Desen Cao
Interpretable Machine Learning Model for Early Prediction of Mortality in Elderly Patients with Multiple Organ Dysfunction Syndrome (MODS): a Multicenter Retrospective Study and Cross Validation
Jan 28, 2020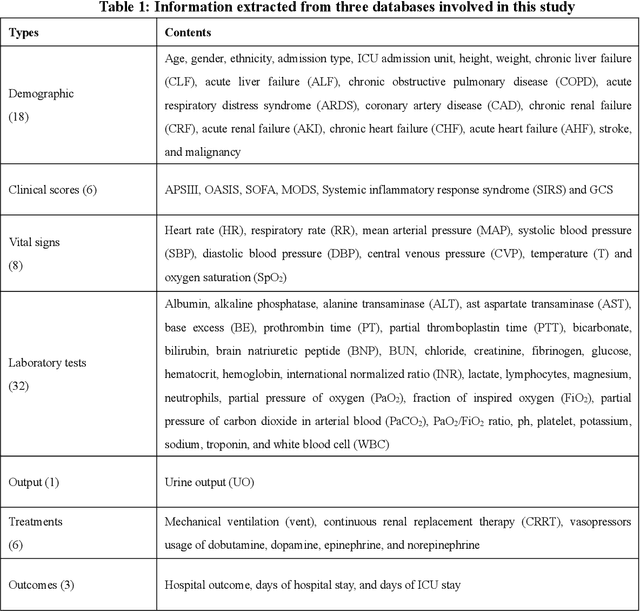
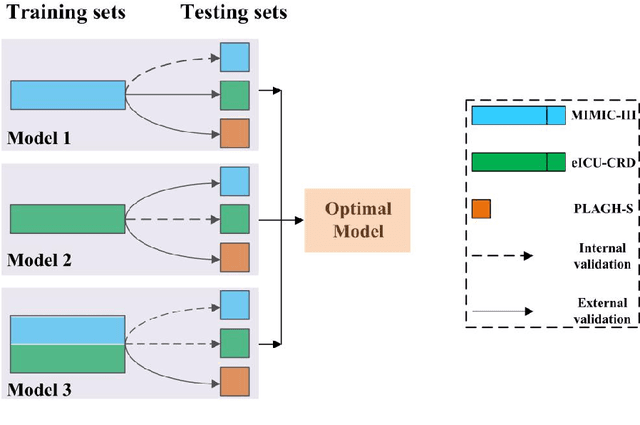
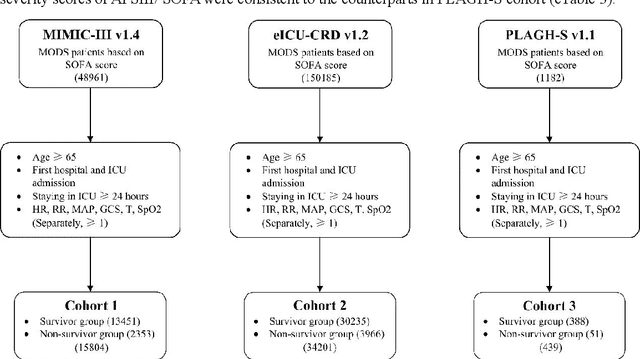
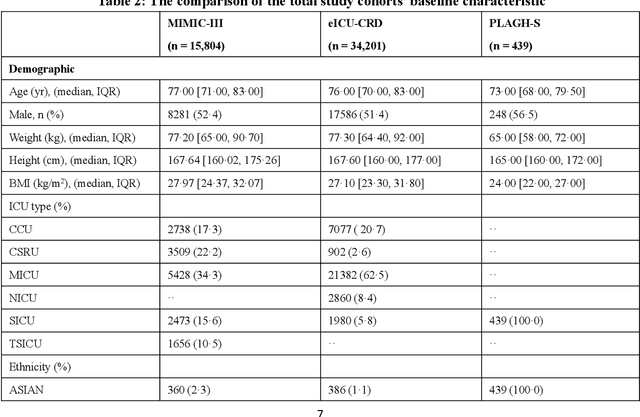
Abstract:Background: Elderly patients with MODS have high risk of death and poor prognosis. The performance of current scoring systems assessing the severity of MODS and its mortality remains unsatisfactory. This study aims to develop an interpretable and generalizable model for early mortality prediction in elderly patients with MODS. Methods: The MIMIC-III, eICU-CRD and PLAGH-S databases were employed for model generation and evaluation. We used the eXtreme Gradient Boosting model with the SHapley Additive exPlanations method to conduct early and interpretable predictions of patients' hospital outcome. Three types of data source combinations and five typical evaluation indexes were adopted to develop a generalizable model. Findings: The interpretable model, with optimal performance developed by using MIMIC-III and eICU-CRD datasets, was separately validated in MIMIC-III, eICU-CRD and PLAGH-S datasets (no overlapping with training set). The performances of the model in predicting hospital mortality as validated by the three datasets were: AUC of 0.858, sensitivity of 0.834 and specificity of 0.705; AUC of 0.849, sensitivity of 0.763 and specificity of 0.784; and AUC of 0.838, sensitivity of 0.882 and specificity of 0.691, respectively. Comparisons of AUC between this model and baseline models with MIMIC-III dataset validation showed superior performances of this model; In addition, comparisons in AUC between this model and commonly used clinical scores showed significantly better performance of this model. Interpretation: The interpretable machine learning model developed in this study using fused datasets with large sample sizes was robust and generalizable. This model outperformed the baseline models and several clinical scores for early prediction of mortality in elderly ICU patients. The interpretative nature of this model provided clinicians with the ranking of mortality risk features.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge