Yonggang Ma
Deep-Learning Tool for Early Identifying Non-Traumatic Intracranial Hemorrhage Etiology based on CT Scan
Feb 02, 2023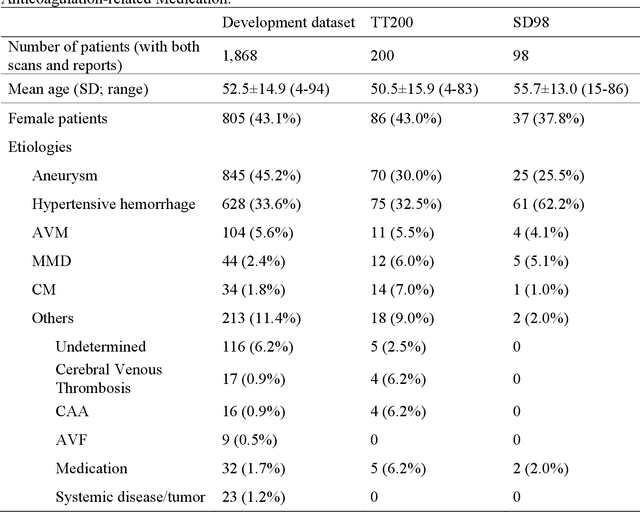
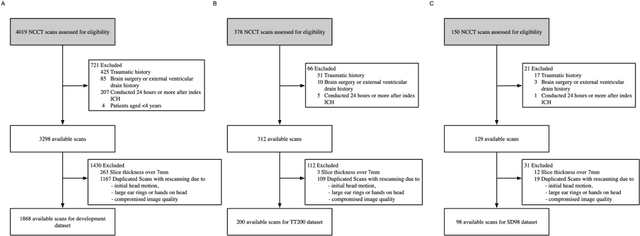

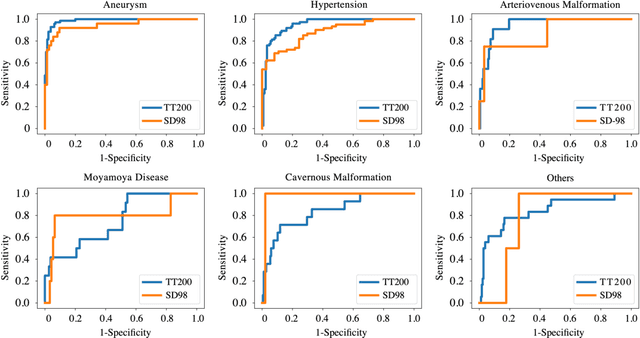
Abstract:Background: To develop an artificial intelligence system that can accurately identify acute non-traumatic intracranial hemorrhage (ICH) etiology based on non-contrast CT (NCCT) scans and investigate whether clinicians can benefit from it in a diagnostic setting. Materials and Methods: The deep learning model was developed with 1868 eligible NCCT scans with non-traumatic ICH collected between January 2011 and April 2018. We tested the model on two independent datasets (TT200 and SD 98) collected after April 2018. The model's diagnostic performance was compared with clinicians's performance. We further designed a simulated study to compare the clinicians's performance with and without the deep learning system augmentation. Results: The proposed deep learning system achieved area under the receiver operating curve of 0.986 (95% CI 0.967-1.000) on aneurysms, 0.952 (0.917-0.987) on hypertensive hemorrhage, 0.950 (0.860-1.000) on arteriovenous malformation (AVM), 0.749 (0.586-0.912) on Moyamoya disease (MMD), 0.837 (0.704-0.969) on cavernous malformation (CM), and 0.839 (0.722-0.959) on other causes in TT200 dataset. Given a 90% specificity level, the sensitivities of our model were 97.1% and 90.9% for aneurysm and AVM diagnosis, respectively. The model also shows an impressive generalizability in an independent dataset SD98. The clinicians achieve significant improvements in the sensitivity, specificity, and accuracy of diagnoses of certain hemorrhage etiologies with proposed system augmentation. Conclusions: The proposed deep learning algorithms can be an effective tool for early identification of hemorrhage etiologies based on NCCT scans. It may also provide more information for clinicians for triage and further imaging examination selection.
Deep Learning Approach to Predict Hemorrhage in Moyamoya Disease
Feb 01, 2023Abstract:Objective: Reliable tools to predict moyamoya disease (MMD) patients at risk for hemorrhage could have significant value. The aim of this paper is to develop three machine learning classification algorithms to predict hemorrhage in moyamoya disease. Methods: Clinical data of consecutive MMD patients who were admitted to our hospital between 2009 and 2015 were reviewed. Demographics, clinical, radiographic data were analyzed to develop artificial neural network (ANN), support vector machine (SVM), and random forest models. Results: We extracted 33 parameters, including 11 demographic and 22 radiographic features as input for model development. Of all compared classification results, ANN achieved the highest overall accuracy of 75.7% (95% CI, 68.6%-82.8%), followed by SVM with 69.2% (95% CI, 56.9%-81.5%) and random forest with 70.0% (95% CI, 57.0%-83.0%). Conclusions: The proposed ANN framework can be a potential effective tool to predict the possibility of hemorrhage among adult MMD patients based on clinical information and radiographic features.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge