Rafe Mcbeth
Automating High Quality RT Planning at Scale
Jan 21, 2025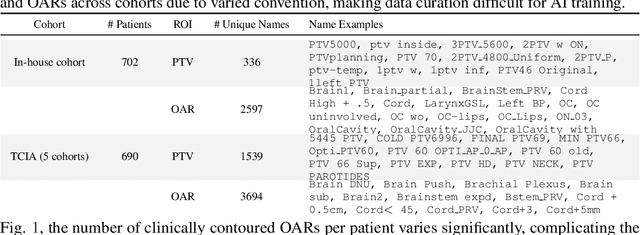
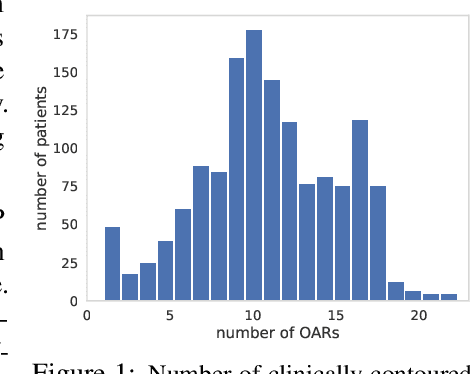
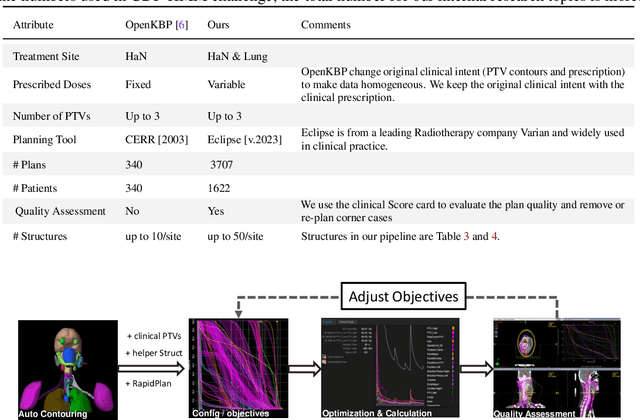
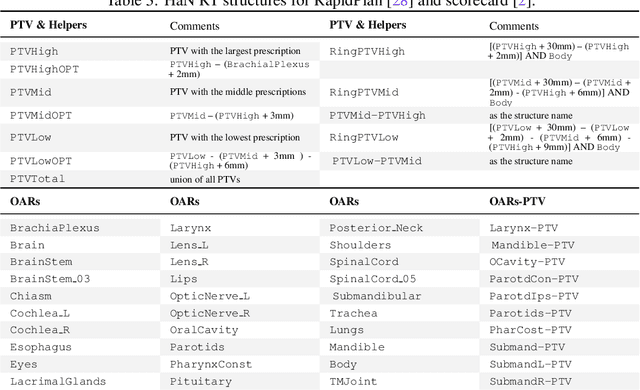
Abstract:Radiotherapy (RT) planning is complex, subjective, and time-intensive. Advances in artificial intelligence (AI) promise to improve its precision, efficiency, and consistency, but progress is often limited by the scarcity of large, standardized datasets. To address this, we introduce the Automated Iterative RT Planning (AIRTP) system, a scalable solution for generating high-quality treatment plans. This scalable solution is designed to generate substantial volumes of consistently high-quality treatment plans, overcoming a key obstacle in the advancement of AI-driven RT planning. Our AIRTP pipeline adheres to clinical guidelines and automates essential steps, including organ-at-risk (OAR) contouring, helper structure creation, beam setup, optimization, and plan quality improvement, using AI integrated with RT planning software like Eclipse of Varian. Furthermore, a novel approach for determining optimization parameters to reproduce 3D dose distributions, i.e. a method to convert dose predictions to deliverable treatment plans constrained by machine limitations. A comparative analysis of plan quality reveals that our automated pipeline produces treatment plans of quality comparable to those generated manually, which traditionally require several hours of labor per plan. Committed to public research, the first data release of our AIRTP pipeline includes nine cohorts covering head-and-neck and lung cancer sites to support an AAPM 2025 challenge. This data set features more than 10 times the number of plans compared to the largest existing well-curated public data set to our best knowledge. Repo:{https://github.com/RiqiangGao/GDP-HMM_AAPMChallenge}
Uncertainty-Error correlations in Evidential Deep Learning models for biomedical segmentation
Oct 24, 2024Abstract:In this work, we examine the effectiveness of an uncertainty quantification framework known as Evidential Deep Learning applied in the context of biomedical image segmentation. This class of models involves assigning Dirichlet distributions as priors for segmentation labels, and enables a few distinct definitions of model uncertainties. Using the cardiac and prostate MRI images available in the Medical Segmentation Decathlon for validation, we found that Evidential Deep Learning models with U-Net backbones generally yielded superior correlations between prediction errors and uncertainties relative to the conventional baseline equipped with Shannon entropy measure, Monte-Carlo Dropout and Deep Ensemble methods. We also examined these models' effectiveness in active learning, finding that relative to the standard Shannon entropy-based sampling, they yielded higher point-biserial uncertainty-error correlations while attaining similar performances in Dice-Sorensen coefficients. These superior features of EDL models render them well-suited for segmentation tasks that warrant a critical sensitivity in detecting large model errors.
Deep Evidential Learning for Dose Prediction
Apr 26, 2024Abstract:In this work, we present a novel application of an uncertainty-quantification framework called Deep Evidential Learning in the domain of radiotherapy dose prediction. Using medical images of the Open Knowledge-Based Planning Challenge dataset, we found that this model can be effectively harnessed to yield uncertainty estimates that inherited correlations with prediction errors upon completion of network training. This was achieved only after reformulating the original loss function for a stable implementation. We found that (i)epistemic uncertainty was highly correlated with prediction errors, with various association indices comparable or stronger than those for Monte-Carlo Dropout and Deep Ensemble methods, (ii)the median error varied with uncertainty threshold much more linearly for epistemic uncertainty in Deep Evidential Learning relative to these other two conventional frameworks, indicative of a more uniformly calibrated sensitivity to model errors, (iii)relative to epistemic uncertainty, aleatoric uncertainty demonstrated a more significant shift in its distribution in response to Gaussian noise added to CT intensity, compatible with its interpretation as reflecting data noise. Collectively, our results suggest that Deep Evidential Learning is a promising approach that can endow deep-learning models in radiotherapy dose prediction with statistical robustness. Towards enhancing its clinical relevance, we demonstrate how we can use such a model to construct the predicted Dose-Volume-Histograms' confidence intervals.
Exploring UMAP in hybrid models of entropy-based and representativeness sampling for active learning in biomedical segmentation
Dec 16, 2023Abstract:In this work, we study various hybrid models of entropy-based and representativeness sampling techniques in the context of active learning in medical segmentation, in particular examining the role of UMAP (Uniform Manifold Approximation and Projection) as a technique for capturing representativeness. Although UMAP has been shown viable as a general purpose dimension reduction method in diverse areas, its role in deep learning-based medical segmentation has yet been extensively explored. Using the cardiac and prostate datasets in the Medical Segmentation Decathlon for validation, we found that a novel hybrid combination of Entropy-UMAP sampling technique achieved a statistically significant Dice score advantage over the random baseline ($3.2 \%$ for cardiac, $4.5 \%$ for prostate), and attained the highest Dice coefficient among the spectrum of 10 distinct active learning methodologies we examined. This provides preliminary evidence that there is an interesting synergy between entropy-based and UMAP methods when the former precedes the latter in a hybrid model of active learning.
Swin UNETR++: Advancing Transformer-Based Dense Dose Prediction Towards Fully Automated Radiation Oncology Treatments
Nov 11, 2023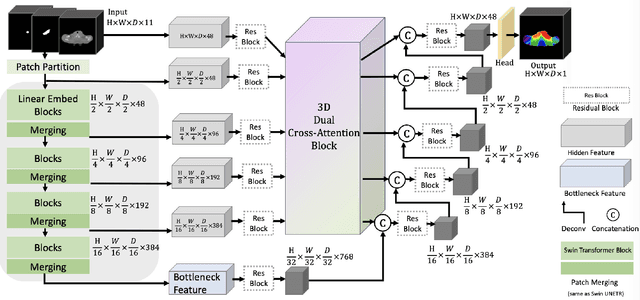
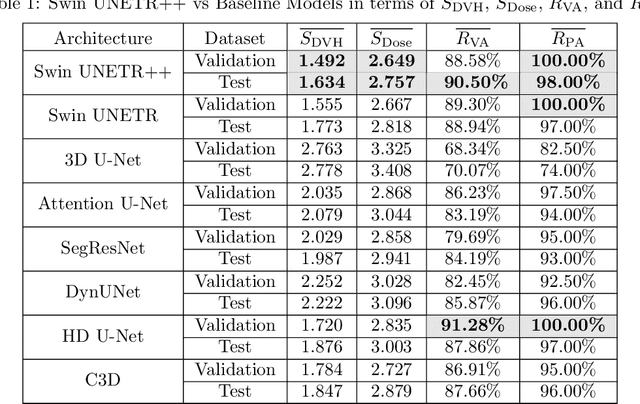
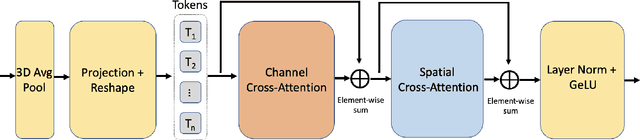
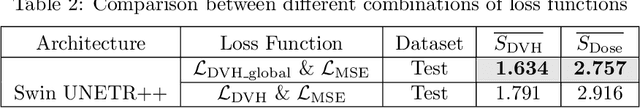
Abstract:The field of Radiation Oncology is uniquely positioned to benefit from the use of artificial intelligence to fully automate the creation of radiation treatment plans for cancer therapy. This time-consuming and specialized task combines patient imaging with organ and tumor segmentation to generate a 3D radiation dose distribution to meet clinical treatment goals, similar to voxel-level dense prediction. In this work, we propose Swin UNETR++, that contains a lightweight 3D Dual Cross-Attention (DCA) module to capture the intra and inter-volume relationships of each patient's unique anatomy, which fully convolutional neural networks lack. Our model was trained, validated, and tested on the Open Knowledge-Based Planning dataset. In addition to metrics of Dose Score $\overline{S_{\text{Dose}}}$ and DVH Score $\overline{S_{\text{DVH}}}$ that quantitatively measure the difference between the predicted and ground-truth 3D radiation dose distribution, we propose the qualitative metrics of average volume-wise acceptance rate $\overline{R_{\text{VA}}}$ and average patient-wise clinical acceptance rate $\overline{R_{\text{PA}}}$ to assess the clinical reliability of the predictions. Swin UNETR++ demonstrates near-state-of-the-art performance on validation and test dataset (validation: $\overline{S_{\text{DVH}}}$=1.492 Gy, $\overline{S_{\text{Dose}}}$=2.649 Gy, $\overline{R_{\text{VA}}}$=88.58%, $\overline{R_{\text{PA}}}$=100.0%; test: $\overline{S_{\text{DVH}}}$=1.634 Gy, $\overline{S_{\text{Dose}}}$=2.757 Gy, $\overline{R_{\text{VA}}}$=90.50%, $\overline{R_{\text{PA}}}$=98.0%), establishing a basis for future studies to translate 3D dose predictions into a deliverable treatment plan, facilitating full automation.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge