Survival modeling using deep learning, machine learning and statistical methods: A comparative analysis for predicting mortality after hospital admission
Paper and Code
Mar 04, 2024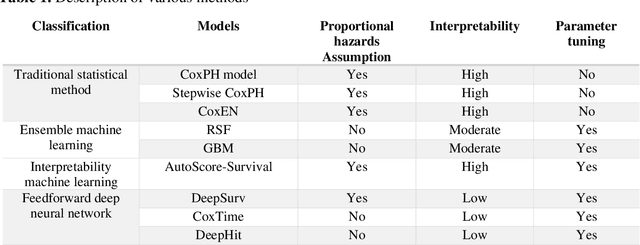
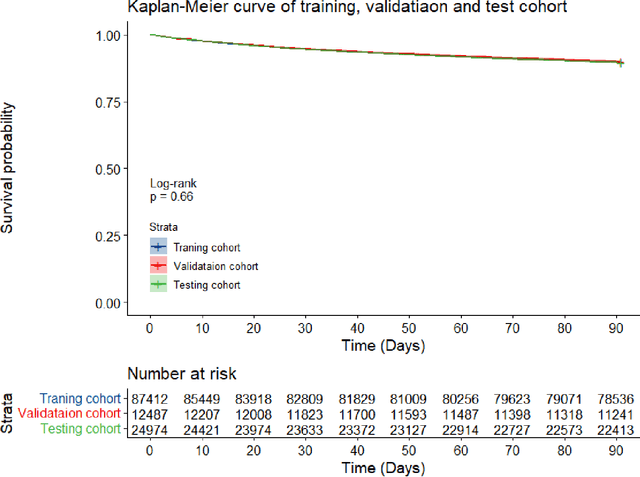
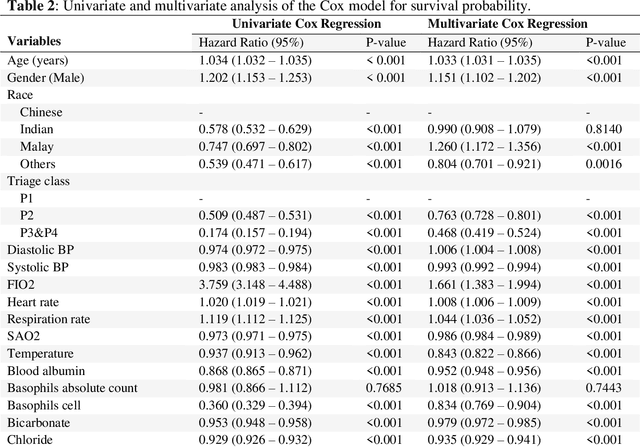
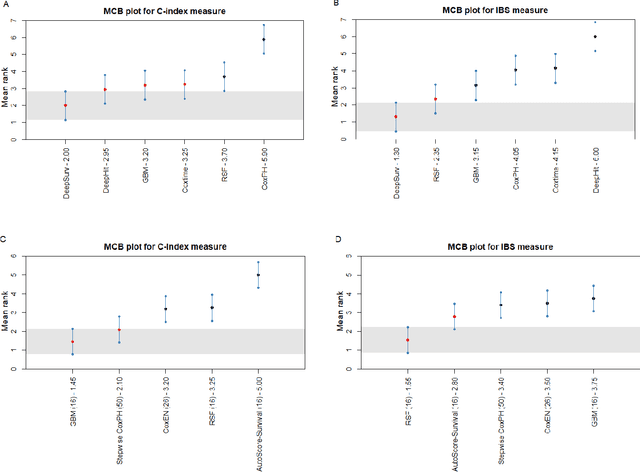
Survival analysis is essential for studying time-to-event outcomes and providing a dynamic understanding of the probability of an event occurring over time. Various survival analysis techniques, from traditional statistical models to state-of-the-art machine learning algorithms, support healthcare intervention and policy decisions. However, there remains ongoing discussion about their comparative performance. We conducted a comparative study of several survival analysis methods, including Cox proportional hazards (CoxPH), stepwise CoxPH, elastic net penalized Cox model, Random Survival Forests (RSF), Gradient Boosting machine (GBM) learning, AutoScore-Survival, DeepSurv, time-dependent Cox model based on neural network (CoxTime), and DeepHit survival neural network. We applied the concordance index (C-index) for model goodness-of-fit, and integral Brier scores (IBS) for calibration, and considered the model interpretability. As a case study, we performed a retrospective analysis of patients admitted through the emergency department of a tertiary hospital from 2017 to 2019, predicting 90-day all-cause mortality based on patient demographics, clinicopathological features, and historical data. The results of the C-index indicate that deep learning achieved comparable performance, with DeepSurv producing the best discrimination (DeepSurv: 0.893; CoxTime: 0.892; DeepHit: 0.891). The calibration of DeepSurv (IBS: 0.041) performed the best, followed by RSF (IBS: 0.042) and GBM (IBS: 0.0421), all using the full variables. Moreover, AutoScore-Survival, using a minimal variable subset, is easy to interpret, and can achieve good discrimination and calibration (C-index: 0.867; IBS: 0.044). While all models were satisfactory, DeepSurv exhibited the best discrimination and calibration. In addition, AutoScore-Survival offers a more parsimonious model and excellent interpretability.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge