Cameron Carlin
The Impact of Extraneous Variables on the Performance of Recurrent Neural Network Models in Clinical Tasks
Apr 01, 2019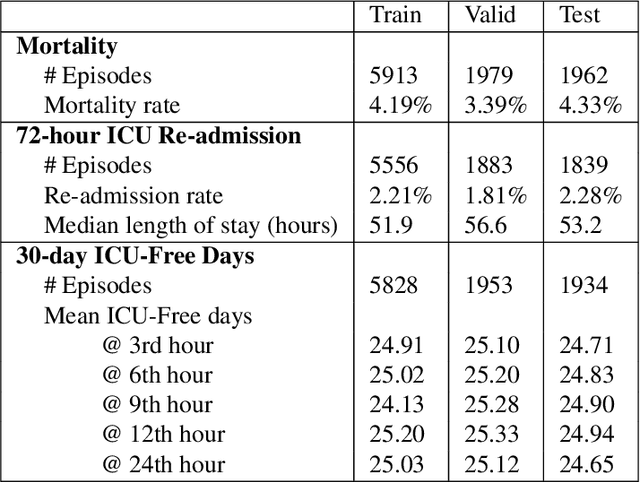
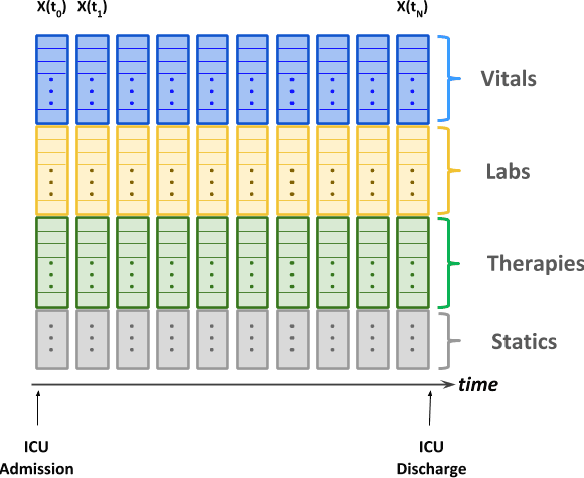
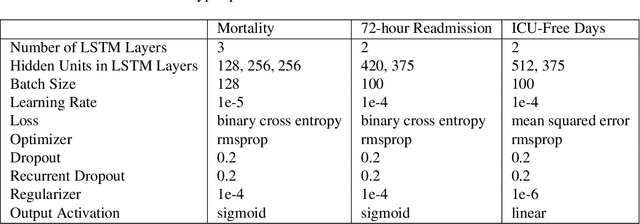
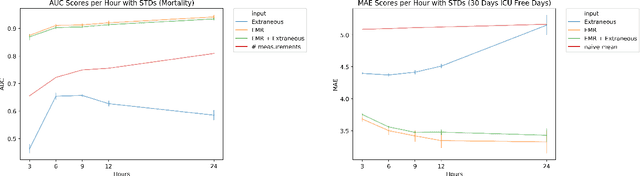
Abstract:Electronic Medical Records (EMR) are a rich source of patient information, including measurements reflecting physiologic signs and administered therapies. Identifying which variables are useful in predicting clinical outcomes can be challenging. Advanced algorithms such as deep neural networks were designed to process high-dimensional inputs containing variables in their measured form, thus bypass separate feature selection or engineering steps. We investigated the effect of extraneous input variables on the predictive performance of Recurrent Neural Networks (RNN) by including in the input vector extraneous variables randomly drawn from theoretical and empirical distributions. RNN models using different input vectors (EMR variables; EMR and extraneous variables; extraneous variables only) were trained to predict three clinical outcomes: in-ICU mortality, 72-hour ICU re-admission, and 30-day ICU-free days. The measured degradations of the RNN's predictive performance with the addition of extraneous variables to EMR variables were negligible.
Predicting Individual Responses to Vasoactive Medications in Children with Septic Shock
Jan 15, 2019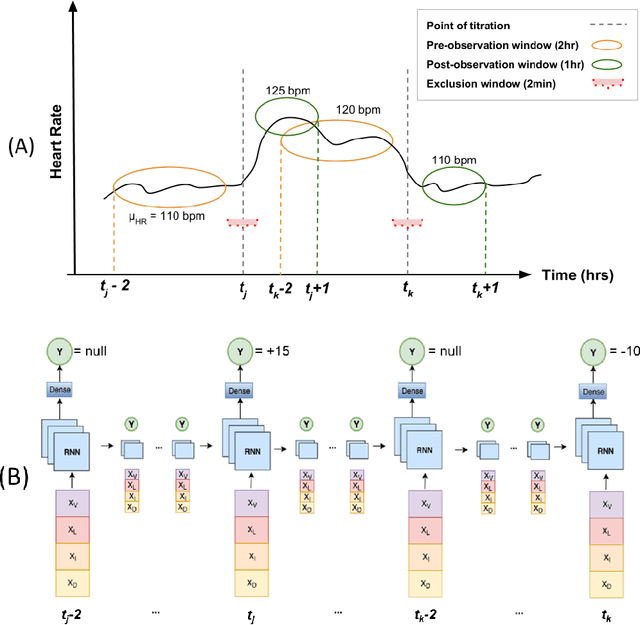
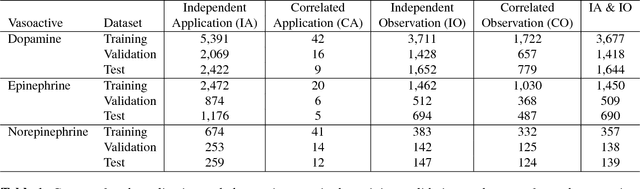
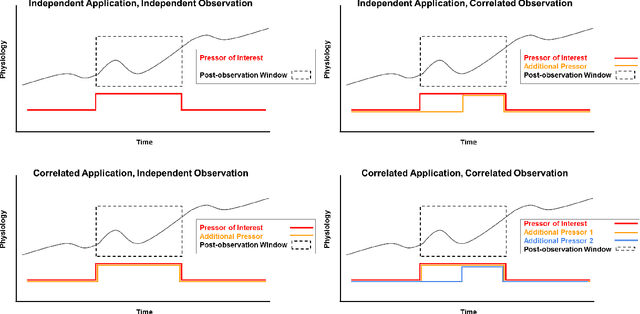
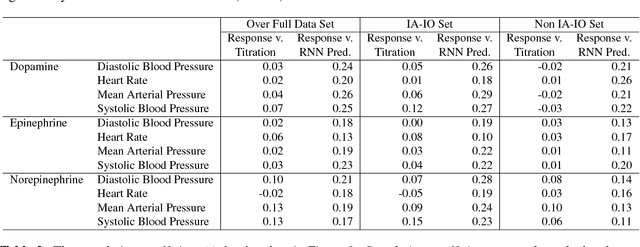
Abstract:Objective: Predict individual septic children's personalized physiologic responses to vasoactive titrations by training a Recurrent Neural Network (RNN) using EMR data. Materials and Methods: This study retrospectively analyzed EMR of patients admitted to a pediatric ICU from 2009 to 2017. Data included charted time series vitals, labs, drugs, and interventions of children with septic shock treated with dopamine, epinephrine, or norepinephrine. A RNN was trained to predict responses in heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) to 8,640 titrations during 652 septic episodes and evaluated on a holdout set of 3,883 titrations during 254 episodes. A linear regression model using titration data as its sole input was also developed and compared to the RNN model. Evaluation methods included the correlation coefficient between actual physiologic responses and RNN predictions, mean absolute error (MAE), and area under the receiver operating characteristic curve (AUC). Results: The actual physiologic responses displayed significant variability and were more accurately predicted by the RNN model than by titration alone (r=0.20 vs r=0.05, p<0.01). The RNN showed MAE and AUC improvements over the linear model. The RNN's MAEs associated with dopamine and epinephrine were 1-3% lower than the linear regression model MAE for HR, SBP, DBP, and MAP. Across all vitals vasoactives, the RNN achieved 1-19% AUC improvement over the linear model. Conclusion: This initial attempt in pediatric critical care to predict individual physiologic responses to vasoactive dose changes in children with septic shock demonstrated an RNN model showed some improvement over a linear model. While not yet clinically applicable, further development may assist clinical administration of vasoactive medications in children with septic shock.
Predicting Individual Physiologically Acceptable States for Discharge from a Pediatric Intensive Care Unit
Dec 18, 2017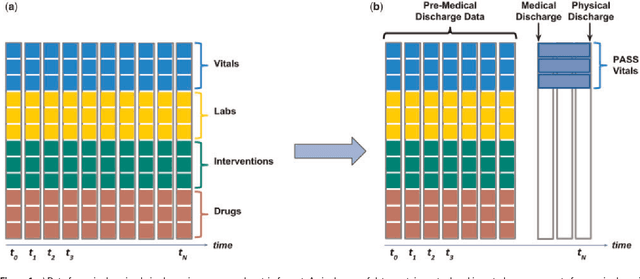
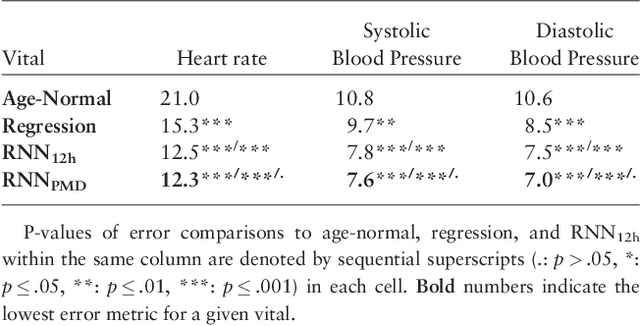
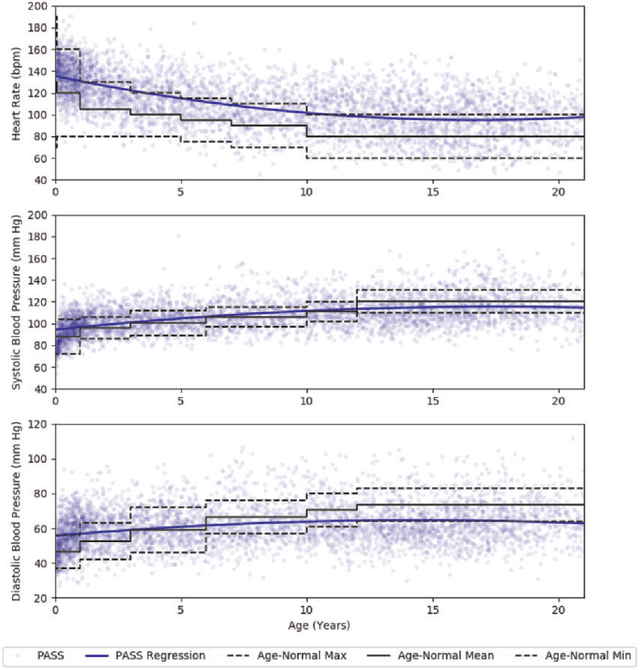
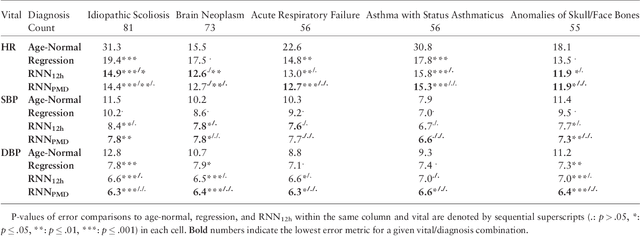
Abstract:Objective: Predict patient-specific vitals deemed medically acceptable for discharge from a pediatric intensive care unit (ICU). Design: The means of each patient's hr, sbp and dbp measurements between their medical and physical discharge from the ICU were computed as a proxy for their physiologically acceptable state space (PASS) for successful ICU discharge. These individual PASS values were compared via root mean squared error (rMSE) to population age-normal vitals, a polynomial regression through the PASS values of a Pediatric ICU (PICU) population and predictions from two recurrent neural network models designed to predict personalized PASS within the first twelve hours following ICU admission. Setting: PICU at Children's Hospital Los Angeles (CHLA). Patients: 6,899 PICU episodes (5,464 patients) collected between 2009 and 2016. Interventions: None. Measurements: Each episode data contained 375 variables representing vitals, labs, interventions, and drugs. They also included a time indicator for PICU medical discharge and physical discharge. Main Results: The rMSEs between individual PASS values and population age-normals (hr: 25.9 bpm, sbp: 13.4 mmHg, dbp: 13.0 mmHg) were larger than the rMSEs corresponding to the polynomial regression (hr: 19.1 bpm, sbp: 12.3 mmHg, dbp: 10.8 mmHg). The rMSEs from the best performing RNN model were the lowest (hr: 16.4 bpm; sbp: 9.9 mmHg, dbp: 9.0 mmHg). Conclusion: PICU patients are a unique subset of the general population, and general age-normal vitals may not be suitable as target values indicating physiologic stability at discharge. Age-normal vitals that were specifically derived from the medical-to-physical discharge window of ICU patients may be more appropriate targets for 'acceptable' physiologic state for critical care patients. Going beyond simple age bins, an RNN model can provide more personalized target values.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge