Jeng Wei
Representation Learning of Structured Data for Medical Foundation Models
Oct 17, 2024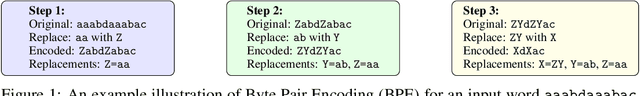
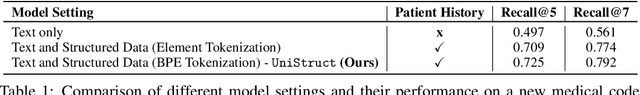
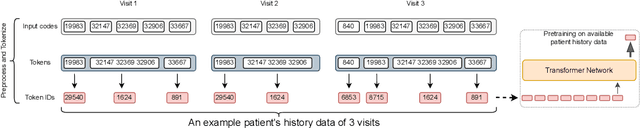
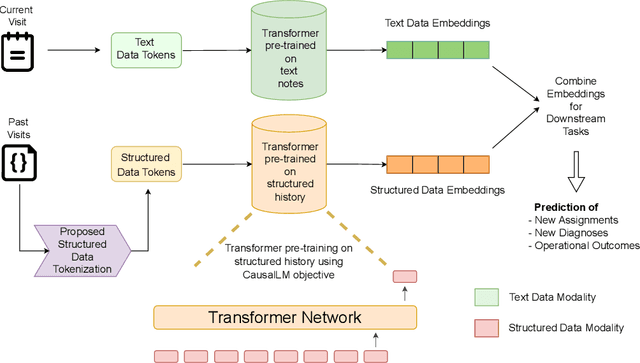
Abstract:Large Language Models (LLMs) have demonstrated remarkable performance across various domains, including healthcare. However, their ability to effectively represent structured non-textual data, such as the alphanumeric medical codes used in records like ICD-10 or SNOMED-CT, is limited and has been particularly exposed in recent research. This paper examines the challenges LLMs face in processing medical codes due to the shortcomings of current tokenization methods. As a result, we introduce the UniStruct architecture to design a multimodal medical foundation model of unstructured text and structured data, which addresses these challenges by adapting subword tokenization techniques specifically for the structured medical codes. Our approach is validated through model pre-training on both an extensive internal medical database and a public repository of structured medical records. Trained on over 1 billion tokens on the internal medical database, the proposed model achieves up to a 23% improvement in evaluation metrics, with around 2% gain attributed to our proposed tokenization. Additionally, when evaluated on the EHRSHOT public benchmark with a 1/1000 fraction of the pre-training data, the UniStruct model improves performance on over 42% of the downstream tasks. Our approach not only enhances the representation and generalization capabilities of patient-centric models but also bridges a critical gap in representation learning models' ability to handle complex structured medical data, alongside unstructured text.
Automated Clinical Coding for Outpatient Departments
Dec 24, 2023Abstract:Computerised clinical coding approaches aim to automate the process of assigning a set of codes to medical records. While there is active research pushing the state of the art on clinical coding for hospitalized patients, the outpatient setting -- where doctors tend to non-hospitalised patients -- is overlooked. Although both settings can be formalised as a multi-label classification task, they present unique and distinct challenges, which raises the question of whether the success of inpatient clinical coding approaches translates to the outpatient setting. This paper is the first to investigate how well state-of-the-art deep learning-based clinical coding approaches work in the outpatient setting at hospital scale. To this end, we collect a large outpatient dataset comprising over 7 million notes documenting over half a million patients. We adapt four state-of-the-art clinical coding approaches to this setting and evaluate their potential to assist coders. We find evidence that clinical coding in outpatient settings can benefit from more innovations in popular inpatient coding benchmarks. A deeper analysis of the factors contributing to the success -- amount and form of data and choice of document representation -- reveals the presence of easy-to-solve examples, the coding of which can be completely automated with a low error rate.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge