Luca Canalini
Comparison of different automatic solutions for resection cavity segmentation in postoperative MRI volumes including longitudinal acquisitions
Oct 14, 2022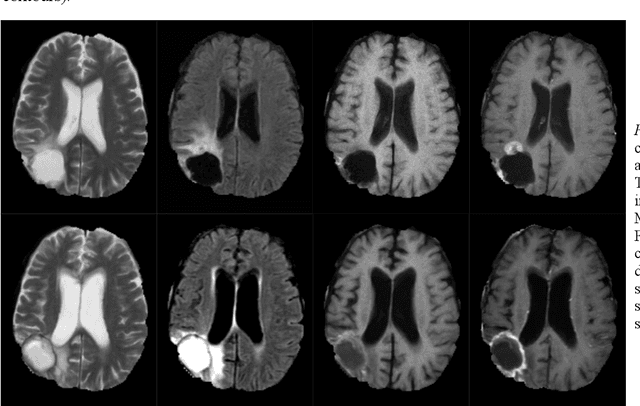
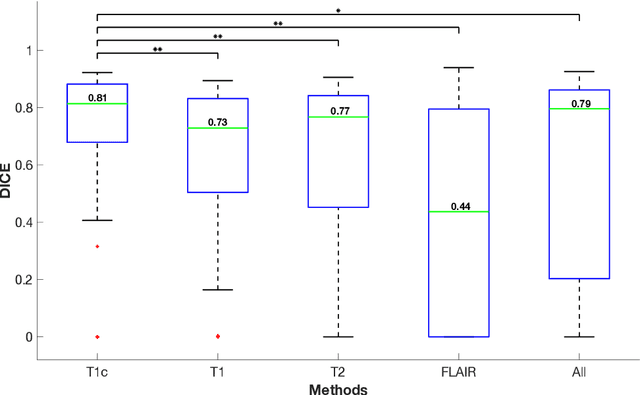

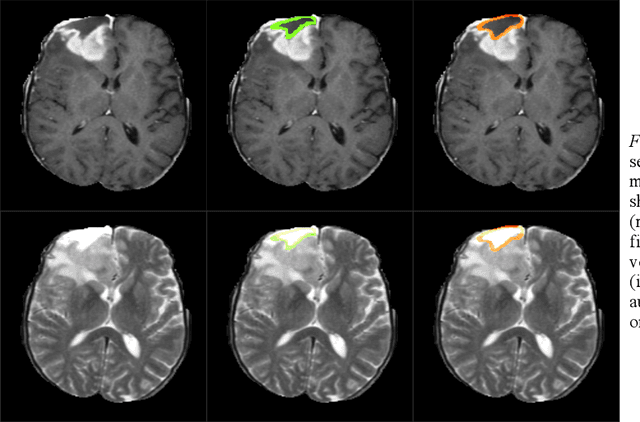
Abstract:In this work, we compare five deep learning solutions to automatically segment the resection cavity in postoperative MRI. The proposed methods are based on the same 3D U-Net architecture. We use a dataset of postoperative MRI volumes, each including four MRI sequences and the ground truth of the corresponding resection cavity. Four solutions are trained with a different MRI sequence. Besides, a method designed with all the available sequences is also presented. Our experiments show that the method trained only with the T1 weighted contrast-enhanced MRI sequence achieves the best results, with a median DICE index of 0.81.
Learn-Morph-Infer: a new way of solving the inverse problem for brain tumor modeling
Nov 07, 2021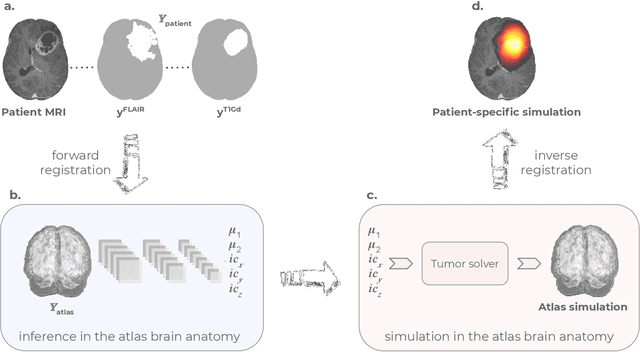
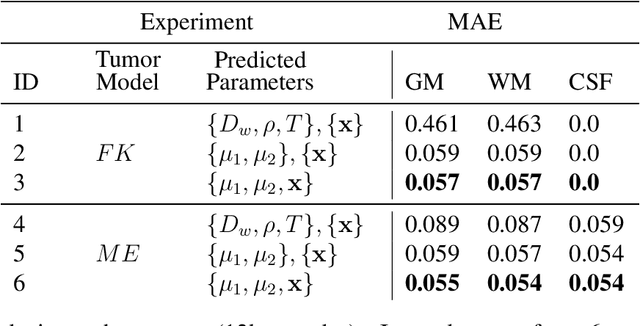
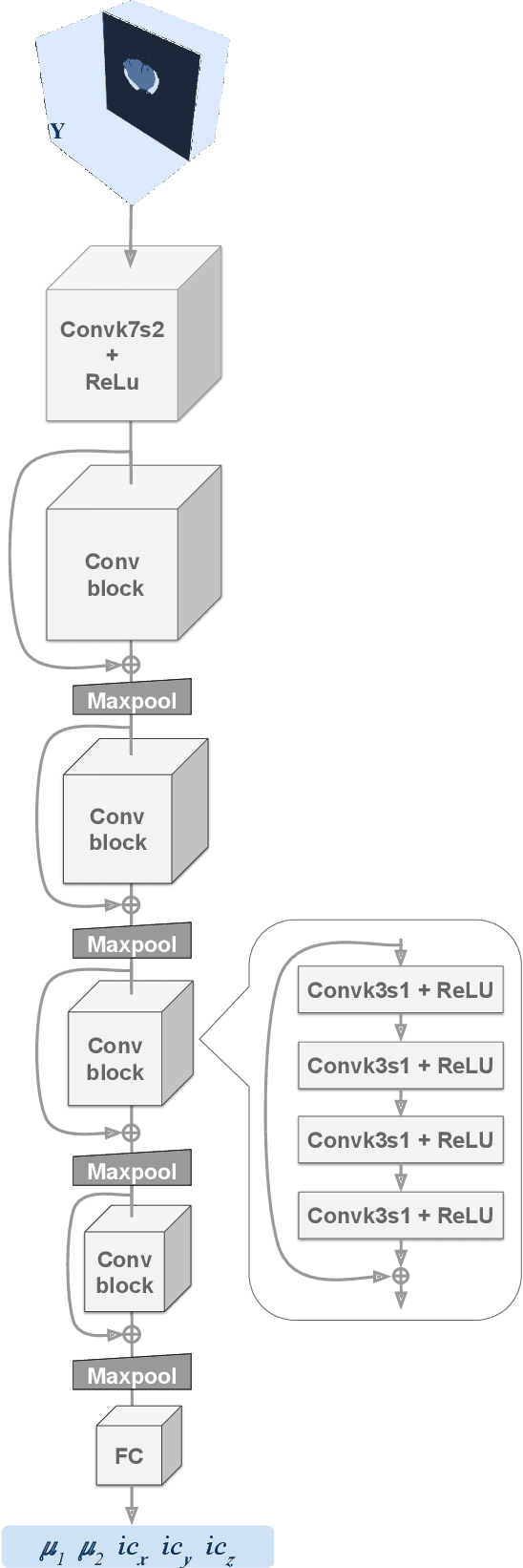
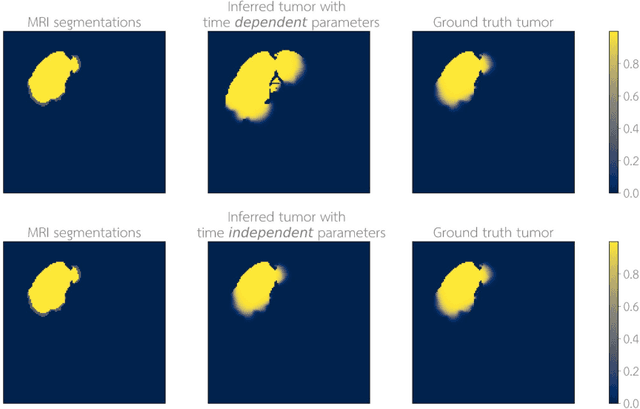
Abstract:Current treatment planning of patients diagnosed with brain tumor could significantly benefit by accessing the spatial distribution of tumor cell concentration. Existing diagnostic modalities, such as magnetic-resonance imaging (MRI), contrast sufficiently well areas of high cell density. However, they do not portray areas of low concentration, which can often serve as a source for the secondary appearance of the tumor after treatment. Numerical simulations of tumor growth could complement imaging information by providing estimates of full spatial distributions of tumor cells. Over recent years a corpus of literature on medical image-based tumor modeling was published. It includes different mathematical formalisms describing the forward tumor growth model. Alongside, various parametric inference schemes were developed to perform an efficient tumor model personalization, i.e. solving the inverse problem. However, the unifying drawback of all existing approaches is the time complexity of the model personalization that prohibits a potential integration of the modeling into clinical settings. In this work, we introduce a methodology for inferring patient-specific spatial distribution of brain tumor from T1Gd and FLAIR MRI medical scans. Coined as \textit{Learn-Morph-Infer} the method achieves real-time performance in the order of minutes on widely available hardware and the compute time is stable across tumor models of different complexity, such as reaction-diffusion and reaction-advection-diffusion models. We believe the proposed inverse solution approach not only bridges the way for clinical translation of brain tumor personalization but can also be adopted to other scientific and engineering domains.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge