Predicting Individual Responses to Vasoactive Medications in Children with Septic Shock
Paper and Code
Jan 15, 2019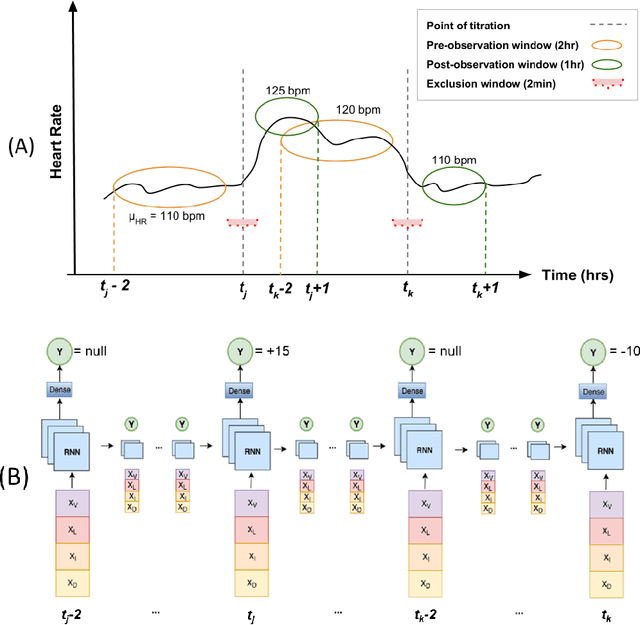
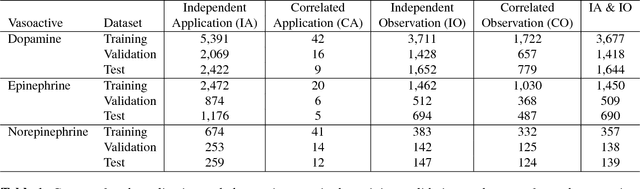
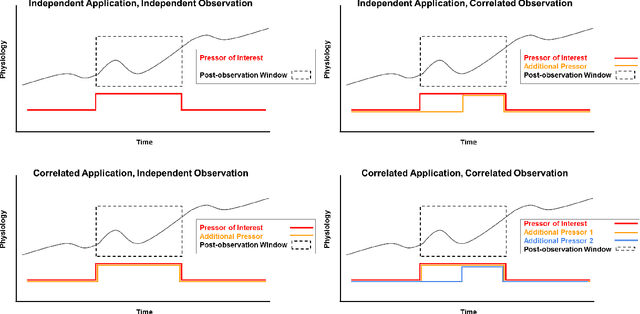
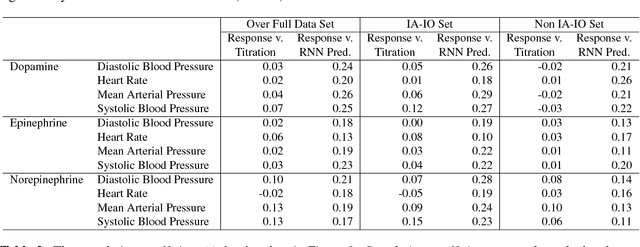
Objective: Predict individual septic children's personalized physiologic responses to vasoactive titrations by training a Recurrent Neural Network (RNN) using EMR data. Materials and Methods: This study retrospectively analyzed EMR of patients admitted to a pediatric ICU from 2009 to 2017. Data included charted time series vitals, labs, drugs, and interventions of children with septic shock treated with dopamine, epinephrine, or norepinephrine. A RNN was trained to predict responses in heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) to 8,640 titrations during 652 septic episodes and evaluated on a holdout set of 3,883 titrations during 254 episodes. A linear regression model using titration data as its sole input was also developed and compared to the RNN model. Evaluation methods included the correlation coefficient between actual physiologic responses and RNN predictions, mean absolute error (MAE), and area under the receiver operating characteristic curve (AUC). Results: The actual physiologic responses displayed significant variability and were more accurately predicted by the RNN model than by titration alone (r=0.20 vs r=0.05, p<0.01). The RNN showed MAE and AUC improvements over the linear model. The RNN's MAEs associated with dopamine and epinephrine were 1-3% lower than the linear regression model MAE for HR, SBP, DBP, and MAP. Across all vitals vasoactives, the RNN achieved 1-19% AUC improvement over the linear model. Conclusion: This initial attempt in pediatric critical care to predict individual physiologic responses to vasoactive dose changes in children with septic shock demonstrated an RNN model showed some improvement over a linear model. While not yet clinically applicable, further development may assist clinical administration of vasoactive medications in children with septic shock.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge