Richard L Hughson
Temporal prediction of oxygen uptake dynamics from wearable sensors during low-, moderate-, and heavy-intensity exercise
May 20, 2021



Abstract:Oxygen consumption (VO$_2$) provides established clinical and physiological indicators of cardiorespiratory function and exercise capacity. However, VO$_2$ monitoring is largely limited to specialized laboratory settings, making its widespread monitoring elusive. Here, we investigate temporal prediction of VO$_2$ from wearable sensors during cycle ergometer exercise using a temporal convolutional network (TCN). Cardiorespiratory signals were acquired from a smart shirt with integrated textile sensors alongside ground-truth VO$_2$ from a metabolic system on twenty-two young healthy adults. Participants performed one ramp-incremental and three pseudorandom binary sequence exercise protocols to assess a range of VO$_2$ dynamics. A TCN model was developed using causal convolutions across an effective history length to model the time-dependent nature of VO$_2$. Optimal history length was determined through minimum validation loss across hyperparameter values. The best performing model encoded 218 s history length (TCN-VO$_2$ A), with 187 s, 97 s, and 76 s yielding less than 3% deviation from the optimal validation loss. TCN-VO$_2$ A showed strong prediction accuracy (mean, 95% CI) across all exercise intensities (-22 ml.min$^{-1}$, [-262, 218]), spanning transitions from low-moderate (-23 ml.min$^{-1}$, [-250, 204]), low-heavy (14 ml.min$^{-1}$, [-252, 280]), ventilatory threshold-heavy (-49 ml.min$^{-1}$, [-274, 176]), and maximal (-32 ml.min$^{-1}$, [-261, 197]) exercise. Second-by-second classification of physical activity across 16090 s of predicted VO$_2$ was able to discern between vigorous, moderate, and light activity with high accuracy (94.1%). This system enables quantitative aerobic activity monitoring in non-laboratory settings across a range of exercise intensities using wearable sensors for monitoring exercise prescription adherence and personal fitness.
Assessing postural instability during cerebral hypoperfusion using sub-millimeter monocular 3D sway tracking
Jul 11, 2019



Abstract:Postural instability is prevalent in aging and neurodegenerative disease, decreasing quality of life and independence. Quantitatively monitoring balance control is important for assessing treatment efficacy and rehabilitation progress. However, existing technologies for assessing postural sway are complex and expensive, limiting their widespread utility. Here, we propose a monocular imaging system capable of assessing sub-millimeter 3D sway dynamics. By physically embedding anatomical targets with known \textit{a priori} geometric models, 3D central and upper body kinematic motion was automatically assessed through geometric feature tracking and 3D kinematic motion inverse estimation from a set of 2D frames. Sway was tracked in 3D and compared between control and hypoperfusion conditions. The proposed system demonstrated high agreement with a commercial motion capture system (error $4.4 \times 10^{-16} \pm 0.30$~mm, $r^2=0.9773$). Significant differences in sway dynamics were observed in early stance central anterior-posterior sway (control: $147.1 \pm 7.43$~mm, hypoperfusion: $177.8 \pm 15.3$~mm; $p=0.039$) and mid stance upper body coronal sway (control: $106.3 \pm 5.80$~mm, hypoperfusion: $128.1 \pm 18.4$~mm; $p=0.040$) commensurate with cerebral blood flow (CBF) perfusion deficit, followed by recovered sway dynamics during late stance governed by CBF recovery. This inexpensive single-camera system enables quantitative 3D sway monitoring for assessing neuromuscular balance control in weakly constrained environments.
Non-contact hemodynamic imaging reveals the jugular venous pulse waveform
Apr 21, 2016
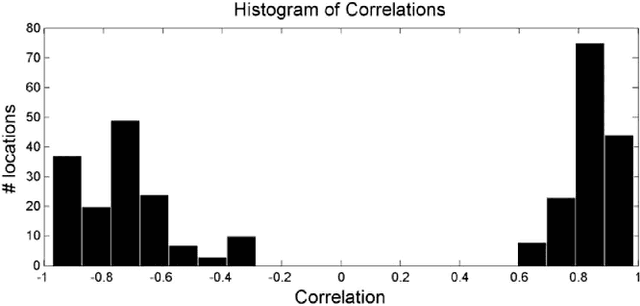
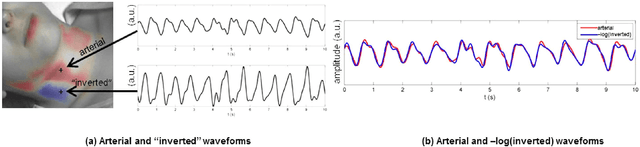
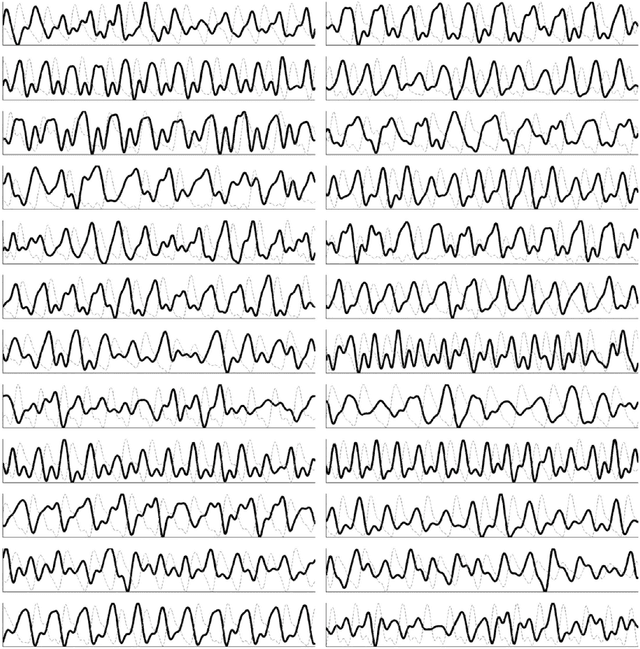
Abstract:Cardiovascular monitoring is important to prevent diseases from progressing. The jugular venous pulse (JVP) waveform offers important clinical information about cardiac health, but is not routinely examined due to its invasive catheterisation procedure. Here, we demonstrate for the first time that the JVP can be consistently observed in a non-contact manner using a novel light-based photoplethysmographic imaging system, coded hemodynamic imaging (CHI). While traditional monitoring methods measure the JVP at a single location, CHI's wide-field imaging capabilities were able to observe the jugular venous pulse's spatial flow profile for the first time. The important inflection points in the JVP were observed, meaning that cardiac abnormalities can be assessed through JVP distortions. CHI provides a new way to assess cardiac health through non-contact light-based JVP monitoring, and can be used in non-surgical environments for cardiac assessment.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge