David Shin
Clinical Applications of Plantar Pressure Measurement
Jan 09, 2024Abstract:Plantar pressure measurements can provide valuable insight into various health characteristics in patients. In this study, we describe different plantar pressure devices available on the market and their clinical relevance. Current devices are either platform-based or wearable and consist of a variety of sensor technologies: resistive, capacitive, piezoelectric, and optical. The measurements collected from any of these sensors can be utilized for a range of clinical applications including patients with diabetes, trauma, deformity and cerebral palsy, stroke, cervical myelopathy, ankle instability, sports injuries, and Parkinsons disease. However, the proper technology should be selected based on the clinical need and the type of tests being performed on the device. In this review we provide the reader with a simple overview of the existing technologies their advantages and disadvantages and provide application examples for each. Moreover, we suggest new areas in orthopaedic that plantar pressure mapping technology can be utilized for increased quality of care.
The Required Spatial Resolution to Assess Imbalance using Plantar Pressure Mapping
Jan 08, 2024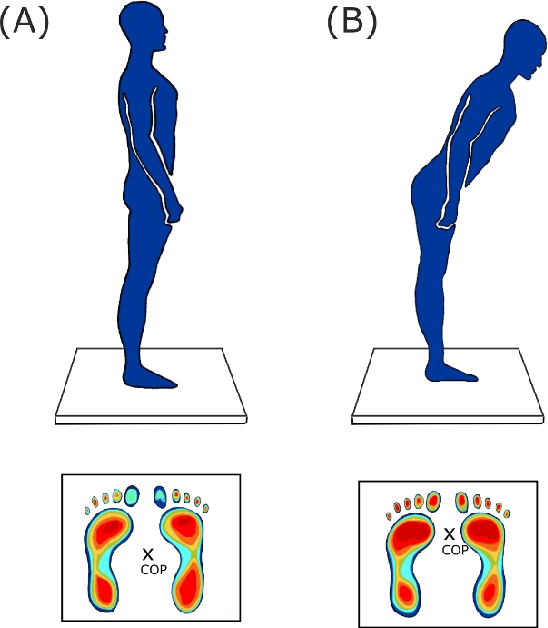
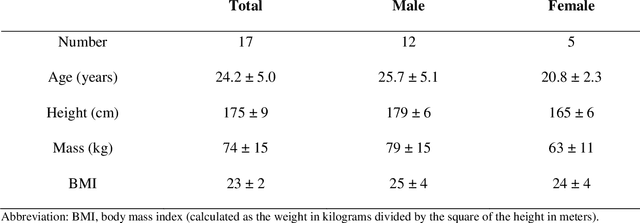
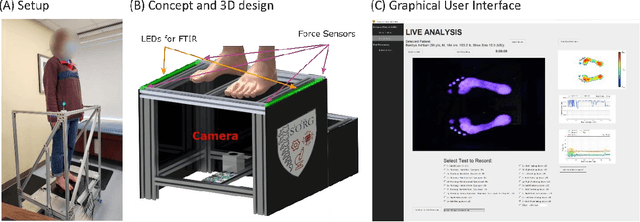
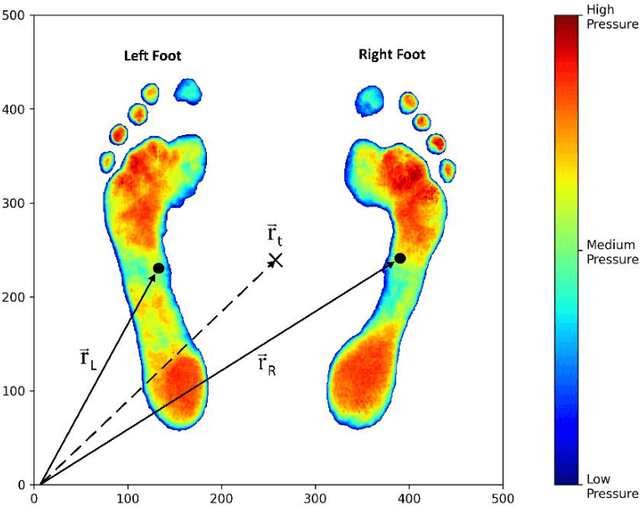
Abstract:Roughly 1/3 of adults older than 65 fall each year, resulting in more than 3 million emergency room visits, thousands of deaths, and over $50 Billion in direct costs. The Centers for Disease Control and Prevention (CDC) estimate that 1/3 of falls are preventable with effective mitigation strategies, particularly for imbalance. Therefore, quantification of imbalance is being studied extensively in recent years. In this study we investigate the feasibility of plantar pressure mapping in balance assessment through a healthy human subject study. We used an in-house plantar pressure mapping device with high precision based on Frustrated Total Internal Reflection to measure subjects sway during the Romberg test. Through the measurements obtained from all subjects, we measured the minimum spatial resolution required for plantar pressure mapping devices in assessment of balance. We conclude that most of the current devices in the market lack the requirements for imbalance measurements.
Brain MRI-to-PET Synthesis using 3D Convolutional Attention Networks
Nov 22, 2022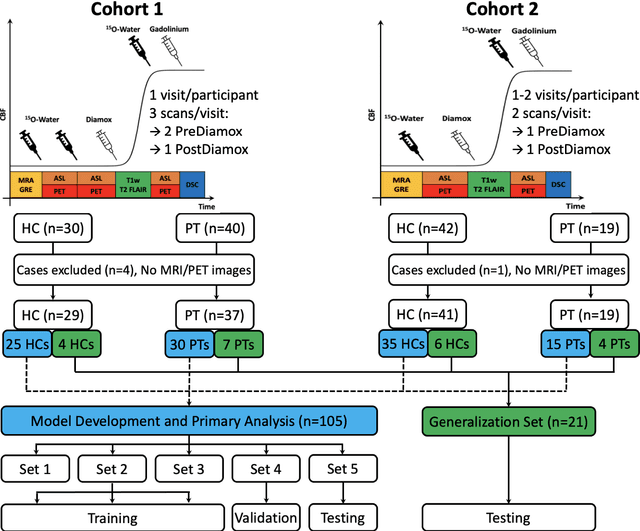
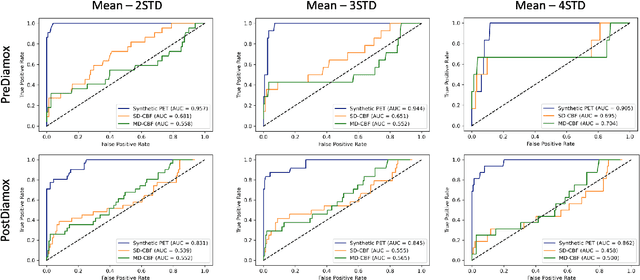
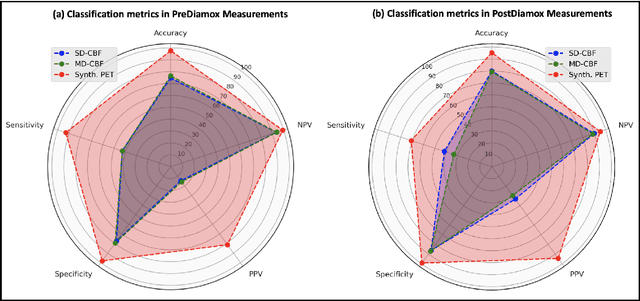
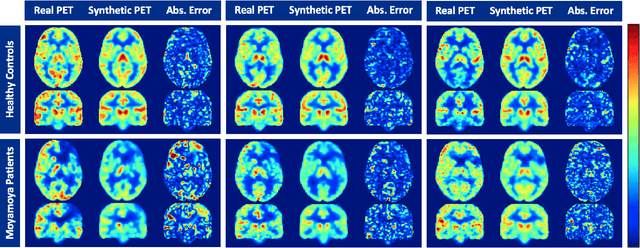
Abstract:Accurate quantification of cerebral blood flow (CBF) is essential for the diagnosis and assessment of a wide range of neurological diseases. Positron emission tomography (PET) with radiolabeled water (15O-water) is considered the gold-standard for the measurement of CBF in humans. PET imaging, however, is not widely available because of its prohibitive costs and use of short-lived radiopharmaceutical tracers that typically require onsite cyclotron production. Magnetic resonance imaging (MRI), in contrast, is more readily accessible and does not involve ionizing radiation. This study presents a convolutional encoder-decoder network with attention mechanisms to predict gold-standard 15O-water PET CBF from multi-sequence MRI scans, thereby eliminating the need for radioactive tracers. Inputs to the prediction model include several commonly used MRI sequences (T1-weighted, T2-FLAIR, and arterial spin labeling). The model was trained and validated using 5-fold cross-validation in a group of 126 subjects consisting of healthy controls and cerebrovascular disease patients, all of whom underwent simultaneous $15O-water PET/MRI. The results show that such a model can successfully synthesize high-quality PET CBF measurements (with an average SSIM of 0.924 and PSNR of 38.8 dB) and is more accurate compared to concurrent and previous PET synthesis methods. We also demonstrate the clinical significance of the proposed algorithm by evaluating the agreement for identifying the vascular territories with abnormally low CBF. Such methods may enable more widespread and accurate CBF evaluation in larger cohorts who cannot undergo PET imaging due to radiation concerns, lack of access, or logistic challenges.
Multi-task Deep Learning for Cerebrovascular Disease Classification and MRI-to-PET Translation
Feb 12, 2022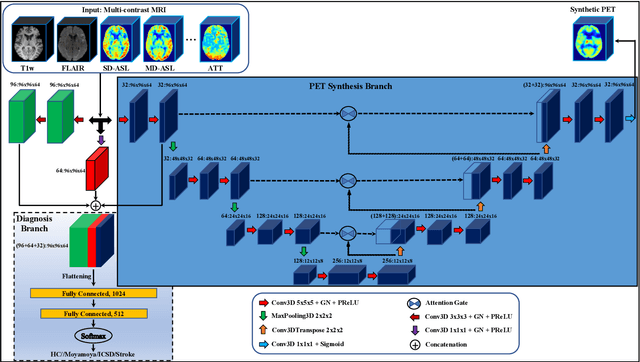
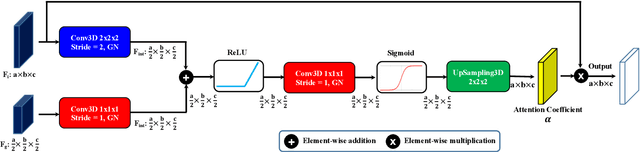
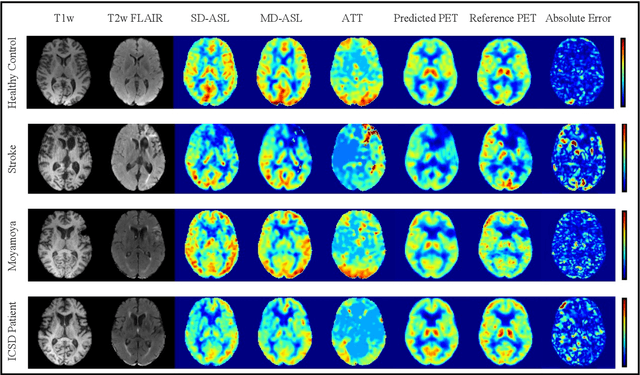
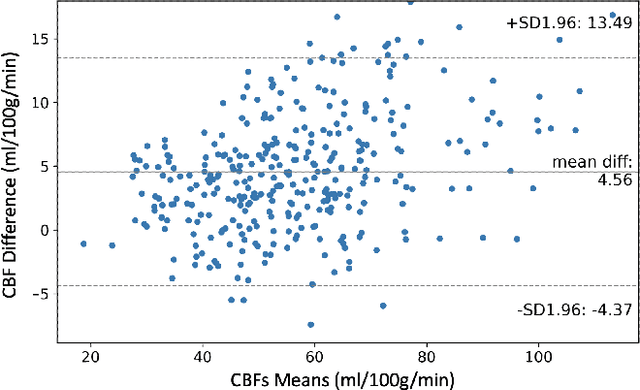
Abstract:Accurate quantification of cerebral blood flow (CBF) is essential for the diagnosis and assessment of cerebrovascular diseases such as Moyamoya, carotid stenosis, aneurysms, and stroke. Positron emission tomography (PET) is currently regarded as the gold standard for the measurement of CBF in the human brain. PET imaging, however, is not widely available because of its prohibitive costs, use of ionizing radiation, and logistical challenges, which require a co-localized cyclotron to deliver the 2 min half-life Oxygen-15 radioisotope. Magnetic resonance imaging (MRI), in contrast, is more readily available and does not involve ionizing radiation. In this study, we propose a multi-task learning framework for brain MRI-to-PET translation and disease diagnosis. The proposed framework comprises two prime networks: (1) an attention-based 3D encoder-decoder convolutional neural network (CNN) that synthesizes high-quality PET CBF maps from multi-contrast MRI images, and (2) a multi-scale 3D CNN that identifies the brain disease corresponding to the input MRI images. Our multi-task framework yields promising results on the task of MRI-to-PET translation, achieving an average structural similarity index (SSIM) of 0.94 and peak signal-to-noise ratio (PSNR) of 38dB on a cohort of 120 subjects. In addition, we show that integrating multiple MRI modalities can improve the clinical diagnosis of brain diseases.
Natural Language Processing with Deep Learning for Medical Adverse Event Detection from Free-Text Medical Narratives: A Case Study of Detecting Total Hip Replacement Dislocation
Apr 26, 2020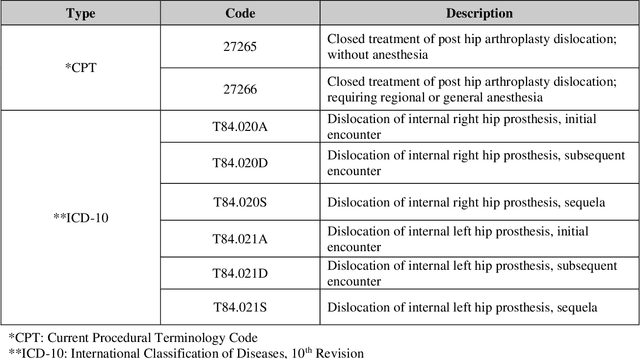
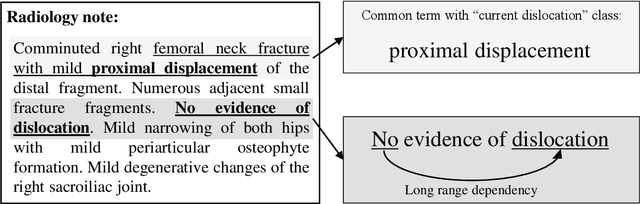
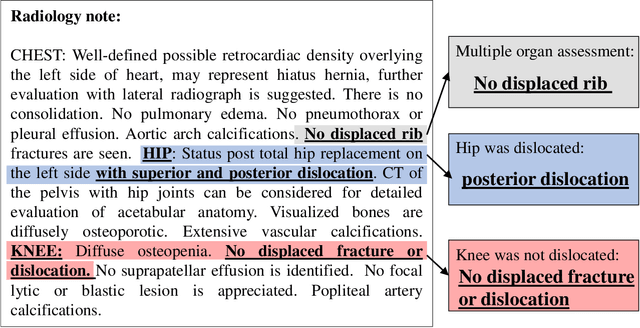
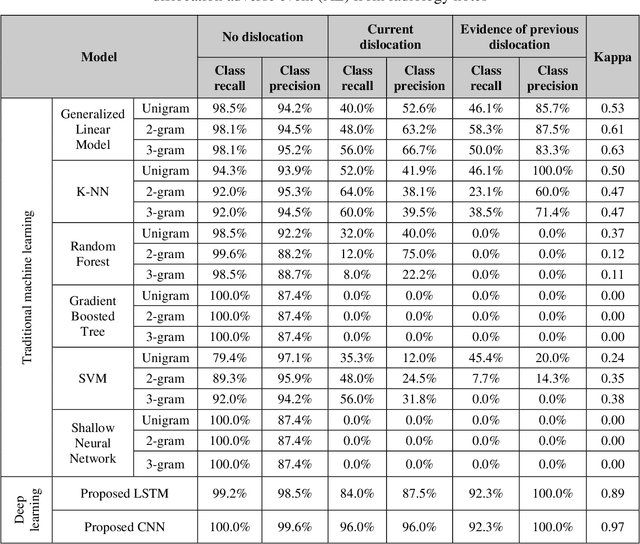
Abstract:Accurate and timely detection of medical adverse events (AEs) from free-text medical narratives is challenging. Natural language processing (NLP) with deep learning has already shown great potential for analyzing free-text data, but its application for medical AE detection has been limited. In this study we proposed deep learning based NLP (DL-NLP) models for efficient and accurate hip dislocation AE detection following total hip replacement from standard (radiology notes) and non-standard (follow-up telephone notes) free-text medical narratives. We benchmarked these proposed models with a wide variety of traditional machine learning based NLP (ML-NLP) models, and also assessed the accuracy of International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes in capturing these hip dislocation AEs in a multi-center orthopaedic registry. All DL-NLP models out-performed all of the ML-NLP models, with a convolutional neural network (CNN) model achieving the best overall performance (Kappa = 0.97 for radiology notes, and Kappa = 1.00 for follow-up telephone notes). On the other hand, the ICD/CPT codes of the patients who sustained a hip dislocation AE were only 75.24% accurate, showing the potential of the proposed model to be used in largescale orthopaedic registries for accurate and efficient hip dislocation AE detection to improve the quality of care and patient outcome.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge