tissue background. Most of the time, the breast density is estimated manually where a radiologist assigns one of the four density categories decided by the Breast Imaging and Reporting Data Systems (BI-RADS). There have been efforts in the direction of automating a breast density classification pipeline. Breast density estimation is one of the key tasks performed during a screening exam. Dense breasts are more susceptible to breast cancer. The density estimation is challenging because of low contrast and fluctuations in mammograms' fatty tissue background. Traditional mammograms are being replaced by tomosynthesis and its other low radiation dose variants (for example Hologic' Intelligent 2D and C-View). Because of the low-dose requirement, increasingly more screening centers are favoring the Intelligent 2D view and C-View. Deep-learning studies for breast density estimation use only a single modality for training a neural network. However, doing so restricts the number of images in the dataset. In this paper, we show that a neural network trained on all the modalities at once performs better than a neural network trained on any single modality. We discuss these results using the area under the receiver operator characteristics curves.
Deep Learning-Based Automatic Detection of Poorly Positioned Mammograms to Minimize Patient Return Visits for Repeat Imaging: A Real-World Application
Sep 28, 2020



Abstract:Screening mammograms are a routine imaging exam performed to detect breast cancer in its early stages to reduce morbidity and mortality attributed to this disease. In order to maximize the efficacy of breast cancer screening programs, proper mammographic positioning is paramount. Proper positioning ensures adequate visualization of breast tissue and is necessary for effective breast cancer detection. Therefore, breast-imaging radiologists must assess each mammogram for the adequacy of positioning before providing a final interpretation of the examination; this often necessitates return patient visits for additional imaging. In this paper, we propose a deep learning-algorithm method that mimics and automates this decision-making process to identify poorly positioned mammograms. Our objective for this algorithm is to assist mammography technologists in recognizing inadequately positioned mammograms real-time, improve the quality of mammographic positioning and performance, and ultimately reducing repeat visits for patients with initially inadequate imaging. The proposed model showed a true positive rate for detecting correct positioning of 91.35% in the mediolateral oblique view and 95.11% in the craniocaudal view. In addition to these results, we also present an automatically generated report which can aid the mammography technologist in taking corrective measures during the patient visit.
Democratizing Artificial Intelligence in Healthcare: A Study of Model Development Across Two Institutions Incorporating Transfer Learning
Sep 25, 2020



Abstract:The training of deep learning models typically requires extensive data, which are not readily available as large well-curated medical-image datasets for development of artificial intelligence (AI) models applied in Radiology. Recognizing the potential for transfer learning (TL) to allow a fully trained model from one institution to be fine-tuned by another institution using a much small local dataset, this report describes the challenges, methodology, and benefits of TL within the context of developing an AI model for a basic use-case, segmentation of Left Ventricular Myocardium (LVM) on images from 4-dimensional coronary computed tomography angiography. Ultimately, our results from comparisons of LVM segmentation predicted by a model locally trained using random initialization, versus one training-enhanced by TL, showed that a use-case model initiated by TL can be developed with sparse labels with acceptable performance. This process reduces the time required to build a new model in the clinical environment at a different institution.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge