Predicting Individual Physiologically Acceptable States for Discharge from a Pediatric Intensive Care Unit
Paper and Code
Dec 18, 2017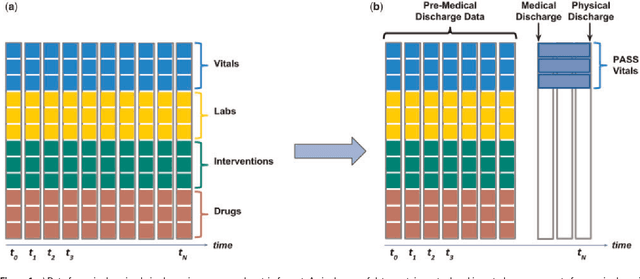
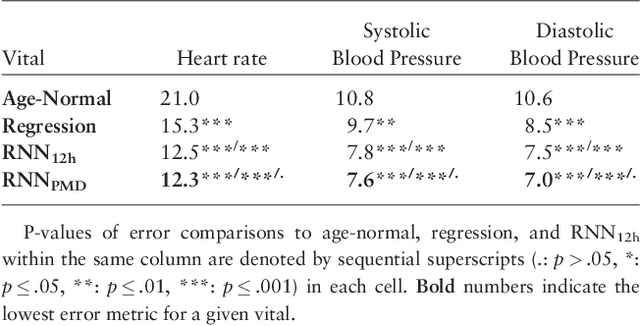
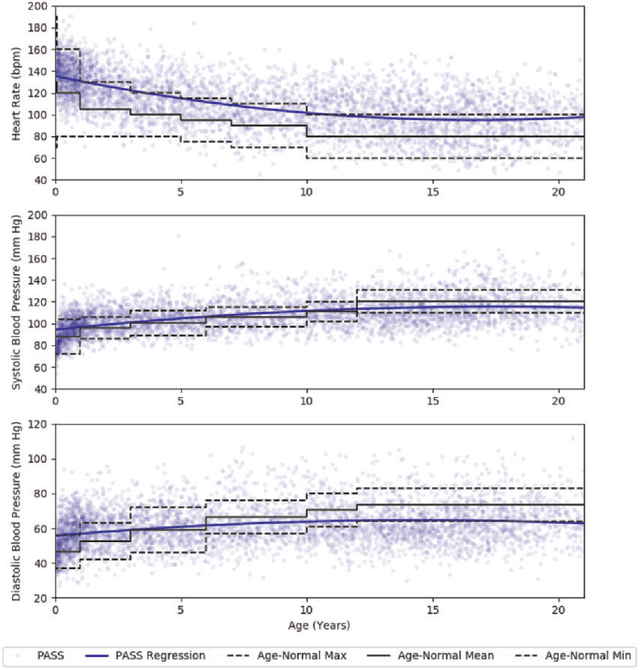
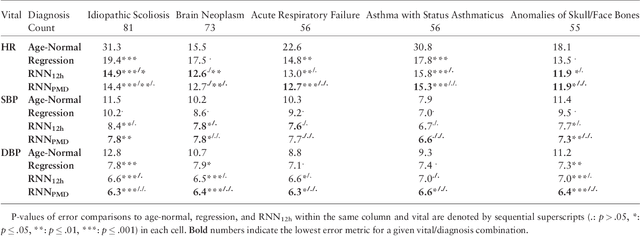
Objective: Predict patient-specific vitals deemed medically acceptable for discharge from a pediatric intensive care unit (ICU). Design: The means of each patient's hr, sbp and dbp measurements between their medical and physical discharge from the ICU were computed as a proxy for their physiologically acceptable state space (PASS) for successful ICU discharge. These individual PASS values were compared via root mean squared error (rMSE) to population age-normal vitals, a polynomial regression through the PASS values of a Pediatric ICU (PICU) population and predictions from two recurrent neural network models designed to predict personalized PASS within the first twelve hours following ICU admission. Setting: PICU at Children's Hospital Los Angeles (CHLA). Patients: 6,899 PICU episodes (5,464 patients) collected between 2009 and 2016. Interventions: None. Measurements: Each episode data contained 375 variables representing vitals, labs, interventions, and drugs. They also included a time indicator for PICU medical discharge and physical discharge. Main Results: The rMSEs between individual PASS values and population age-normals (hr: 25.9 bpm, sbp: 13.4 mmHg, dbp: 13.0 mmHg) were larger than the rMSEs corresponding to the polynomial regression (hr: 19.1 bpm, sbp: 12.3 mmHg, dbp: 10.8 mmHg). The rMSEs from the best performing RNN model were the lowest (hr: 16.4 bpm; sbp: 9.9 mmHg, dbp: 9.0 mmHg). Conclusion: PICU patients are a unique subset of the general population, and general age-normal vitals may not be suitable as target values indicating physiologic stability at discharge. Age-normal vitals that were specifically derived from the medical-to-physical discharge window of ICU patients may be more appropriate targets for 'acceptable' physiologic state for critical care patients. Going beyond simple age bins, an RNN model can provide more personalized target values.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge