Kaylen J Pfisterer
Fully-Automatic Semantic Segmentation for Food Intake Tracking in Long-Term Care Homes
Oct 24, 2019

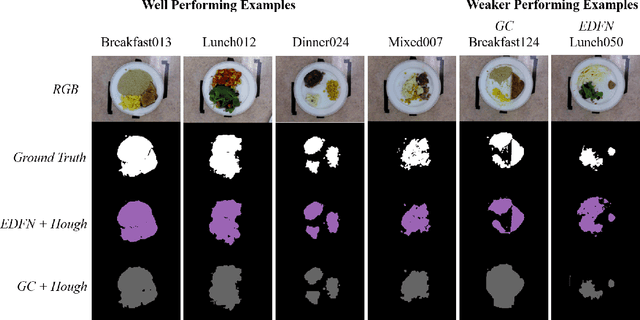
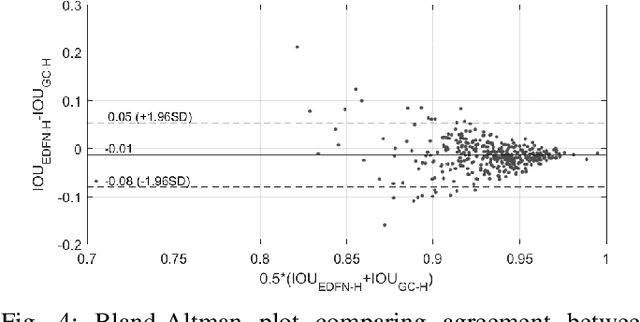
Abstract:Malnutrition impacts quality of life and places annually-recurring burden on the health care system. Half of older adults are at risk for malnutrition in long-term care (LTC). Monitoring and measuring nutritional intake is paramount yet involves time-consuming and subjective visual assessment, limiting current methods' reliability. The opportunity for automatic image-based estimation exists. Some progress outside LTC has been made (e.g., calories consumed, food classification), however, these methods have not been implemented in LTC, potentially due to a lack of ability to independently evaluate automatic segmentation methods within the intake estimation pipeline. Here, we propose and evaluate a novel fully-automatic semantic segmentation method for pixel-level classification of food on a plate using a deep convolutional neural network (DCNN). The macroarchitecture of the DCNN is a multi-scale encoder-decoder food network (EDFN) architecture comprising a residual encoder microarchitecture, a pyramid scene parsing decoder microarchitecture, and a specialized per-pixel food/no-food classification layer. The network was trained and validated on the pre-labelled UNIMIB 2016 food dataset (1027 tray images, 73 categories), and tested on our novel LTC plate dataset (390 plate images, 9 categories). Our fully-automatic segmentation method attained similar intersection over union to the semi-automatic graph cuts (91.2% vs. 93.7%). Advantages of our proposed system include: testing on a novel dataset, decoupled error analysis, no user-initiated annotations, with similar segmentation accuracy and enhanced reliability in terms of types of segmentation errors. This may address several short-comings currently limiting utility of automated food intake tracking in time-constrained LTC and hospital settings.
Non-contact hemodynamic imaging reveals the jugular venous pulse waveform
Apr 21, 2016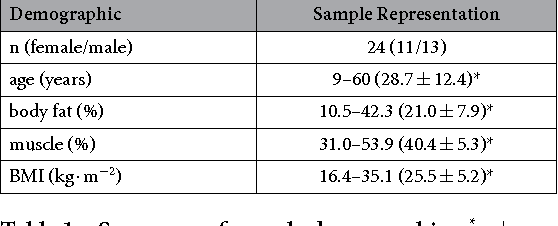
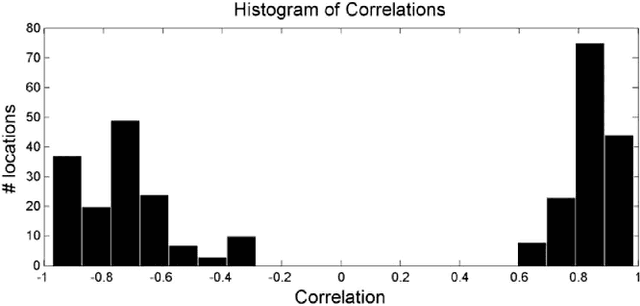
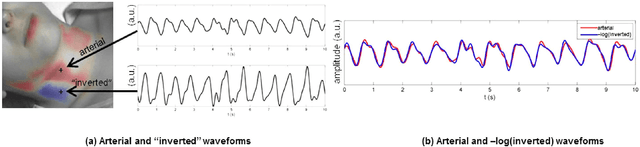
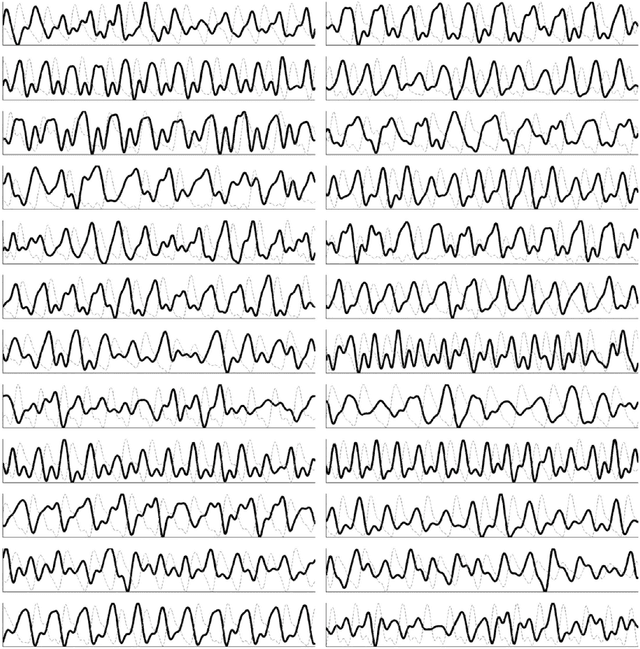
Abstract:Cardiovascular monitoring is important to prevent diseases from progressing. The jugular venous pulse (JVP) waveform offers important clinical information about cardiac health, but is not routinely examined due to its invasive catheterisation procedure. Here, we demonstrate for the first time that the JVP can be consistently observed in a non-contact manner using a novel light-based photoplethysmographic imaging system, coded hemodynamic imaging (CHI). While traditional monitoring methods measure the JVP at a single location, CHI's wide-field imaging capabilities were able to observe the jugular venous pulse's spatial flow profile for the first time. The important inflection points in the JVP were observed, meaning that cardiac abnormalities can be assessed through JVP distortions. CHI provides a new way to assess cardiac health through non-contact light-based JVP monitoring, and can be used in non-surgical environments for cardiac assessment.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge