Konstantia Zarkogianni
A modular framework for automated evaluation of procedural content generation in serious games with deep reinforcement learning agents
May 22, 2025Abstract:Serious Games (SGs) are nowadays shifting focus to include procedural content generation (PCG) in the development process as a means of offering personalized and enhanced player experience. However, the development of a framework to assess the impact of PCG techniques when integrated into SGs remains particularly challenging. This study proposes a methodology for automated evaluation of PCG integration in SGs, incorporating deep reinforcement learning (DRL) game testing agents. To validate the proposed framework, a previously introduced SG featuring card game mechanics and incorporating three different versions of PCG for nonplayer character (NPC) creation has been deployed. Version 1 features random NPC creation, while versions 2 and 3 utilize a genetic algorithm approach. These versions are used to test the impact of different dynamic SG environments on the proposed framework's agents. The obtained results highlight the superiority of the DRL game testing agents trained on Versions 2 and 3 over those trained on Version 1 in terms of win rate (i.e. number of wins per played games) and training time. More specifically, within the execution of a test emulating regular gameplay, both Versions 2 and 3 peaked at a 97% win rate and achieved statistically significant higher (p=0009) win rates compared to those achieved in Version 1 that peaked at 94%. Overall, results advocate towards the proposed framework's capability to produce meaningful data for the evaluation of procedurally generated content in SGs.
Sustaining model performance for covid-19 detection from dynamic audio data: Development and evaluation of a comprehensive drift-adaptive framework
Sep 28, 2024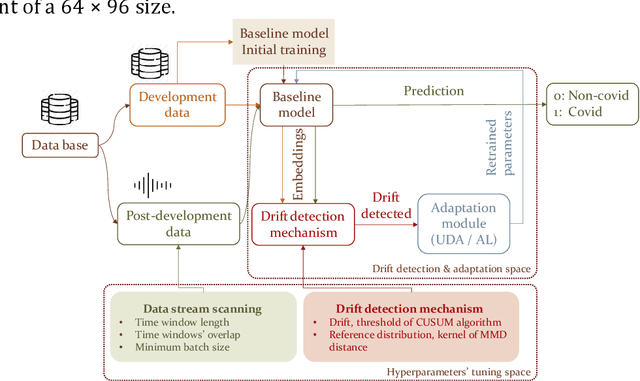
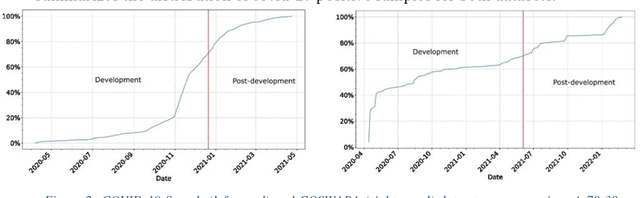
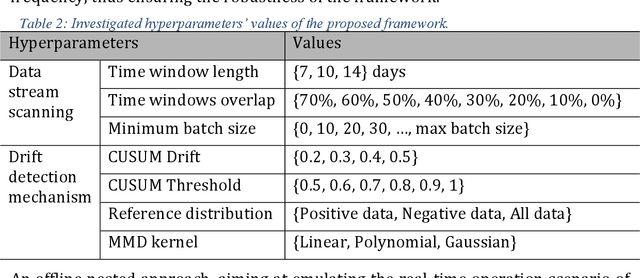
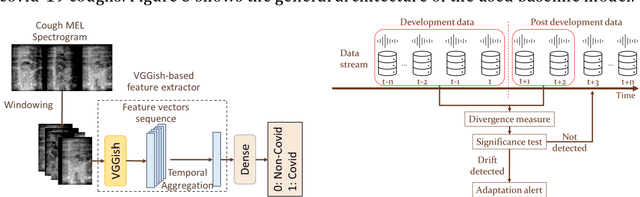
Abstract:Background: The COVID-19 pandemic has highlighted the need for robust diagnostic tools capable of detecting the disease from diverse and evolving data sources. Machine learning models, especially convolutional neural networks (CNNs), have shown promise. However, the dynamic nature of real-world data can lead to model drift, where performance degrades over time as the underlying data distribution changes. Addressing this challenge is crucial to maintaining accuracy and reliability in diagnostic applications. Objective: This study aims to develop a framework that monitors model drift and employs adaptation mechanisms to mitigate performance fluctuations in COVID-19 detection models trained on dynamic audio data. Methods: Two crowd-sourced COVID-19 audio datasets, COVID-19 Sounds and COSWARA, were used. Each was divided into development and post-development periods. A baseline CNN model was trained and evaluated using cough recordings from the development period. Maximum mean discrepancy (MMD) was used to detect changes in data distributions and model performance between periods. Upon detecting drift, retraining was triggered to update the baseline model. Two adaptation approaches were compared: unsupervised domain adaptation (UDA) and active learning (AL). Results: UDA improved balanced accuracy by up to 22% and 24% for the COVID-19 Sounds and COSWARA datasets, respectively. AL yielded even greater improvements, with increases of up to 30% and 60%, respectively. Conclusions: The proposed framework addresses model drift in COVID-19 detection, enabling continuous adaptation to evolving data. This approach ensures sustained model performance, contributing to robust diagnostic tools for COVID-19 and potentially other infectious diseases.
The smarty4covid dataset and knowledge base: a framework enabling interpretable analysis of audio signals
Jul 11, 2023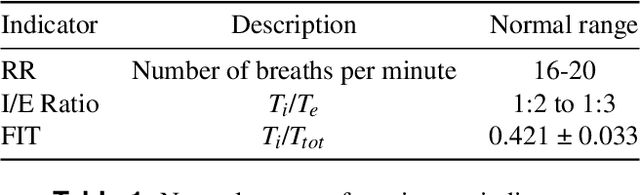
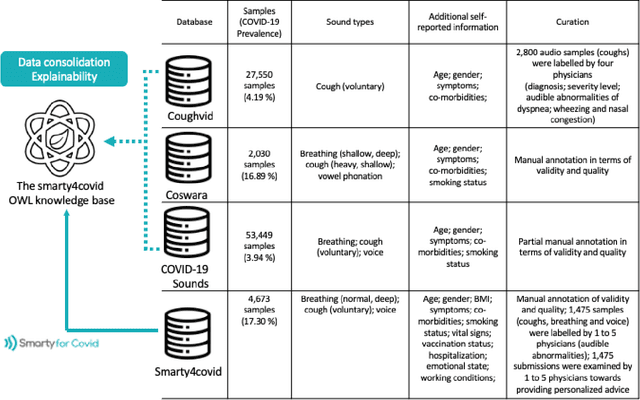

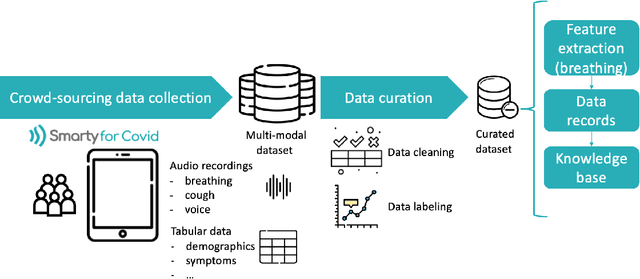
Abstract:Harnessing the power of Artificial Intelligence (AI) and m-health towards detecting new bio-markers indicative of the onset and progress of respiratory abnormalities/conditions has greatly attracted the scientific and research interest especially during COVID-19 pandemic. The smarty4covid dataset contains audio signals of cough (4,676), regular breathing (4,665), deep breathing (4,695) and voice (4,291) as recorded by means of mobile devices following a crowd-sourcing approach. Other self reported information is also included (e.g. COVID-19 virus tests), thus providing a comprehensive dataset for the development of COVID-19 risk detection models. The smarty4covid dataset is released in the form of a web-ontology language (OWL) knowledge base enabling data consolidation from other relevant datasets, complex queries and reasoning. It has been utilized towards the development of models able to: (i) extract clinically informative respiratory indicators from regular breathing records, and (ii) identify cough, breath and voice segments in crowd-sourced audio recordings. A new framework utilizing the smarty4covid OWL knowledge base towards generating counterfactual explanations in opaque AI-based COVID-19 risk detection models is proposed and validated.
An explainable XGBoost-based approach towards assessing the risk of cardiovascular disease in patients with Type 2 Diabetes Mellitus
Sep 14, 2020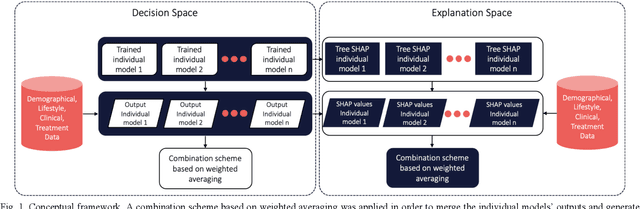
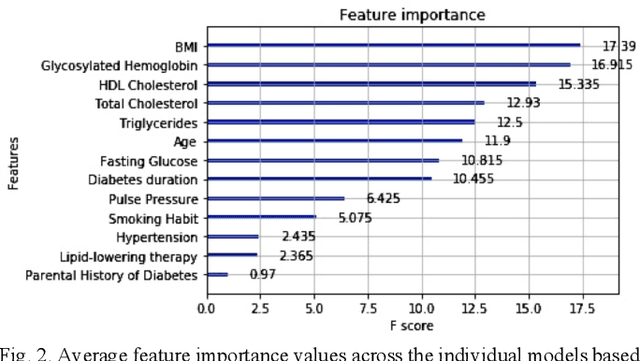
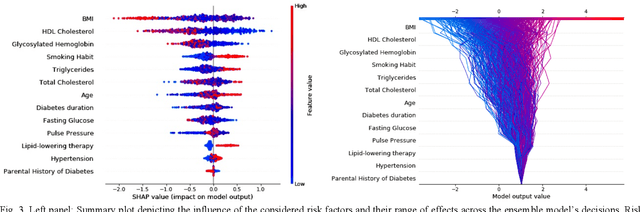
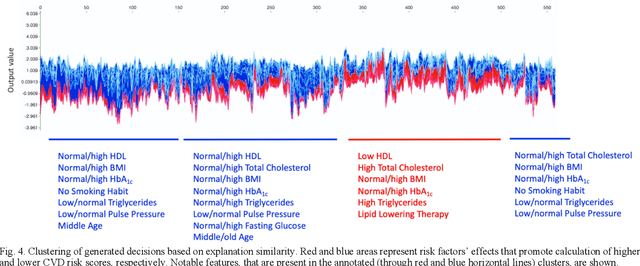
Abstract:Cardiovascular Disease (CVD) is an important cause of disability and death among individuals with Diabetes Mellitus (DM). International clinical guidelines for the management of Type 2 DM (T2DM) are founded on primary and secondary prevention and favor the evaluation of CVD related risk factors towards appropriate treatment initiation. CVD risk prediction models can provide valuable tools for optimizing the frequency of medical visits and performing timely preventive and therapeutic interventions against CVD events. The integration of explainability modalities in these models can enhance human understanding on the reasoning process, maximize transparency and embellish trust towards the models' adoption in clinical practice. The aim of the present study is to develop and evaluate an explainable personalized risk prediction model for the fatal or non-fatal CVD incidence in T2DM individuals. An explainable approach based on the eXtreme Gradient Boosting (XGBoost) and the Tree SHAP (SHapley Additive exPlanations) method is deployed for the calculation of the 5-year CVD risk and the generation of individual explanations on the model's decisions. Data from the 5-year follow up of 560 patients with T2DM are used for development and evaluation purposes. The obtained results (AUC = 71.13%) indicate the potential of the proposed approach to handle the unbalanced nature of the used dataset, while providing clinically meaningful insights about the ensemble model's decision process.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge